Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Sarcomas of the bone are relatively rare neoplasms with an estimated 2890 new cases in the United States in 2012 [ ]. Because of the rarity of primary bone sarcomas and interpretive uncertainty, management may be delayed from initial misdiagnosis [ ]. After biopsy, pathologic diagnosis may be confounding with disagreements in interpretation among pathologists [ ]. Therefore the best approach to diagnose and treat primary bone sarcomas is through an interdisciplinary team approach, as the roles of the radiologist and pathologist are complementary in reaching an accurate diagnosis.
In addition to helping in diagnosis, imaging studies are critical for staging and influencing management. Current recommendations from the European Society of Medical Oncology for evaluation and staging of primary bone sarcomas include obtaining 2-view radiographs of the primary sarcoma, a magnetic resonance imaging (MRI) of the entire bone involved and the adjacent joints, chest radiograph and CT to assess for pulmonary metastases, and bone scintigraphy to evaluate for osseous metastases [ ].
The purpose of this chapter is to further discuss the utility of a multimodality imaging approach for diagnosis, staging, and follow-up of primary bone sarcomas, followed by a discussion of pertinent imaging characteristics and diagnostic considerations of the more common specific tumor types.
Patients with primary bone sarcomas often present with pain or an enlarging mass prompting their clinicians to obtain the ubiquitous radiograph [ ].
When evaluating the radiograph, the two most important pieces of information to the interpreting radiologist are the patients' age and location of the tumor. These two pieces of information alone are often adequate to provide a narrow, accurate differential diagnosis the majority of the time. In fact, the late famed skeletal radiologist Jack Edeiken showed that simply based on age alone, approximately 80% of bone tumors could be correctly diagnosed [ ].
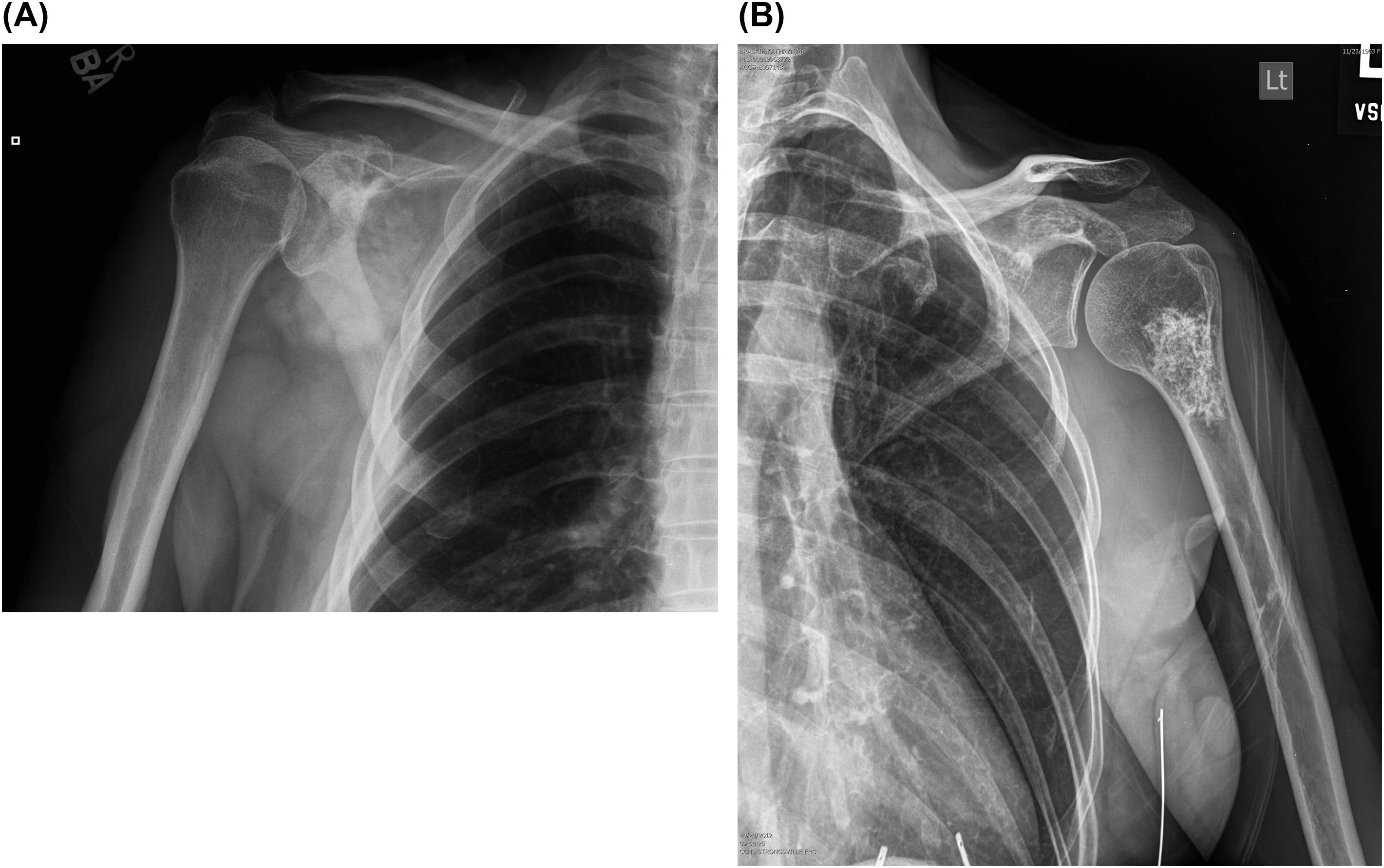
The radiograph should be scrutinized for associated periosteal reaction, tumor margins (or zone of transition), and tumor matrix [ ]. These observations serve to characterize the lesion. Bone sarcomas often show associated aggressive patterns of periosteal reaction such as a Codman's triangle, sunburst, hair-on-end, or multilamellated appearance ( Fig. 46.1 ). Their tumor margins are often ill-defined and can show a lytic permeative or moth-eaten appearance, which are again features of an aggressive underlying process ( Fig. 46.2 ). Mineralization of the tumor, or tumor matrix, can also be classified based on the radiographic appearance. Osteoid matrix is classically described as cloud-like or fluffy, while chondroid matrix is classically described as a rings and arcs pattern ( Fig. 46.3 ).


The importance of the radiograph in primary bone sarcoma evaluation cannot be overstated. In fact, if a patient has been evaluated with only MRI, a radiograph should be obtained to best characterize tumor margins and matrix. Signal intensity characteristics on MRI inconsistently permit characterization of the matrix of a lesion.
MRI remains the modality of choice for locally staging primary bone tumors [ ]. Although more expensive and time-consuming than CT, MRI does not use ionizing radiation to acquire cross-sectional images unlike CT. It best shows the contrast between normal fatty bone marrow and abnormally replaced marrow, thereby providing important information for local staging, assessment for intraosseous skip lesions, response to therapy, assessment for recurrence, and planning limb salvage surgical procedures ( Fig. 46.4 ). When assessing local staging, MRI is the best modality for showing not only the intramedullary extent of bone tumors, but also shows involvement of adjacent soft tissues, neurovascular bundles, and adjacent joint spaces. For all these reasons, a pretreatment MRI is very important for locally staging primary bone sarcomas. It should be noted too that obtaining an MRI prior to biopsy is mandatory to prevent misinterpretation of biopsy-related signal changes [ ].
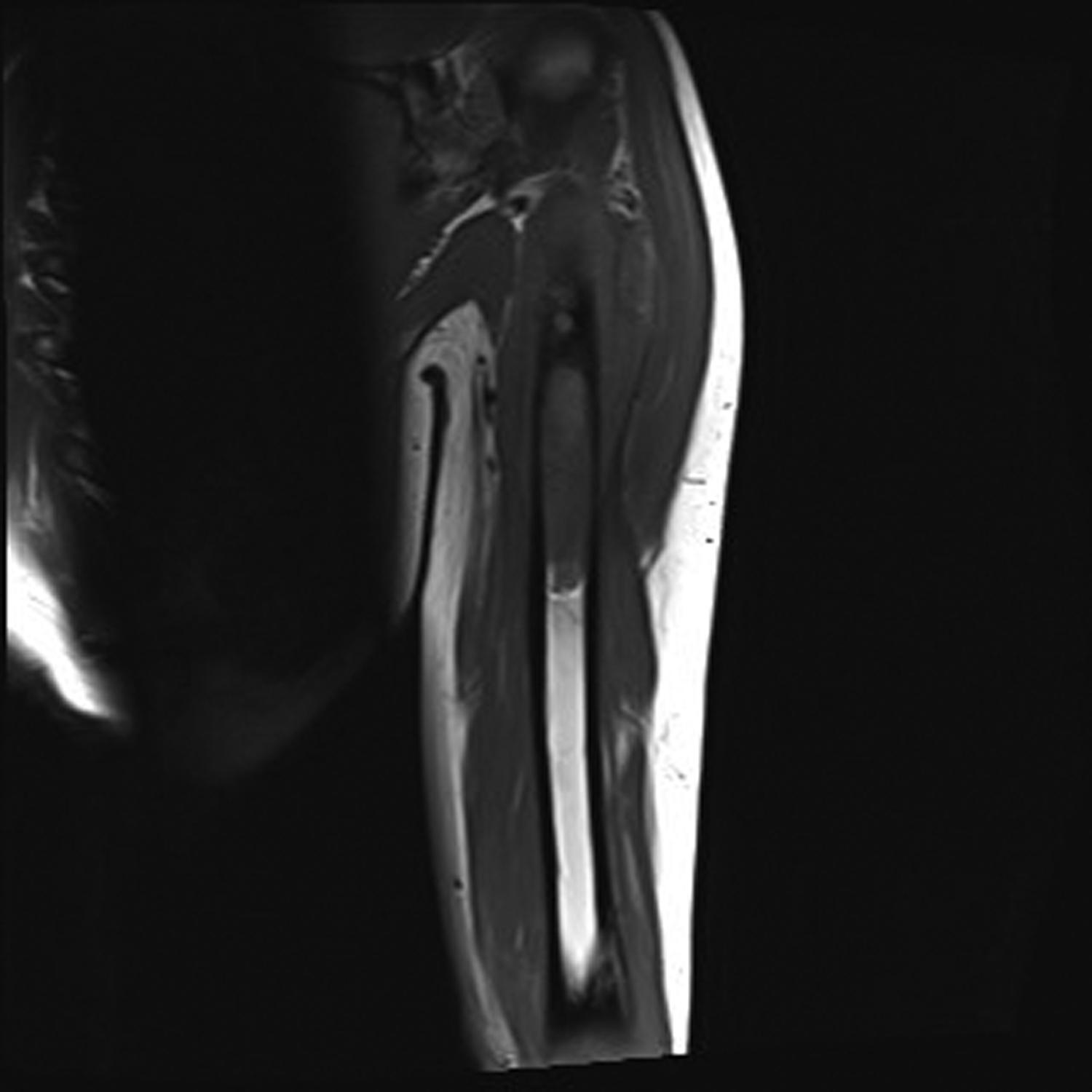
Regarding the imaging appearance of sarcomas on MRI, the nonspecific signal characteristics of heterogeneous decreased T1 signal and increased T2 signal are seen with most primary bone sarcomas. By contrast, a bone lesion showing focal normal high T1 fatty marrow signal is highly suggestive of a benign tumor, with rare exception [ ]. These signal characteristics that are seen with bone sarcomas do not on a consistent basis help differentiate or diagnose specific types of sarcomas, but rather help in assessing the extent of tumor involvement consistently and accurately.
Because of the superiority in soft tissue characterization with MRI, computed tomography (CT) has a narrow, but important, role in bone sarcoma imaging. The two most common uses of CT are to help in systemic staging and interventional planning of imaging-guided biopsy [ ]. A chest CT is the best modality to evaluate for pulmonary metastases, and it is routinely obtained for staging purposes to look for lung metastases. CT also has utility in biopsy planning, as biopsies of bone lesions are most commonly done percutaneously under CT guidance.
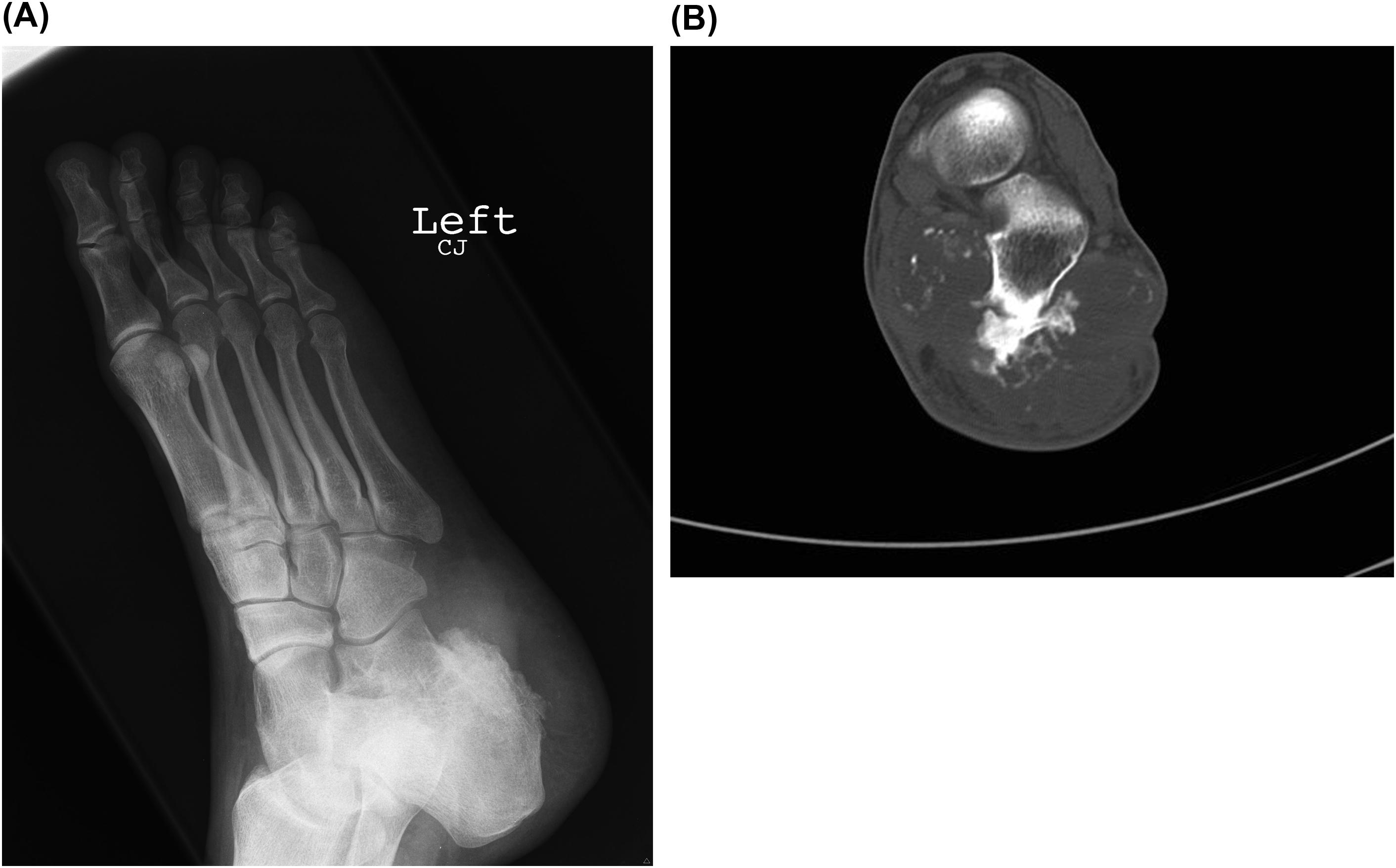
CT is technically the best modality for assessing cortical destruction and tumor mineralization, and can be helpful to the radiologist if these features are not clearly defined on the MRI and radiographs ( Fig. 46.5 ). It is not, however, obtained routinely to solely characterize these features because the combination of MRI and radiographs is often adequate for diagnostic purposes and local staging [ ].
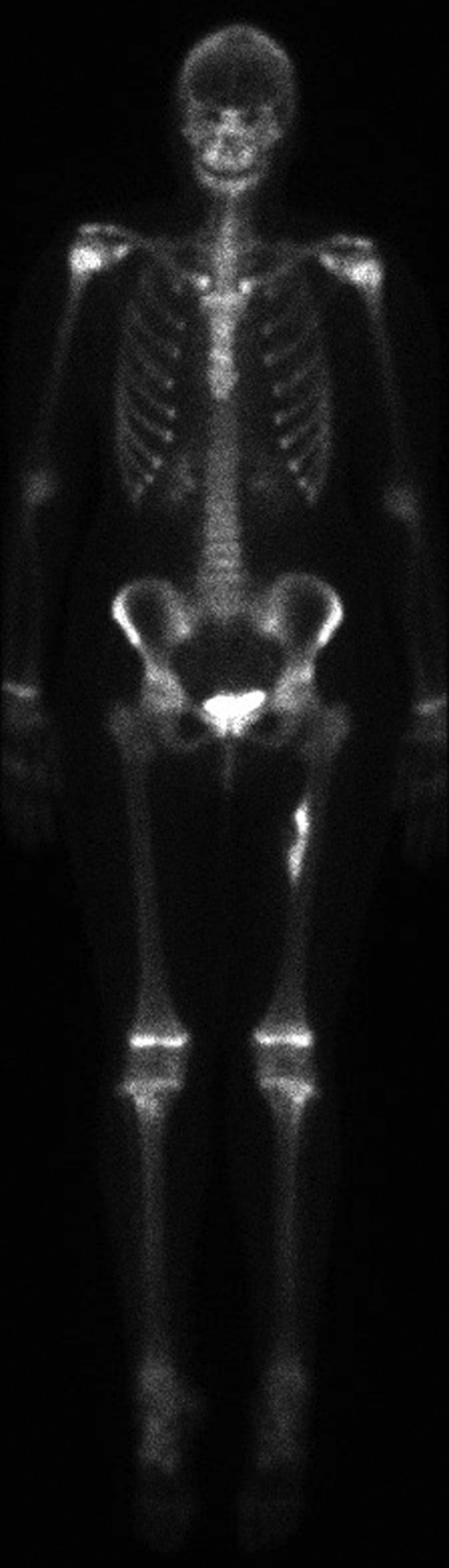
Bone scintigraphy is used to specifically evaluate for osseous metastases. It utilizes the radiopharmaceutical Technetium-99m labeled methylene diphosphonate (Tc-99m MDP), which is taken up by areas of increased osteoblastic activity. It is therefore most sensitive for finding osteoblastic bone lesions as opposed to osteolytic lesions ( Fig. 46.6 ).
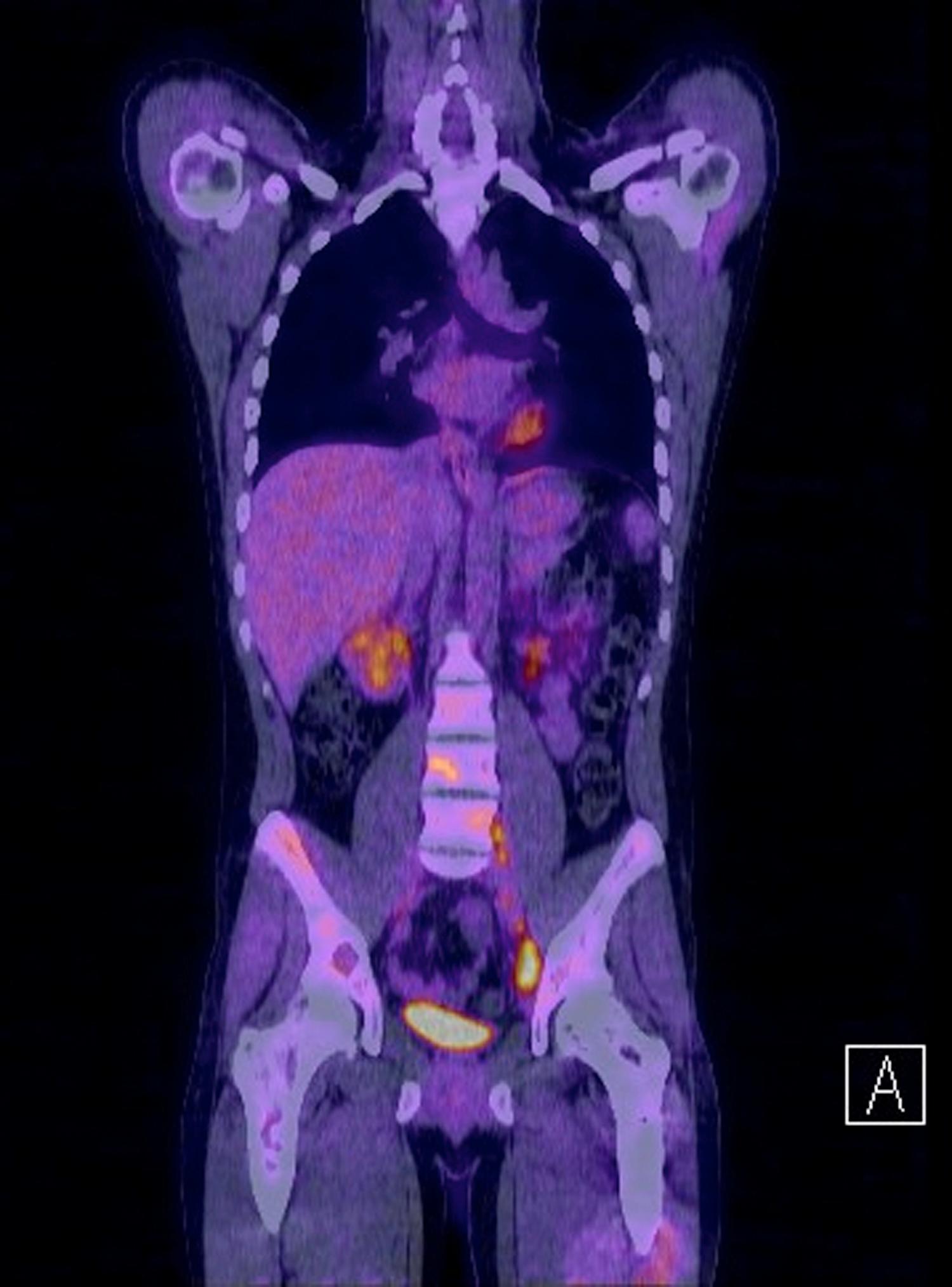
PET/CT utilizes the radiopharmaceutical 18-fluorodeoxyglucose, which is a glucose analog that is taken up most avidly by hypermetabolic tissues, such as aggressive neoplasms. PET/CT can be used to evaluate for both osseous and soft tissue metastases ( Fig. 46.7 ).
Although bone scintigraphy is currently the standard to evaluate for osseous metastases in patients with primary bone sarcomas, recent studies raise debate regarding the utility and sensitivity as compared to PET/CT [ ]. One study showed that Tc-99m MDP bone scan was the least sensitive at detecting osseous metastases compared to MRI or PET [ ]. Another study showed that PET/CT was more sensitive than bone scintigraphy at finding Ewing's sarcoma metastases [ ]. This same study did show, however, that when evaluating specifically for osteosarcoma metastases, bone scintigraphy was more sensitive than PET/CT.
Although PET/CT is not the current standard of practice in staging primary bone sarcomas, some studies show better accuracy in staging with PET/CT as compared to conventional imaging methods [ , ]. The drawbacks of using PET/CT as compared to bone scintigraphy are higher cost and higher radiation dose, the latter of which is an especially important consideration in a pediatric population. Even though PET/CT is emerging as a helpful imaging modality for primary bone sarcomas, more studies evaluating the cost-effectiveness and utility are likely needed before it may become standard of care.
Ewing's sarcoma of the bone has an incidence of approximately 3 per 1 million children and adolescents [ ]. It is the second most common primary musculoskeletal neoplasm after osteosarcoma in children and adolescents. An important and unusual feature is that it is very rare in African Americans [ ].
The most common sites of occurrence are the long bones, most commonly of the lower extremity with femoral involvement having the highest incidence [ ]. Within the long bones, the metadiaphysis and diaphysis are most common locations of involvement, and epiphyseal involvement is rare. Within the axial skeleton, the most common site of involvement by far is the pelvis with much less incidence in the spine, sacrum, scapula, ribs, clavicle, and skull.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here