Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
“Doctor, I have hemorrhoids” is a common complaint. The majority of these complaints are not truly hemorrhoids but other benign conditions; some may hide a more threatening diagnosis, such as anal cancer. Evaluating each patient based on his or her symptoms is important to avoid missing a condition that may require further management. Management of symptomatic hemorrhoids requires an in-depth understanding of the anorectal anatomy for successful treatment and to avoid complications.
Hemorrhoids are normally occurring vascular cushions found within the anal canal. They are described as being predominately at three anatomic locations in the anal canal (i.e., in left lateral, right anterolateral, and right posterolateral columns) ( Fig. 32.1A ). However, in reality, this is not always the case, and they often are more circumferential. Their location is around the dentate line, which is an anatomic landmark that divides the anal canal based on the epithelial lining and nerve supply. The region above the dentate line is insensate, whereas that below is supplied by nerve endings that perceive pain. This is an important landmark to consider when treatment is planned. Hemorrhoids are found in the submucosal layer and are considered sinusoids because they typically have no muscular wall. They are suspended in the anal canal by the muscle of Treitz, which is a submucosal extension of the conjoined longitudinal ligament.
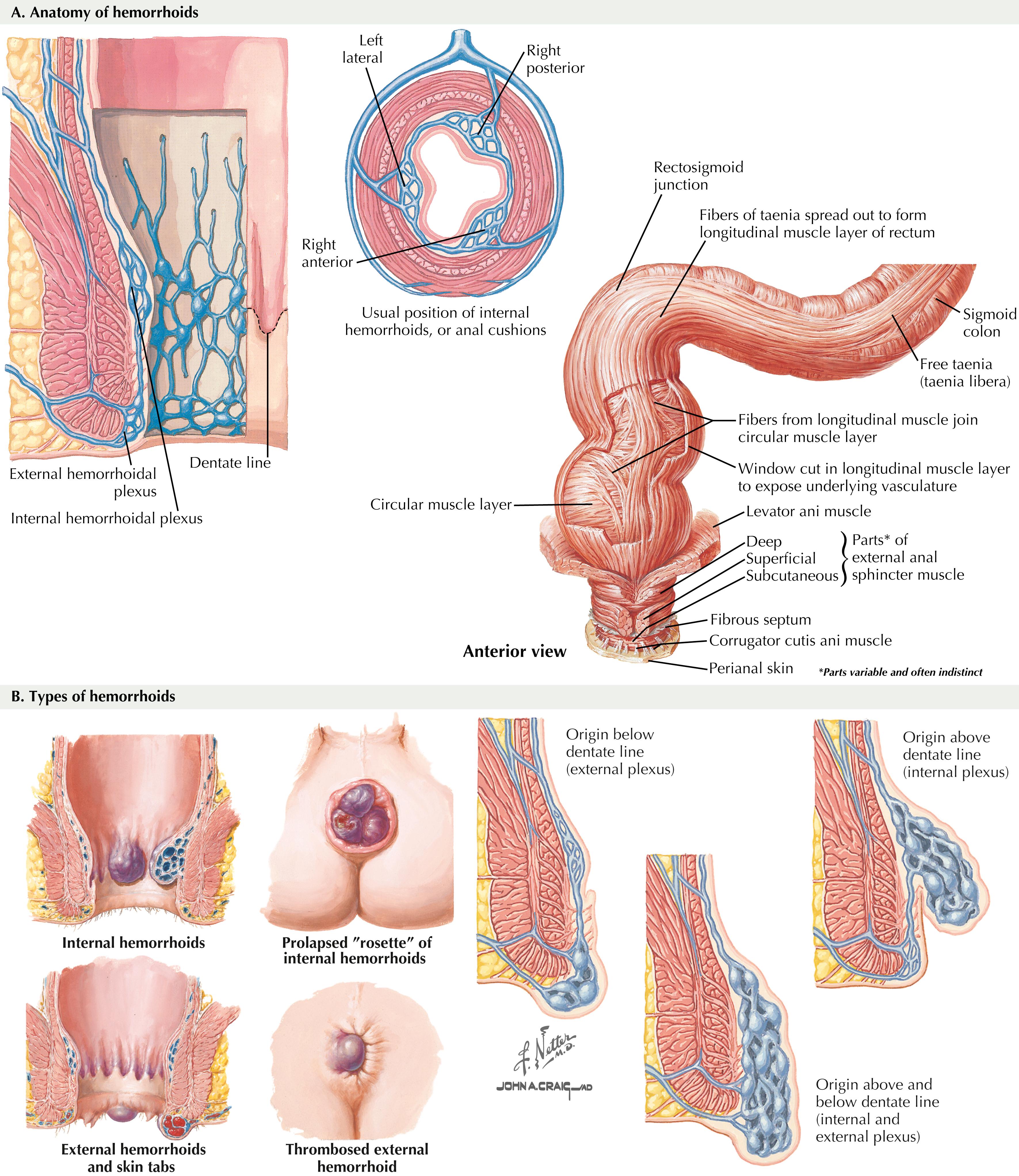
Anatomically, hemorrhoids are classified as internal or external. Internal hemorrhoids are located proximal to the dentate line and have visceral innervation; therefore, the most common presentation is painless bleeding. Because they are close to the anal transitional zone (ATZ), internal hemorrhoids can be covered by columnar, squamous, or basaloid cells. External hemorrhoids are located in the distal third of the anal canal and are covered by anoderm (i.e., squamous epithelium). Because of the somatic innervation of external hemorrhoids, patients who have these are more likely to be seen with pain when these are inflamed, and interventional treatment will require some form of anesthesia ( Fig. 32.1B ).
Hemorrhoids are thought to enhance anal continence and may contribute 15% to 20% of resting anal canal pressure. They also provide complete closure of the anus, enhancing control of defecation. In addition to making important contributions to the maintenance of continence through pressure phenomena, hemorrhoids also relay important sensory data regarding the composition (gas, liquid, stool) of intrarectal contents. Hence it may be important to make note of this, especially in patients who have low sensation in the rectum and anal area, such as spinal cord injury patients, in whom internal sphincter tone and hemorrhoid function may be the only factors contributing to continence.
The central causative pathway for the development of hemorrhoidal pathology is an associated increase in intraabdominal pressure. This increase may be secondary to straining, constipation, or obesity. Other etiologic factors can include diarrhea, pregnancy, and ascites. Aging is also associated with dysfunction of the supporting smooth muscle tissue, resulting in prolapse of hemorrhoidal tissues.
Hemorrhoids are normal structures and thus are treated only if they become symptomatic. Common complaints include bleeding, pain, prolapse, and swelling. After nonoperative measures have failed, treatment is largely applied on the basis of size and symptomatology. Internal hemorrhoids classically are categorized as grade 1, with enlargement, but no prolapse outside the anal canal; grade 2, with prolapse through the anal canal on straining, but with spontaneous reduction; grade 3, manual reduction required; or grade 4, hemorrhoids cannot be reduced into the anal canal.
First-degree hemorrhoidal disease can usually be treated with nonsurgical measures. The primary goal is to decrease straining with bowel movements and thus reduce the intra-abdominal pressure transmitted to the hemorrhoidal vessels. Larger hemorrhoids may present with prolapse of the mucosal lining with or without bleeding. Irritation of the external hemorrhoid may cause pain/itching. The mainstay of nonoperative hemorrhoidal treatment is aimed at keeping the stool soft and consists of increased fiber and water consumption.
Patients with second-degree hemorrhoids can be offered a trial of nonsurgical management, although a number of these measures may fail and require procedural intervention. Third- and fourth-degree hemorrhoids generally require surgery.
Common office procedures in the management of patients with symptomatic hemorrhoids include rubber band ligation, infrared coagulation, bipolar diathermy, sclerotherapy, and cryotherapy. All these techniques rely on some form of tissue destruction, which then results in fixation of the remaining hemorrhoidal tissues.
Rubber band ligation is the most frequently used procedure in the United States. This technique is most often used to address first- and second-degree hemorrhoids, although third-degree hemorrhoids can occasionally be treated with this technique as well. The rubber band causes necrosis of the intervening tissue over the course of 7 to 10 days and is passed in the patient’s stool. The resultant ulcer and scar are thought to cause a local “pexy” of the surrounding tissue. The most common of the many implements available for application of the rubber bands is a suction ligator, which allows the surgeon to draw in the hemorrhoidal tissue and apply the rubber band with one hand ( Fig. 32.2A ). Other devices require that the operator grasp the hemorrhoidal pedicle with a long forceps and apply the rubber band with the other hand ( Fig. 32.2B and C ). The most important visual factor is application of the band above the dentate line. Questioning the patient about pain and sensation before applying the band may prevent application of the band at an incorrect site.
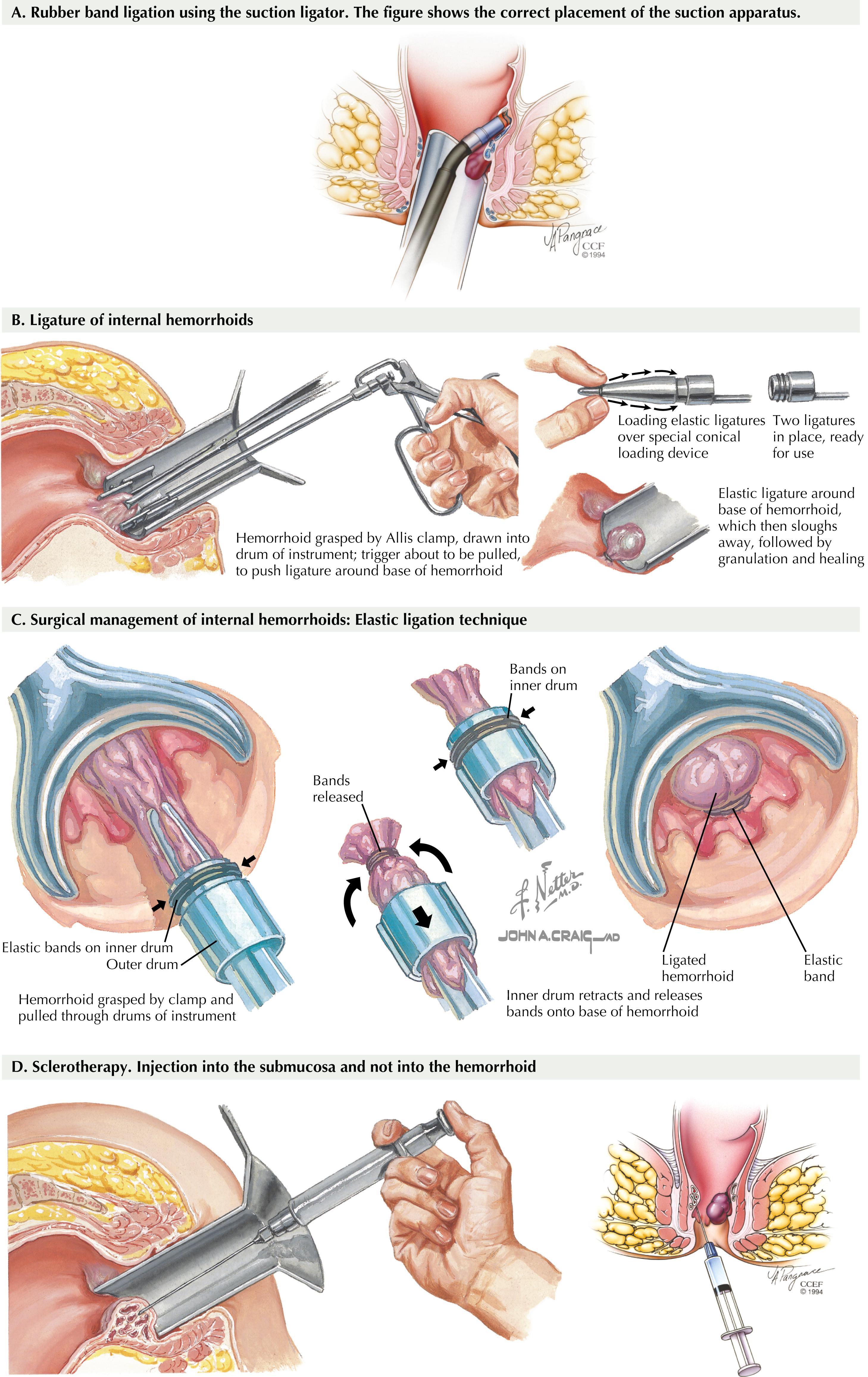
Hemorrhoidal banding controls bleeding in more than 90% of cases. Complications are rare but include vasovagal response, pain, bleeding, and pelvic sepsis. Pelvic sepsis may rarely result from perforation by incorporation of the distal rectal wall into the band. Classically, the combination of pain, urinary retention, and fever after banding should raise suspicion of pelvic sepsis.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here