Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Successful reconstruction of the acetabulum during revision total hip arthroplasty requires a thorough understanding of host bone defects. In an attempt to better define these defects, classification systems are used. The most commonly used systems are the American Academy of Orthopaedic Surgeons (AAOS) and Paprosky classifications of acetabular defects.
The Paprosky classification is based on the anteroposterior pelvis radiograph. It uses radiographic criteria to determine the classification: superior migration of the hip center in reference to the superior obturator line, the amount of ischial osteolysis, the degree of teardrop osteolysis, and the position of the hip center relative to the Köhler line.
Several different options are available for reconstruction of the acetabulum, including hemispheric cementless cups, jumbo cups, bilobed cups, high hip center, impaction grafting of the acetabulum, bulk structural allograft, antiprotrusio cages, cup cage reconstruction, and highly porous acetabular cups with or without modular porous augments. Each treatment option has its own advantages and disadvantages.
The number of primary total hip arthroplasty (THA) procedures being performed annually is continuing to rise, lending itself to a higher burden of revision THA. Over the past decade, technological advances and improved surgical techniques have made acetabular revision more successful and straightforward. The presence of acetabular bone loss at the time of revision continues to be a challenging problem.
The main goals of cementless acetabular revision are to (1) extract failed implants with minimal bone and soft tissue damage, (2) implant a stable cementless acetabular component to allow for biologic fixation, (3) obtain intimate contact with host bone, (4) restore the hip center of rotation, (5) allow for stress distribution to the remaining acetabular bone stock, and (6) manage bone deficiencies effectively to restore bone stock when possible.
The location and degree of acetabular bone loss can be predicted with the use of preoperative radiographs, including anteroposterior (AP) pelvis, AP hip, and cross-table lateral views. Computed tomography (CT) is helpful in further delineating bone loss secondary to acetabular osteolysis.
The advent of the acetabular “cup out” osteotome has facilitated removal of existing components, allowing for minimal iatrogenic bone loss. Restoring optimal hip biomechanics provides the highest likelihood of hip stability. These factors must be addressed in the planning process of the reconstruction and can be completed in such a way that the likelihood of success is optimized. This chapter focuses on classifying bone loss patterns about the acetabulum, the preoperative planning phase, the authors' approach to complicated cases, and the treatment options available for addressing acetabular bone loss. We do not discuss the use of custom triflange implants in this chapter.
The decision to proceed with revision hip surgery is the endpoint of a complex decision-making process involving the patient and the surgeon. The process should include the consideration of the severity of the patient's symptoms, along with the patient's function, disability, and general health as well as the surgeon's experience. However, revision hip arthroplasty usually is not indicated unless a specific problem is identified that can be surgically corrected—this is a critical part of the preoperative planning phase.
Indications for acetabular revision include instability, symptomatic aseptic loosening, failure of fixation, infection, wear, osteolysis, component malposition, and periprosthetic fracture. Revision may be indicated for an asymptomatic patient who has progressive osteolysis, severe wear, or bone loss that could render future reconstruction more difficult.
Historically, the most common indication for acetabular revision has been loosening of the acetabular component. However, Bozic and associates, using the Healthcare Cost and Utilization Project Nationwide Inpatient Sample database, recently found that the most common cause of revision hip surgery was instability or dislocation (22.5%). Mechanical loosening and infection were next in frequency at 19.7% and 14.8%, respectively. Instability or dislocation was the most common cause of an isolated acetabular revision (33%); mechanical loosening was the second most common indication (24%). In this study, 54% of all cases required revision of the acetabulum.
Contraindications for revision of the acetabular component include persistent infection and medical comorbidities that preclude surgery. In these patients, nonsurgical treatment such as activity modification, ambulatory aids, and oral analgesics may be appropriate.
The American Academy of Orthopaedic Surgeons (AAOS) classification of bone defects, as described by D'Antonio and associates, identifies the pattern and location of bone loss but does not quantify the defect ( Table 92.1 ). This system, which was developed by evaluating 83 AP and lateral hip radiographs and comparing results intraoperatively, is probably the most commonly used classification in the literature.
| Type I | Segmental defect
|
| Type II | Cavitary defect (intact rim)
|
| Type III | Combined defect |
| Type IV | Pelvic discontinuity |
| Type V | Arthrodesis |
The AAOS classification is based on two basic categories: segmental and cavitary defects. A segmental defect (type I) is defined as complete loss of bone in the hemisphere of the acetabulum, peripherally or centrally. A central segmental defect involves loss of the medial wall of the acetabulum. A cavitary deficiency (type II) is defined as volumetric bony loss of the acetabulum with an intact rim. These defects can occur peripherally or centrally. Medial cavitary defects involve loss of bone centrally with an intact medial wall, as in most cases of protrusio. The peripheral defects in types I and II are further divided by anatomic position: medial, superior, anterior, or posterior. Combined segmental and cavitary defects (type III) occur frequently. These include defects due to a failed, migrated endoprosthesis and those defects seen in developmental dysplasia.
Pelvic discontinuity (type IV) is an unusual condition defined as a separation between the superior pelvis and the inferior pelvis. Typically, this occurs through an inferior fracture line that extends to the greater sciatic notch. A high likelihood of a discontinuity is present when preoperative radiographs demonstrate a visible fracture line through the anterior and posterior columns, violation of the Köhler line, and/or rotation of the inferior aspect of the hemipelvis relative to the superior aspect, which is often seen as asymmetry of the obturator rings.
Arthrodesis is considered the final type of acetabular defect (type V) in this classification. Although this classification does define acetabular defects, its major flaw as a classification system is that it does not guide the management of these defects.
The Paprosky classification system is based on the severity of bone loss as seen with disruption of certain radiographic landmarks on preoperative radiographs. It was initially developed by evaluating the AP pelvis radiograph and comparing this information with intraoperative findings. The Paprosky classification system guides the reconstruction for a given bone loss pattern. The key to this classification is determining the ability of the remaining host bone to provide initial stability to a hemispheric cementless acetabular component until biologic fixation has been obtained. Intraoperative decision making is based on trial components; however, intraoperative findings can often be predicted by preoperative radiographs used in conjunction with the classification system.
Careful interpretation of the AP radiograph can predict the type of defect and can allow the surgeon to plan for the acetabular reconstruction. Four radiographic criteria are used to assess preoperative radiographs: (1) superior migration of the hip center compared with the superior obturator line, (2) ischial osteolysis, (3) teardrop osteolysis, and (4) position of the implant relative to the Köhler line ( Table 92.2 ).
| Defect | Rim | Walls | Columns | Migration | Teardrop Lysis |
|---|---|---|---|---|---|
| Type I | Intact | Intact | Intact/Supportive | None | None |
| Type II | Distorted | Distorted | Intact/Supportive | < 2 cm | |
| Type IIA | Distorted | Intact | Intact/Supportive | Superomedial | Minimal |
| Type IIB | Missing | Distorted | Intact/Supportive | Superolateral | Minimal |
| Type IIC | Distorted | Intact | Intact/Supportive | Medial | Severe |
| Type III | Missing | Compromised | Nonsupportive | > 2 cm | |
| Type IIIA | Missing | Compromised | Nonsupportive | Superolateral | Moderate |
| Type IIIB | Missing | Compromised | Nonsupportive | Superomedial | Severe |
Superior migration of the hip center represents bone loss in the acetabular dome, involving the anterior and posterior columns. Superior and medial migration indicates greater involvement of the anterior column. Superior and lateral migration indicates greater involvement of the posterior column. The amount of superior migration is measured as the distance in millimeters (adjusted for magnification) relative to the superior obturator line or a line drawn from the top of each obturator foramen.
Ischial osteolysis indicates bone loss from the inferior aspect of the posterior column, including the posterior wall. The amount of ischial osteolysis is quantified by measuring the distance (adjusted for magnification) from the most inferior extent of the lytic area to the superior obturator line. Mild ischial osteolysis is defined as less than 7 mm; severe ischial osteolysis is defined as greater than 15 mm.
Teardrop osteolysis indicates bone loss from the inferior and medial aspects of the acetabulum, including the inferior aspect of the anterior column, the lateral aspect of the pubis, and the medial wall. Moderate osteolysis is defined as partial destruction of the teardrop with maintenance of the medial limb of the teardrop. Severe involvement is defined as complete obliteration of the teardrop.
Medial migration of the component relative to the Köhler line represents a deficiency of the anterior column. The Köhler line, or the ilioischial line, is defined as a line connecting the most lateral aspect of the pelvic brim and the most lateral aspect of the obturator foramen on an anteroposterior radiograph of the pelvis. The medial aspect of the implant is lateral to the Köhler line with grade 1 migration and medial to the line with grade 3 migration. With grade 2 migration, migration to the Köhler line or slight remodeling of the iliopubic and ilioischial lines occurs without a break in continuity.
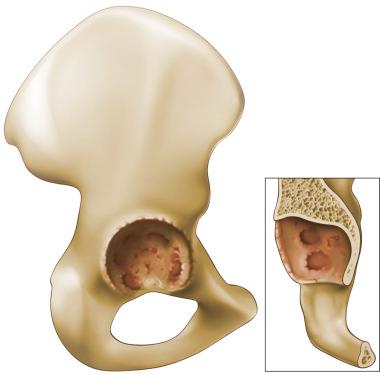
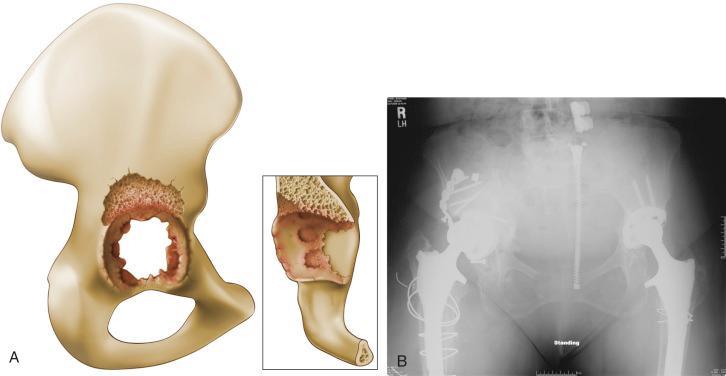
With a Paprosky type I defect, minimal bone loss is noted ( Fig. 92.1 ). The acetabulum is not distorted and the anteroposterior and posteroinferior columns are supportive. The acetabulum is hemispheric, and there may be small focal areas of contained bone loss. The preoperative radiograph shows no superior migration of the component, no evidence of osteolysis in the ischium or teardrop, and grade 1 medial migration (the Köhler line has not been violated). A hemispheric cementless implant is almost completely supported by native bone; however, a large cup may be required. Full inherent stability is achieved, and particulate grafting can be used to fill the minor areas of bone loss.
In a type II defect, the acetabulum is distorted but the columns are still able to support a cementless acetabular component. On the preoperative radiograph of a type II defect, superior migration of the hip center is less than 3 cm from the superior obturator line, osteolysis of the ischium is mild (< 7 mm distal to the obturator line), and osteolysis of the teardrop is not substantial. At least 50% of the surface area of the component is in contact with host bone to achieve biologic fixation, and good mechanical support can be provided entirely by host bone. The trial component has full inherent stability; however, the hip center may be elevated as much as 1.5 cm to achieve superior contact and support.
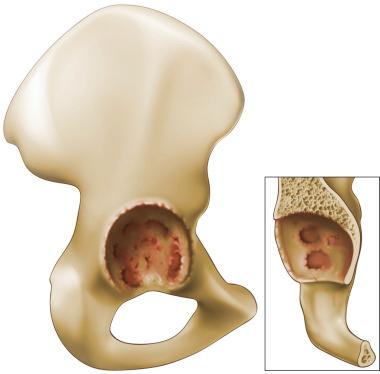
Type II defects are subclassified into types A, B, and C according to the direction of the bone loss pattern. Type IIA defects are oval enlargements of the acetabulum caused by < 2 cm of superomedial migration of the hip center ( Fig. 92.2 ). In most patients, the defect can be treated with particulate allograft because the remaining superior acetabular rim provides a buttress for containment of the allograft.
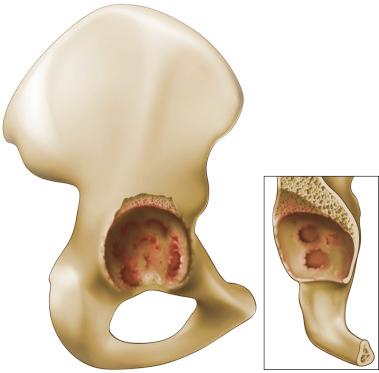
A type IIB defect is defined by < 2 cm of superolateral hip center migration ( Fig. 92.3 ). This defect is uncontained, but the anterosuperior and posteroinferior columns are supportive of an implant. Most reconstructions are done without grafting of the segmental defect because stability can be achieved through the remaining columns. Occasionally, an allograft can be used to restore bone stock; however, it is not supportive of the implant.
Type IIC defects ( Fig. 92.4 ) have a medial wall defect and migration of the acetabular component medial to the Köhler line. The acetabular columns are intact and will support a hemispheric component. Reconstruction of these defects is similar to treatment of protrusio acetabuli in the setting of a primary THA. Sequentially larger reamers are used until the acetabular columns can be engaged. Particulate bone graft can be placed medially to lateralize the hip center of rotation, restoring the anatomic position.
Type III Paprosky defects are the most severe and denote significant bone loss. The acetabular anterosuperior and posteroinferior columns are compromised and are nonsupportive. The remaining acetabular bone stock will not provide adequate initial component stability to achieve reliable biologic fixation; therefore, trial implants lack absolute stability (i.e., ability to undergo trial reduction without migration of the acetabular component). The acetabular component has migrated proximally more than 3 cm. These defects are further subdivided into two subtypes.
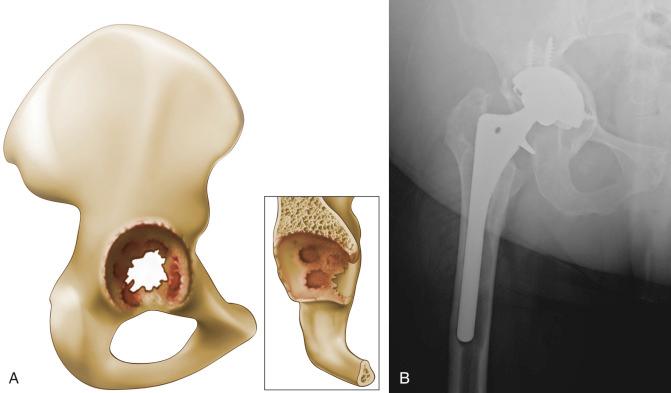
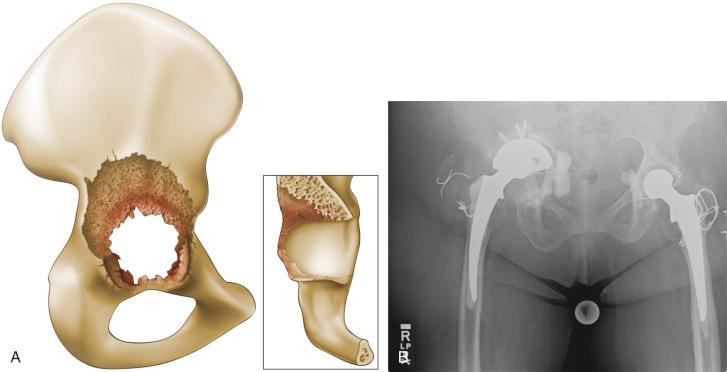
Type IIIA defects ( Fig. 92.5 ) are “up and out” defects; the bone loss is superolateral. The Köhler line is intact and there is mild to moderate ischial osteolysis, extending less than 15 mm inferior to the obturator line. Partial destruction of the teardrop is seen, but the medial limb usually is still present. Enough host bone is in contact with the ingrowth surface of a hemispheric component to attain durable biologic fixation (meaning that more than 50% of the surface area of the cementless cup is in contact with host bone). However, trial components typically achieve relative stability (i.e., the cup appears to be stable to manual pressure, but trial reduction would disengage the cup) and support of the implant with a porous modular metal augment or bulk allograft is necessary in the short term to provide initial construct stability.
Type IIIB defects ( Fig. 92.6 ) represent the most complex bone loss pattern. The failed acetabular component migrates superiorly and medially (“up and in”) because the medial wall has been destroyed. Patients with a type IIIB defect are at high risk for pelvic discontinuity, although pelvic discontinuity can be present with a type 2C and 3A defect. Preoperative radiographs often show severe ischial osteolysis, complete destruction of the teardrop, migration medial to the Köhler line, and migration greater than 3 cm superior to the obturator line. Less than 40% of the ingrowth surface of the acetabular component is in contact with host bone. Inherent stability is not achievable with a trial implant. Alternative techniques are often required to address these defects.
Any classification system must undergo validity and reliability testing to be universally accepted. In Paprosky's original paper, 92.5% agreement was reported between preoperative and intraoperative assessment or an assessment of the validity of the system. Gozzard and coworkers evaluated both of the discussed classification systems by having two orthopedic consultants and two orthopedic registrars examine 25 radiographs on two separate occasions. The validity of the Paprosky system, or the comparison between preoperative and intraoperative findings, was found to be good. The reliability of a system is defined as its ability to grade a given degree of bone stock loss in a consistent manner. Intraobserver reliability ranged from poor to good, depending on the experience of the observer, with the registrars having higher scores. Interobserver agreement was moderate in both classification systems.
In a separate study evaluating the AAOS and Paprosky systems, Campbell examined interobserver and intraobserver reliability for 33 hips needing revision hip arthroplasty. The originators of each system—three expert orthopedic surgeons and three senior residents—reviewed the films on two separate occasions at a minimum of 2 weeks apart. Overall reliability was poor for both systems. Intraobserver reliability of the originators was moderate for both, with the Paprosky classification being slightly more reliable. However, intraobserver reliability among orthopedic surgeons and residents was poor. Interobserver reliability was poor for both. Although these studies show that neither of these classification systems is perfect, the authors recommend the use of the Paprosky classification as it provides guidance as to what reconstruction should be employed given a certain acetabular bone loss pattern.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here