Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Nephron-sparing surgery (NSS) is indicated for the treatment of small renal masses, and the technique for NSS has transitioned from open to the minimally invasive approach. Although the initial experience with minimally invasive NSS used traditional laparoscopy, robotic surgery has evolved as the preferred approach given the benefits of three-dimensional (3D) vision and improved instrument dexterity. Similar to laparoscopy, most early adopters of robotic NSS preferred the transperitoneal approach to access the kidney. This preference was due in large part to the increased working space which allowed adequate separation of the robotic arms, decreasing external arm conflict, in addition to the familiar anatomic landmarks of the colon, liver, and spleen. However, posterior and lateral renal masses are not ideally suited to the transperitoneal technique and can be directly accessed via the retroperitoneal approach, reducing operative time by eliminating bowel mobilization and rotation of the kidney. As techniques to gain access to the retroperitoneal space have become more standardized, concerns regarding space limitations and disorientation have become less of a barrier to adoption. , Compared with the transperitoneal technique, the retroperitoneal approach has been shown to decrease operative times, length of stay, and estimated blood loss. Furthermore, there does not appear to be any increase in perioperative complications using this approach. In this chapter, we will discuss our approach for robotic retroperitoneal partial nephrectomy (RPPN), with a focus on modifications for the obese patient.
Positioning—Full flank with bed flexed at the umbilicus
Access—1 cm above iliac crest in midaxillary line, 10-mm kidney balloon dilator to create space
Exposing edge of the peritoneum and transversus abdominis
Port placement
Fat management, incision of posterior layer of Gerota fascia, and hilar exposure
Tumor exposure and creation of margin
Hilar clamping and tumor resection
Renorrhaphy
Once under general anesthesia, the supine patient is positioned using an underlying drawsheet so that the patient’s umbilicus is over the flexion point of the bed. They are then placed in a complete, full flank position to facilitate retroperitoneal access. Full flexion of the flank is necessary to increase the space between the 12th rib and iliac crest. The patient is stabilized using soft padding such as pillows and blankets, thus avoiding hard fixation aids such as the vacuum bean bag. This author prefers using a blanket rolled and taped into a large bolster. Starting at the end of the drawsheet, the blanket bolsters are rolled into the drawsheet toward the patient, essentially locking them in place along the patient’s back (large roll) and abdomen (small roll). It may be necessary to use an extension pad on each side of the table to support the blanket bolsters to accommodate an obese patient. A gel roll is used as the axillary support, and the arms are extended 90 degrees, with the lower arm resting on an armrest. Pillows are placed between the arms and legs, with adhesive tape securing them from moving. Prior to flexing the bed, the position of the patient is then checked, ensuring that the patient is in full flank and the shoulder and hip are inline. The bed is then maximally flexed without raising the kidney rest. The patient is then secured to the table with wide adhesive tape ( Fig. 20.1 A–C).

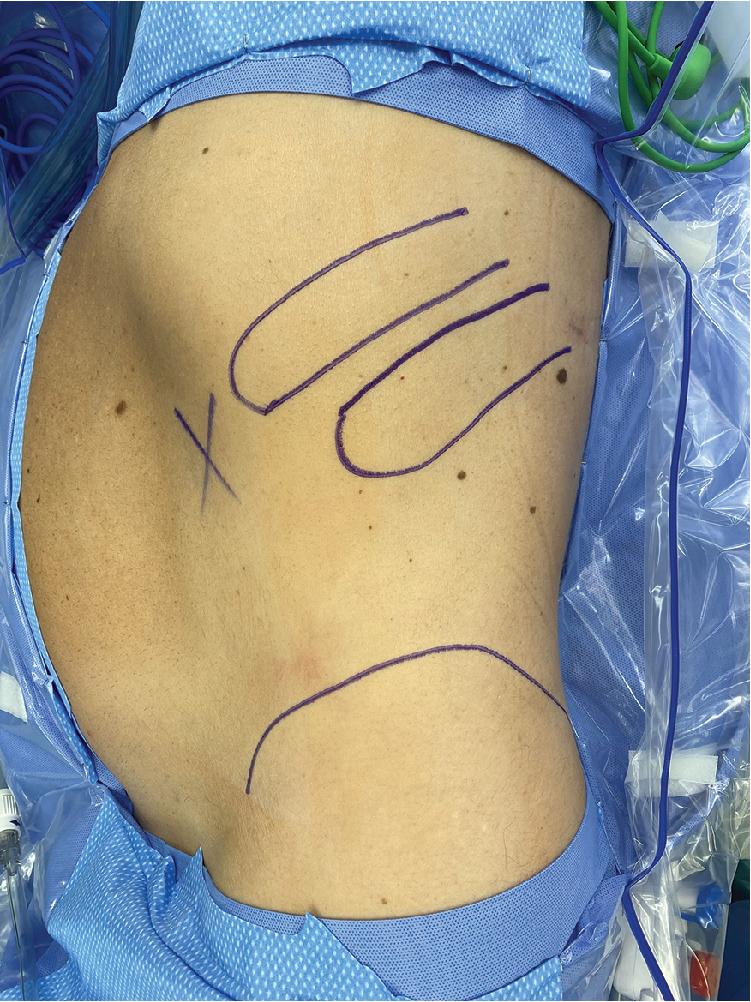
The iliac crest, 11th rib, and 12th rib are marked out. An incision is made approximately 1 cm above the iliac crest directly in the midaxillary line ( Fig. 20.2 ). Tissues are divided with cautery until the external oblique fascia is reached. This is incised with cautery, and finger dissection is used to bluntly gain access into the retroperitoneum. If the patient’s fascia is robust, a tonsil clamp can be used to gently perforate the lumbodorsal fascia to allow finger access. A 10-mm kidney-shaped balloon dilator is inserted into the space and inflated under direct vision (via either a laparoscopic camera or robotic camera with a 30-degree lens) in the appropriate craniocaudal orientation.
10-mm kidney-shaped balloon dilator
8-mm robotic port with the Hasson cone attachment
GelPOINT Mini (Applied Medical)—for an obese patient
AirSeal (CONMED) 120 mm; 150 mm may be needed for an obese patient
Indocyanine green (ICG)
As the balloon inflates, the paranephric fat will peel away, revealing the psoas, the gonadal vessels and ureter along the floor, and the edge of the peritoneum with the transversus abdominis muscle along the roof of the space. Keeping orientation with the psoas muscle horizontal as the floor is key during the entire operation because this is the most prominent and identifiable landmark. The other key landmark is the posterior layer of the Gerota fascia, which will be pushed off the psoas muscle by the balloon dilator. After the balloon has been fully inflated, it is removed, and a camera port is inserted into the retroperitoneum. In most patients an 8-mm robotic port with the Hasson cone attachment is used as the initial access port and insufflation is performed to 15 mm Hg to create a working space. In an obese patient, we routinely use the GelPOINT Mini (Applied Medical) as our initial access port and the 8-mm robotic port is placed directly though the gel cap of the device ( Fig. 20.3 ). The GelPOINT Mini can assist by decreasing the width of the abdominal wall, which creates more space and allows a greater range of motion of the camera point. In addition, the smaller footprint of the GelPOINT Mini allows the other robotic ports to be placed without having to change the port configuration. It may be necessary to wrap Vaseline gauze around the GelPOINT if gas is leaking around the edges.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here