Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Intussusception is the most frequent cause of bowel obstruction in infants and toddlers. It is an acquired invagination of the proximal bowel (intussusceptum) into the distal bowel (intussuscipiens). It was first described in 1674 by Paul Barbette of Amsterdam, defined by Treves in 1899, and operated on successfully in 1873 by John Hutchinson.
The intussusceptum telescopes into the distal bowel by peristaltic activity. There may or may not be a lead point. As the mesentery of the proximal bowel is drawn into the distal bowel, it is compressed, resulting in venous obstruction and bowel wall edema. If reduction of the intussusception does not occur, arterial insufficiency will ultimately lead to ischemia and bowel wall necrosis. Although spontaneous reduction can occur, the natural history of an intussusception is to progress to bowel ischemia and necrosis unless the condition is recognized and treated appropriately.
A majority of cases, especially in infants, do not have a lead point and are classified as primary or idiopathic intussusceptions. The cause is generally attributed to hypertrophied Peyer patches within the bowel wall. Intussusception occurs frequently in the wake of an upper respiratory tract infection or an episode of gastroenteritis, providing an etiology for the hypertrophied lymphoid tissue. Adenoviruses in children older than age 2 and, to a lesser extent rotaviruses, have been historically implicated in up to 50% of cases. Other contributing evidence that viruses may play a role in intussusception includes the rise in cases during seasonal respiratory viral illnesses and the increased risk associated with rotavirus immunization. The initial rotavirus vaccine was removed from the market due to a significant increase in the incidence of intussusception. The current immunization formulas available in the United States, RotaTeq and Rotarix, also have been associated with a small increased risk, but these risks are widely thought to be outweighed by the benefits of vaccination.
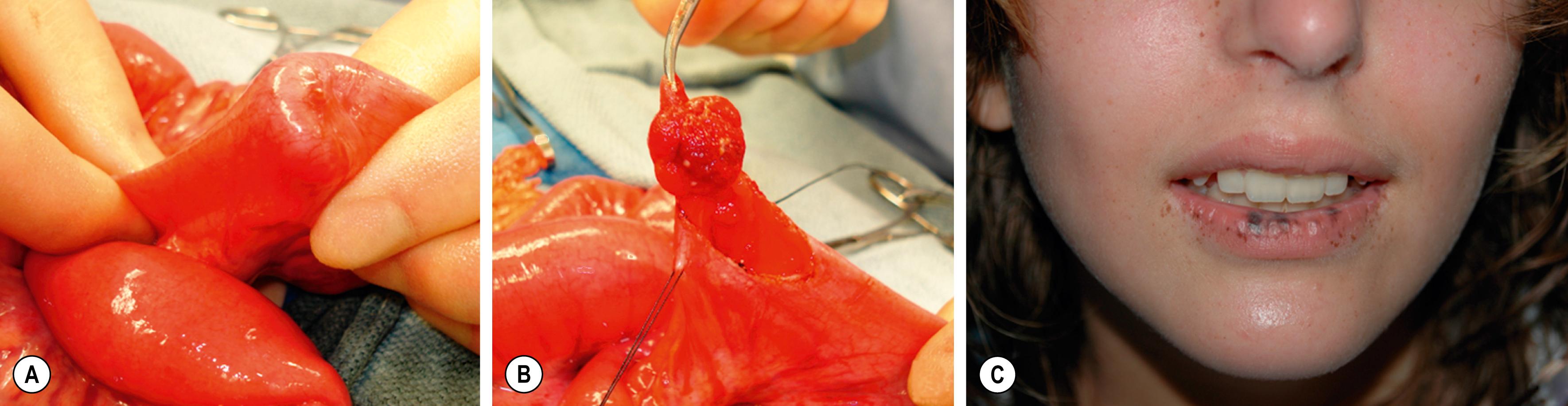
An intussusception can have an identifiable lesion that serves as a lead point, drawing the proximal bowel into the distal bowel by peristaltic activity. The incidence of a lead point varies from 1.5–12%, and the presence of a lead point increases in proportion with age. The most common lead point is a Meckel diverticulum followed by polyps and duplications. Other benign lead points include the appendix, hemangiomas, carcinoid tumors, foreign bodies, ectopic pancreas or gastric mucosa, hamartomas from Peutz–Jeghers syndrome ( Fig. 38.1 ), and lipomas. Malignant causes, although rare, increase in incidence with age and include lymphomas and small bowel tumors. Systemic diseases, including Henoch–Schönlein purpura and cystic fibrosis, have been associated with intussusception. Other diseases that may be related to intussusception include celiac disease and Clostridium difficile colitis.
Idiopathic intussusception can occur at any age. Most affected patients are well-nourished, healthy infants, and approximately two-thirds are boys. The highest incidence occurs in infants between ages 4 and 9 months, and it is the most common cause of small bowel obstruction in this age group. Intussusception is uncommon below 3 months and after 3 years of age. The condition has been described in premature infants and has been postulated as the cause of small bowel atresia in some cases.
The classic presentation is an infant or a young child with intermittent, cramping abdominal pain associated with “currant jelly” stools and a palpable mass on physical examination, although this triad is seen in less than a fourth of children. The abdominal pain is sudden, and the child may stiffen and pull the legs up to the abdomen. The pain also can be associated with hyperextension, writhing, breath holding, and vomiting. The attack often ceases as suddenly as it started. Between attacks, the child may appear comfortable but eventually will become lethargic. Small or normal bowel movements will stop as the obstruction progresses and becomes associated with bilious emesis and increasing abdominal distention. Stools may be blood tinged as impending ischemia causes mucosal sloughing and compression of mucous glands leading to evacuation of dark red mucoid clots or currant jelly stools. This is often a late sign, as are laboratory derangements. A pitfall is to wait for the currant jelly stool, leukocytosis, and electrolyte abnormalities that are often the hallmarks of ischemic bowel.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here