Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Damage control resuscitation (DCR) has become a staple of modern surgical management of traumatic injuries. Hemorrhage secondary to trauma accounts for 40% of trauma fatalities and is the leading cause of preventable death in trauma. Research in military and civilian populations regarding DCR have focused on ways to improve survival in patients with severe hemorrhage. It should be mentioned that the majority of trauma patients do not require DCR, and its techniques should be reserved for those who are the most severely injured. For these patients the rapid and effective use of techniques to control bleeding and correct acute coagulopathy of trauma shock is essential.
Well-established principles of DCR include preferential use of blood product transfusion over crystalloid for resuscitation and permissive hypotension. In the early 2000s, much research centered on the optimal ratios of blood products for DCR, with recommendations to target 1:1:1 ratios of packed red blood cells (PRBCs), plasma, and platelets for patients who are receiving massive transfusion as part of their DCR. More recently, thromboelastography (TEG) has emerged as a guide for resuscitation, replacing ratio-driven end points, though many massive transfusion protocols (MTPs) still use ratios as a guide. Another new development over the past few years has been renewed interest in whole blood (WB) use for DCR rather than component product use. Resuscitative endovascular balloon occlusion of the aorta (REBOA) represents a unique intervention aimed at achieving early hemorrhage control as a component of damage control resuscitation that has been developed rapidly and adopted widely over the past few years.
MTPs have progressively become more widely adopted and are an essential component of a well-functioning trauma center. Historically, transfusion protocols have been cultivated throughout the years from early observations to studies on smaller and limited patient populations. More extensive, original evidence evolved from military experience, specifically from increased combat activity associated with Operation Iraqi Freedom and Operation Enduring Freedom. In addition, many civilian populations have begun to adopt the use of DCR into their MTPs. However, there still exits variability among MTPs throughout civilian institutions. The difference may ultimately stem from the variability of patient populations, especially with regard to the mechanism complexity of injuries.
Recognizing that trauma is an extremely time-sensitive disease process and that early hemorrhage control and resuscitation techniques are crucial in improving outcomes, prehospital interventions as components of DCR have been the focus of much recent interest as well, including prehospital transfusion, prehospital tourniquet use for hemorrhage control, and use of tranexamic acid (TXA), as well as timing of transfusion/resuscitation and minimization of prehospital crystalloid use ( Table 1 ).
| Author (Date) | Title | Outcome | Level of Evidence | Category | DOI |
|---|---|---|---|---|---|
| Cassignol (2020) | Civilian prehospital transfusion—experiences from a French region | Prehospital blood transfusions are safe. Coagulation disorders and acidosis remain a cause of premature death in patients with prehospital transfusions. | 3 | Prehospital transfusion, outcomes | 10.1111/vox.12984 |
| Vuorinen (2020) | Prehospital administration of blood products: experiences from a Finnish physician-staffed helicopter emergency medical service | A prehospital physician-staffed HEMS unit carrying blood products is a feasible and safe method to start transfusion roughly 30 min before arrival to the hospital. | 3 | Prehospital transfusion, outcomes | 10.1186/s12873-020-00350-x |
| Gurney (2020) | Improved survival in critically injured combat casualties treated with fresh whole blood by forward surgical teams in Afghanistan | In forward-deployed environments, where component products are limited, FWB has logistical advantages and was associated with reduced mortality in casualties with a critical combat mortality index. Additional analysis is needed to determine if these effects of FWB are appreciable in all trauma patients or just in those with severe physiologic derangement. | 3 | Whole blood, component therapy, outcomes, prehospital | 10.1111/trf.15767 |
| Anto (2020) | Severity of hemorrhage and the survival benefit associated with plasma: results from a randomized prehospital plasma trial | Patients who received 4 to 7 units of red cells demonstrated the most robust independent survival benefit attributable to prehospital plasma transfusion. Prehospital plasma may be most beneficial in those patients with moderate transfusion requirements and mortality risk. | 1 | Prehospital plasma, outcomes | 10.1097/TA.0000000000002530 |
| Reitz (2020) | Prehospital plasma in injured patients is associated with survival principally in blunt injury: results from two randomized prehospital plasma trials | A survival benefit associated with prehospital plasma at 24 hours and 28 days exists primarily in blunt injured patients with no benefit shown in penetrating trauma patients. No detrimental effects attributable to plasma are demonstrated in penetrating injury. | 1 | Prehospital plasma, outcomes | 10.1097/TA.0000000000002485 |
| Oakeshott (2019) | Feasibility of prehospital freeze-dried plasma administration in a UK Helicopter Emergency Medical Service | Prehospital freeze-dried plasma and PRBC transfusion is feasible in a 1:1 ratio in patients with suspected traumatic hemorrhage. The use of freeze-dried plasma as a first-line fluid bolus reduced the number of prehospital PRBC units required and reduced the time to transfusion. | 3 | Prehospital transfusion, outcomes | 10.1097/MEJ.0000000000000585 |
| Shlaifer (2019) | The impact of prehospital administration of freeze-dried plasma on casualty outcome | The use of FDP in the prehospital setting has logistic benefits and a positive effect on coagulation profile, with no other significant effects. | 3 | Plasma, prehospital | 10.1097/TA.0000000000002094 |
| Griggs (2019) | Mortality of civilian patients with suspected traumatic hemorrhage receiving prehospital transfusion of PRBCs compared to prehospital crystalloid | In a single-center UK HEMS study, in patients with suspected traumatic hemorrhage who received a prehospital PRBC transfusion instead of crystalloid, there was an observed, but nonsignificant, reduction in mortality at 6 hours and 28 days, also reflected in a massive transfusion subgroup. Patients receiving prehospital PRBCs were significantly less likely to require an in-hospital major transfusion. | 3 | Crystalloids, blood, resuscitation, | 10.1186/s13049-018-0567-1 |
| Pusateri (2020) | Association of prehospital plasma transfusion with survival in trauma patients with hemorrhagic shock when transport times are longer than 20 minutes: a post hoc analysis of the PAMPer and COMBAT clinical trials | Two recent randomized clinical trials were published, with apparently contradictory results. The Prehospital Air Medical Plasma (PAMPer) clinical trial showed a nearly 30% reduction in mortality with plasma transfusion in the prehospital environment, while the Control of Major Bleeding After Trauma (COMBAT) clinical trial showed no survival improvement. These data suggest that prehospital plasma is associated with a survival benefit when transport times are longer than 20 minutes and that the benefit-risk ratio is favorable for use of prehospital plasma. | 2 | Crystalloids, blood, resuscitation | 10.1111/trf.15161 |
| Holcomb (2013) | The Prospective, Observational, Multicenter, Major Trauma Transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks | Prospective cohort study, time-dependent proportional hazards models (1:4 vs. 1:2). Not specifically prehospital. ↑ PLT:RBC & FFP:RBC ratios →↑ survival | 1 | Prospective, hemorrhage, ratios | |
| Chapman (2015) | Combat initial experience with a randomized clinical trial of plasma-based resuscitation in the field for traumatic hemorrhagic shock | Randomized controlled trial comparing prehospital plasma to saline. No difference in 28-day mortality, safety outcomes, or adverse events. | 1 | Hemorrhage, resuscitation, outcomes | |
| Holcomb (2015) | Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs. a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial | Pragmatic, phase 3, multisite, randomized clinical trial of 1:1:1 plasma:platelets:PRBCs vs. 1:1:2. 1:1:1 group had decreased exsanguination and increased hemostasis. No difference in 24-hour or 30-day mortality. No differences in complications. | 1 | Ratios, hemorrhage, outcomes | |
| Shackelford (2017) | Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30-day survival | Retrospective military cohort study. Prehospital transfusion is associated with decreased 24-hour and 30-day mortality. | 3 | Military, prehospital, resuscitation, outcomes | |
| Sperry (2018) | Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock | Pragmatic, phase 3, multisite, randomized clinical trial of 1:1:1 (plasma group) vs. 1:1:2. Plasma group had decreased 30-day mortality, with Kaplan-Meier curves showing early separation that persisted to 30 days. Plasma group had improved hemostasis as measured by median prothrombin time. No differences in multiorgan failure, acute lung injury–acute respiratory distress syndrome, nosocomial infections, or allergic or transfusion-related reactions. | 1 | Air care, resuscitation, outcomes, plasma | 10.1001/archsurg.2011.287 |
| Moore (2018) | Plasma-first resuscitation to treat hemorrhagic shock during emergency ground transportation in an urban area: a randomized trial | During rapid ground rescue to an urban Level I trauma center, use of prehospital plasma was not associated with survival benefit. Blood products might be beneficial in settings with longer transport times, but the financial burden would not be justified in an urban environment with short distances to mature trauma centers. | 1 | Plasma, urban, prehospital, outcomes | 10.1016/S0140-6736(18)31553-8 |
| Timing of Resuscitation | |||||
| Cap (2012) | Timing and location of blood product transfusion and outcomes in massively transfused combat casualties | Early HIGH ratio platelet:RBC was independently associated with. increased survival at both 24 hours and 30 days. Increased early FFP:RBC ratio was also independently associated with increased survival. | 3 | Timing of resuscitation, outcomes | |
| Ferrada (2018) | Circulation first—the time has come to question the sequencing of care in the ABCs of trauma; an American Association for the Surgery of Trauma multicenter trial | Many trauma centers are already initiating circulation first prior to intubation when treating hypovolemic shock (CAB), even in patients with a low GCS. This practice was not associated with increased mortality. Further prospective investigation is warranted. | 3 | Circulation, airway, prehospital | 10.1186/s13017-018-0168-3 |
| Eastridge (2019) | Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury | The majority of potentially preventable deaths after trauma are related to hemorrhage and occur early after injury, with the largest number of deaths occurring before hospital arrival. Approximately one fourth of trauma deaths may be potentially preventable through early medical and surgical interventions. Interventions dedicated to bleeding control and hemostatic resuscitation have demonstrated merit in decreasing hemorrhagic injury mortality. Advancing these novel strategies to the casualty in the prehospital phase of care, particularly in tactical or austere environments, may prove beneficial for hemorrhage mitigation to temporize the window of survival to definitive care. Future studies of resuscitation and survival after traumatic injury must include analysis of prehospital deaths to fully understand the outcomes of early interventions. | 3 | Death location, severe hemorrhage, outcomes | |
| TXA | |||||
| CRASH-2 Trial Collaborators (2010) | Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant hemorrhage (CRASH-2): a randomized, placebo-controlled trial | All-cause mortality was significantly reduced with TXA. The risk of death due to bleeding was significantly reduced. | 1 | TXA, outcomes, timing | |
| Morrison (2012) | Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) study | TXA group had lower unadjusted mortality than the no-TXA group despite being more severely injured. This benefit was greatest in the group of patients who received massive transfusion, where TXA was also independently associated with survival and less coagulopathy. | 1 | Military, outcomes, TXA | DOI |
| CRASH-2 Trial Collaborators (2019) | Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomized, placebo-controlled trial | Patients with mild to moderate head injury randomized to receive TXA had decreased risk of death. Early treatment was more effective than later treatment. There was no difference in vascular occlusive events or seizures. | 1 | TBI, TXA, outcomes | 10.1097/ta.0000000000000689 |
| Guyette (2020) | Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: a double-blind, placebo-controlled, randomized clinical trial | Randomized controlled trial comparing prehospital TXA to placebo found no difference in 30-day mortality, complications, or adverse events. It was associated with survival benefit in specific subgroups. | 1 | TXA, hemorrhage, outcomes | 10.1001/jamasurg.2020.4350 |
| Dixon (2020) | TXA administration in the field does not affect admission TEG after traumatic brain injury | d -dimer and PAP levels reflect a lower degree of fibrinolysis following prehospital administration of TXA when compared to placebo in a large prehospital trial of patients with TBI, but TEG obtained on admission and 6 hours later did not demonstrate any differences in fibrinolysis between the two TXA dosing regimens and placebo. | 1 | TXA, TBI hemorrhage, outcomes | 10.1097/TA.0000000000002932 |
| Boudreau (2019) | Prehospital tranexamic acid administration during aeromedical transport after injury | Prehospital administration of TXA during aeromedical transport did not improve survival compared with ED administration. Treatment with TXA was associated with increased risk of venous thromboembolic events. | 3 | TXA, hemorrhage, outcomes | 10.1016/j.jss.2018.07.074 |
| Neeki (2018) | Tranexamic acid in civilian trauma care in the California Prehospital Antifibrinolytic Therapy Study | TXA use in the civilian prehospital setting may safely improve survival outcomes in patients who have sustained traumatic injury with signs of hemorrhagic shock. | 2 | TXA, hemorrhage, outcomes | 10.5811/westjem.2018.8.39336 |
| Myers (2019) | Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism | Tranexamic acid was associated with more than threefold increase in the odds of VTE. It was not significantly associated with survival. Risk of VTE remained elevated in the TXA cohort despite accounting for mortality. | 2 | Complications, TXA, outcomes | 10.1186/s40779-018-0178-1 |
| Crystalloid Use | |||||
| Carrick (2016) | Intraoperative hypotensive resuscitation for patients undergoing laparotomy or thoracotomy for trauma | This trial comparing low intraoperative MAP vs. high MAP enrolled 168 patients before early termination in part because of clinical equipoise and futility. No significant survival advantage existed for the LMAP group vs. HMAP at 30 days or 24 hours. There were no differences in secondary outcomes of acute myocardial infarction, renal failure, coagulopathy and infection. | 2 | Permissive hypotension, hemorrhage, outcomes | |
| Tran (2018) | Permissive hypotension versus conventional resuscitation strategies in adult trauma patients with hemorrhagic shock | Meta-analysis of 5 trials evaluating permissive hypotension. The pooled odds ratio was 0.70, suggesting a survival benefit for permissive hypotension. Those patients received fewer blood products and had less estimated blood loss. | 3 | Hemorrhage, outcomes, target blood pressure | |
| Brown (2013) | Goal-directed resuscitation in the prehospital setting: a propensity adjusted analysis | In subjects without PH hypotension, HIGH crystalloid was associated with an increase in the risk of mortality and acute coagulopathy but not in subjects with PH hypotension. HIGH crystalloid was associated with correction of PH hypotension on ED arrival. Each 1 mm Hg increase in ED SBP was associated with a 2% increase in survival in subjects with PH hypotension. | 3 | Prehospital resuscitation, outcomes | 10.1097/ta.0000000000002702 |
| Tourniquet | |||||
| Schouroll (2015) | A multi-institutional analysis of prehospital tourniquet use | Tourniquets 89% effective in civilians, with lower ISS, mortality rates, and limb amputation rates than military patients. | 3 | Tourniquet | 10.1097/ta.0000000000000689 |
| Smith (2019) | Prehospital tourniquet use in penetrating extremity trauma: decreased blood transfusions and limb complications | Tourniquets associated with higher SBP on arrival, less PRBCs and FFP, fewer fasciotomies and amputations. No difference in nerve palsy. | 3 | Tourniquet | 10.1097/ta.0000000000002095 |
| McNickle (2019) | Effect of prehospital tourniquet on resuscitation in extremity arterial trauma | Tourniquets associated with higher HR, more transfusions, more amputations. No difference in length of stay or mortality. | 3 | Tourniquet | 10.1136/tsaco-2018-000267 |
| Inaba (2015) | Tourniquet use for civilian extremity trauma | Of 87 patients with tourniquets, there were 15 amputations, 1 of which was lifesaving but likely contributed to limb loss. No other complications directly attributed to tourniquet use. | 3 | Tourniquet | 10.1097/TA.0000000000000747 |
| Leonard (2015) | A multi-institutional study of hemostatic gauze and tourniquets in rural civilian trauma | Tourniquets 98% effective, with no attributable amputations | 3 | Tourniquet | 10.1097/TA.0000000000001115 |
| Scerbo (2016) | Safety and appropriateness of tourniquets in 105 civilians | Of the tourniquets, 90% were indicated, though less than half had a vascular injury. No complications resulting from tourniquet use. | 3 | Tourniquet | 10.1080/10903127.2016.1182606 |
| Scerbo (2017) | The trauma center is too late: major limb trauma without a prehospital tourniquet has increased death from hemorrhagic shock | Tourniquets associated with higher arrival SBP, fewer transfusions, and lower mortality from hemorrhagic shock | 3 | Tourniquet | 10.1097/TA.0000000000001666 |
| Teixeira (2018) | Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury | Tourniquets independently associated with survival with no difference in delayed amputation rates | 3 | Tourniquet | 10.1016/j.jamcollsurg.2018.01.047 |
| Wellme (2020) | Evaluating tourniquet use in Swedish prehospital care for civilian extremity trauma | Tourniquets 98% effective with 3% complication rate; 29% were possibly not indicated. | 3 | Tourniquet | 10.1007/s00068-020-01341-0 |
| Zeitlow (2015) | Prehospital use of hemostatic bandages and tourniquets: translation from military experience to implementation in civilian trauma care | Tourniquets 99% effective | 3 | Tourniquet | |
| Ode (2015) | Emergency tourniquets for civilians: can military lessons in extremity hemorrhage be translated? | No tourniquet-related complications. Patients with delayed/missed tourniquets had higher incidences of shock, admission, and transfusion. | 3 | Tourniquet | 10.1097/TA.0000000000000815 |
| Kue (2015) | Tourniquet use in a civilian emergency medical services setting: a descriptive analysis of the Boston EMS experience | Tourniquets 91% effective with 2% complication rate | 3 | Tourniquet | 10.3109/10903127.2014.995842 |
In this chapter, we provide an evidence-based appraisal of available recent literature regarding DCR techniques to describe the currently available evidence for cutting-edge care for patients in hemorrhagic shock. An appendix to this chapter is available with the studies included in this review.
In all, 102 articles from 2015 to 2020 were retrieved and stratified into to three classes according to the quality assessment instrument developed by the Brain and Trauma Foundation and adopted by the Eastern Association for the Surgery of Trauma ( www.east.org ). Classes ranging from I to III were assigned according to the strength of scientific evidence. Articles are summarized in the appendix that accompanies this chapter and can be found online. The evidence that was evaluated included studies addressing the following topics: prehospital transfusion, timing of resuscitation, TXA use, crystalloid use, prehospital tourniquet use, WB, MTPs, TEG-guided resuscitation, REBOA, vasopressin use for hemorrhagic shock, selective aortic arch perfusion (SAAP) and hybrid ER/OR (see Table 1 ).
Class I: Prospective randomized controlled trials, which are the gold standard of clinical trials. Some prospective randomized controlled trials, however, suffer from poor design, inadequate numbers, or methodologic inadequacies that are not clinically significant. There were 12 class I studies identified.
Class II: Prospective and retrospective analyses that were based on clearly reliable data. These types of studies include observational studies, cohort studies, prevalence studies, and case control studies. There were 20 studies within this category.
Class III: Mostly retrospectively collected data trials. Evidence used in this class includes clinical series, databases or registries, case reviews, case reports, and expert opinion. There were 70 studies identified within this category.
More than 60,000 civilian deaths due to hemorrhagic shock occur in the United States each year. It is estimated that worldwide, there are 1.5 million deaths annually due to hemorrhage as a result of trauma, and traumatic injury is the leading cause of death in people between the age of 1 and 44 years old. Importantly, because hemorrhagic shock from trauma disproportionately affects young people, nearly 75 million years of life are lost on a global level. Approximately half of these deaths occur in the prehospital setting and achieving timely bleeding control is a challenge faced in all trauma systems. The potential importance of moving the pendulum of hemorrhage control closer to the time of injury is apparent.
Unlike blood, time, once spent, is impossible to recover and cannot be replaced. More than any other modifiable risk factor, time may be the most vital factor when it comes to reducing preventable hemorrhage mortality after traumatic injury. As early as 1975, R. Adams Cowley observed that patients who experienced a delay in treatment suffered higher mortality. He subsequently coined the term “golden hour.” While the concept of the “golden hour” highlights the importance of early treatment, we now recognize that mortality from severe hemorrhage can occur in the first 20 to 35 minutes. Evaluating over 42,000 patients with torso injuries from the National Trauma Data Base, Alarhayem et al showed that mortality after severe truncal hemorrhage increased significantly with longer prehospital times. Furthermore, the risk of death was greatest within the first 30 minutes. The median transport time observed in their study was 37 minutes. Put directly, the risk of death was greatest before the patient ever reached the hospital.
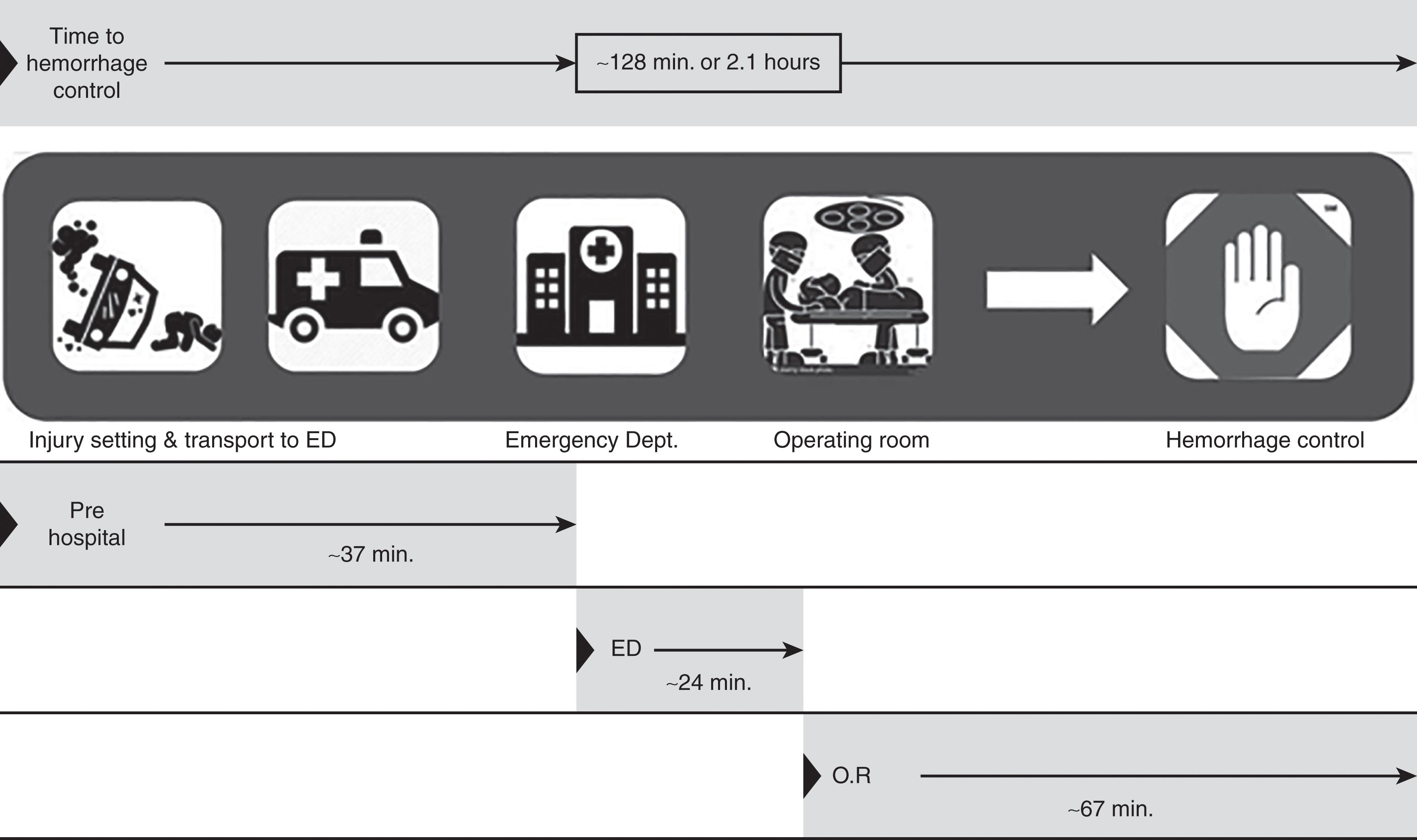
For the last 40 years, civilian emergency medical services (EMS) practice has been to “scoop and run” as opposed to “stay and play.” The existing paradigm is that the patient will receive definitive care at the hospital, and any delays that may arise as a result of prehospital care should be avoided. This practice has served its purpose for a large number of patients. Unfortunately, those that arrive to the hospital alive represent only the tip of the iceberg with a median hemorrhage control time of 2 hours from the time of injury to the time of surgical hemorrhage control ( Fig. 1 ). Special consideration is needed for the large proportion of patients who die as a result of hemorrhage prior to arrival. It is notable to consider that the in-hospital mortality for hypotensive patients in need of MTP (47%) has not changed in over last 12 years. These findings are indicative of a need for intervention at an earlier phase of care.
Fitting with the traditional airway, breathing, circulation (ABC) approach to emergency management, intubation is one of the most common prehospital procedures in the trauma population. It has been shown, however, that prehospital intubation of penetrating trauma patients does not demonstrate a survival benefit. Furthermore, for patients who survived to admission, prehospital intubation was associated with increased mortality and was not protective against a variety of in-hospital complications. Intubation in the setting of animal models of severe hemorrhagic shock has perhaps provided a look at the specific potential harms of prehospital intubation, specifically prior to volume resuscitation. Taghavi et al demonstrated that when compared with bag-valve-mask ventilation, intubation was associated with more profuse hemorrhage, worsened hypothermia, and higher lactate, raising the question of the benefits of intubation prior to effective volume resuscitation. This relationship between airway vs. circulation in the management of patients with severe hemorrhage has been an area of increased focus lately.
The ABC approach to trauma care “became the standard of care despite lack of scientific evidence.” In one study, Ferrada et al challenged the ABC paradigm, proposing, instead, that circulation should be the initial point of focus when treating a trauma patient (CAB approach). Looking at 245 patients who received intravenous blood product resuscitation prior to intubation (CAB) and 195 patients who were intubated prior to receiving volume resuscitation (ABC), Ferrada et al showed there was no statistically significant difference in mortality between the two groups. The group notes that this study highlights that many trauma centers are already initiating volume resuscitation prior to intubation. They further conclude that because of the noninferior mortality outcome of the CAB approach vs. the ABC approach, further prospective investigation is warranted. Studies are currently underway looking at exactly this phenomenon.
Fluid resuscitation is perhaps one of the most contentious points in the prehospital care debate. Current civilian EMS guidelines regarding prehospital fluid resuscitation are not consistently established. If there is a common traditional theme, it is that for systolic blood pressures less than 90 mm Hg, rapid bolus administration of normal saline or Ringer’s lactate should be initiated. Upon closer examination, however, the use of crystalloid solution may actually do more harm than good. Elevated blood pressure can potentially displace clots in patients with uncontrolled hemorrhage; the absence of clotting activity in crystalloid solutions can result in dilutional coagulopathy; and finally, the high chloride content of crystalloid solution may exacerbate the acidosis seen in shock.
A large-scale review from 2009 asked, among other questions, “If prehospital vascular access is obtained, should intravenous fluids be given?” The consensus reached was that no “convincingly justifiable recommendation based on available data” could be made. The study did, however, come to the conclusion that a “reasonably justifiable recommendation” could be made to withhold intravenous fluids in the prehospital setting for patients with penetrating torso injuries, strategies supported by the historical permissive hypotension study from Bickell.
Tourniquet use to control hemorrhage after extremity trauma has been described for hundreds of years, though it fell out of favor for much of the 20th century due to concerns about prolonged tourniquet times leading to iatrogenic injuries including limb ischemia and amputations. However, the conflicts in Iraq and Afghanistan in the early 21st century provided an opportunity for resurgence of battlefield tourniquet use with good results, including several studies in 2008 and 2009 that demonstrated that tourniquets effectively controlled hemorrhage and improved mortality without increasing complications. Renewed interest in civilian tourniquet use shortly after has continued over the past decade with increasing tourniquet use by EMS and police forces in the United States as well as recommendations by the Hartford Consensus in 2013 that tourniquets be utilized by first responders and even laypersons in a mass casualty event, culminating in the rollout of the American College of Surgeons’ Stop the Bleed program in 2017 to teach hemorrhage control techniques including tourniquet application on a broad scale to the public.
Several recent studies have been conducted attempting to evaluate tourniquet use in civilian populations; however, most of these studies have been limited to retrospective database reviews. Most of the initial studies attempted to describe tourniquet efficacy and safety in civilian populations. In 2015 and 2016, several small retrospective reviews by Zietlow et al, Kue et al, Leonard et al, and Inaba et al evaluated the emerging tourniquet use, finding the tourniquets effectively controlled extremity hemorrhage in 89%–98% of patients. These early studies also attempted to describe amputation and other complication rates and generally describe low rates of complications attributable to tourniquet use. Scerbo and colleagues conducted a retrospective review of 105 patients with prehospital tourniquets at a Level I trauma center between 2008 and 2013 and felt that 90% had appropriate indications for placement; they found that this group had a higher amputation rate (32% vs. 0%, p = 0.03) and nerve palsy rate (5% vs. 0%, p = 0.57) than the nonindicated group, concluding that tourniquets were safe and generally appropriately applied in civilians. The largest study from 2015 was a multi-institutional retrospective review by Schouroll and colleagues, which included 197 patients with prehospital tourniquets presenting to 9 Level I trauma centers between 2010 and 2013. They redemonstrated a high efficacy rate of hemorrhage control at 89%, a nerve palsy rate of 6.1%, and amputation rate of 18%, none of which was felt to be directly attributable to tourniquet use. However, the patients were found to be less severely injured than those described in previous military studies, with lower amputation rates and mortality rates, so concern persisted about whether military data could be extrapolated to civilian populations.
More recent studies have attempted to compare tourniquet use to nonuse and determine the effect on outcomes. A second study by Scerbo et al in 2017 compared patients with prehospital tourniquets to those with tourniquets placed at the trauma center and found that prehospital tourniquet use was associated with increased systolic blood pressure at arrival to the hospital (125 vs. 101 mm Hg, p < .001), decreased incidence of blood transfusion (34% vs. 55%, p = 0.02), and decreased mortality from hemorrhagic shock (3% vs. 14%, p = 0.01). The following year, the multicenter “Texas Tourniquet Study” compared prehospital tourniquet use vs. nonuse in 1026 patients with peripheral vascular injury at 11 trauma centers from 2011 to 2016; they found that 181 patients (17.6%) had prehospital tourniquet placement; there was no crude mortality difference (3.9% vs. 5.2%, odds ratio [OR] 1.35, p = 0.452). However, on multivariate analysis prehospital tourniquet use was independently associated with survival (adjusted OR 5.86; 95% confidence interval [CI] 1.41–24.47, adjusted p = 0.015) with similar delayed amputation rates between the two groups (1.1% vs. 1.1%, adjusted OR 1.82, 95% CI 0.36–9.99; adjusted p = 0.473). And finally, a retrospective review by Smith and colleagues of 204 patients with prehospital tourniquets matched to 127 without found prehospital tourniquets were associated with higher systolic blood pressure on arrival to the trauma center (120 vs. 112 mm Hg, p = 0.003), fewer PRBC blood and fresh frozen plasma (FFP) transfusions (2.0 vs. 9.3, p < 0.001) and (1.4 vs. 6.2, p < .001), and lower amputation rates (0.8% vs. 9.1%, p = 0.005).
The previously discussed studies suggest that prehospital tourniquet use in civilian populations is generally safe, effective, and associated with decreased shock, blood transfusion needs, and mortality, and prehospital tourniquet use has been widely adopted as an essential component of DCR for civilians with extremity hemorrhage. However, all studies so far have been Level 3 data consisting of retrospective reviews of registry data; higher-quality studies including prospective data collection are necessary to improve our understanding of civilian prehospital tourniquet use.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here