Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The treatment of telangiectasias was not seriously attempted until the 1930s, with Biegeleisen taking the credit for initially attempting an injection into the perivascular space around telangiectatic areas. Later, he implemented intravascular injections using homemade microneedles. These early efforts led to disappointing results, primarily because the sclerosing solutions, such as sodium morrhuate, were very caustic. It was not until the 1970s that others attempted to treat spider telangiectasias with intravascular injection using less caustic solutions such as sodium tetradecyl sulfate (STS) (Sotradecol) and hypertonic saline. It was these agents that propelled the treatment of telangiectasias forward. The enthusiasm for these treatments increased steadily as Foley's publication, relating to this new technique, gained momentum.
Although research continues to be done in this area, there is consensus today that telangiectasias can result from many causes, alone, or more likely in combination with other etiologic factors. Telangiectatic leg veins, according to the contemporary research, arise as a result of venous hypertension secondary to a number of different causes and conditions. The etiology of varicose veins and telangiectasias, for the most part, is similar. The pathophysiology of telangiectasias is usually broadly categorized as genetic/congenital, acquired, and iatrogenic. Some of the genetic causes of telangiectasias include nevus flammeus (port-wine stains), nevus araneus (spider telangiectasia, which can also result from acquired diseases), and Klippel-Trenaunay syndrome. Congenital conditions associated with telangiectasias include Maffucci syndrome and Rothmund-Thomson syndrome (poikiloderma). Acquired causes of telangiectasias can arise from a primary cutaneous disorder, such as varicose veins and keratosis lichenoides chronica, or the result of a disorder with a secondary cutaneous component, such as lupus erythematosus, a collagen disorder, and mastocytosis (telangiectasia macularis eruptiva perstans). Hormonal influences (estrogen and progesterone) also play a role in the pathogenesis of telangiectasia. Pregnancy places the person at risk for the development of telangiectasia as early as a couple of weeks after conception. Birth control pills, menses, and the time just before ovulation are also associated with the development or worsening of telangiectasia and increased venous dispensability. Topical steroids, particularly at high doses, have also been identified as a possible causative factor. Lastly, physical insults, such as trauma (contusions) and infection, have also been implicated as causal forces. See Box 23.1 for a comprehensive listing of the many causes of lower-leg cutaneous telangiectasia.
Vascular nevi
Nevus flammeus
Klippel-Trenaunay syndrome
Nevus araneus
Angioma serpiginosum
Bockenheimer syndrome
Maffucci syndrome
Congenital poikiloderma (Rothmund-Thomson syndrome)
Essential progressive telangiectasia
Cutis marmorata telangiectatica congenita
Diffuse neonatal hemangiomatosis
Acquired disease with a secondary cutaneous component
Lupus erythematosus
Dermatomyositis
Progressive systemic sclerosis
Cryoglobulinemia
Telangiectasia macularis eruptiva perstans (mastocytosis)
Human T-lymphotrophic virus type III (HTLV-III)
Varicose veins
Keratosis lichenoides chronica
Necrobiosis lipoidica diabeticorum
Capillaritis (purpura annularis telangiectodes)
Malignant atrophic papulosis (Degos disease)
Pregnancy
Estrogen therapy
Topical corticosteroid preparations
Actinic neovascularization and/or vascular dilation
Trauma
Contusion
Surgical incision/laceration
Generalized essential telangiectasia
Progressive ascending telangiectasia
Human T-lymphotrophic virus type III (HTLV-III)
Radiodermatitis
Erythema ab igne (heat/infrared radiation)
Telangiectasia is also associated with a number of other conditions and traits. These include, but are not limited to, those listed here:
Age (peaks during age 50 to 69 years)
Female gender
Occupation and lifestyle: sedentary occupations and lifestyles are associated with telangiectasia
Diseases such as cirrhosis
Excessive exposure to the sun
Therapeutic radiation ( Figs. 23.1–23.8 ).
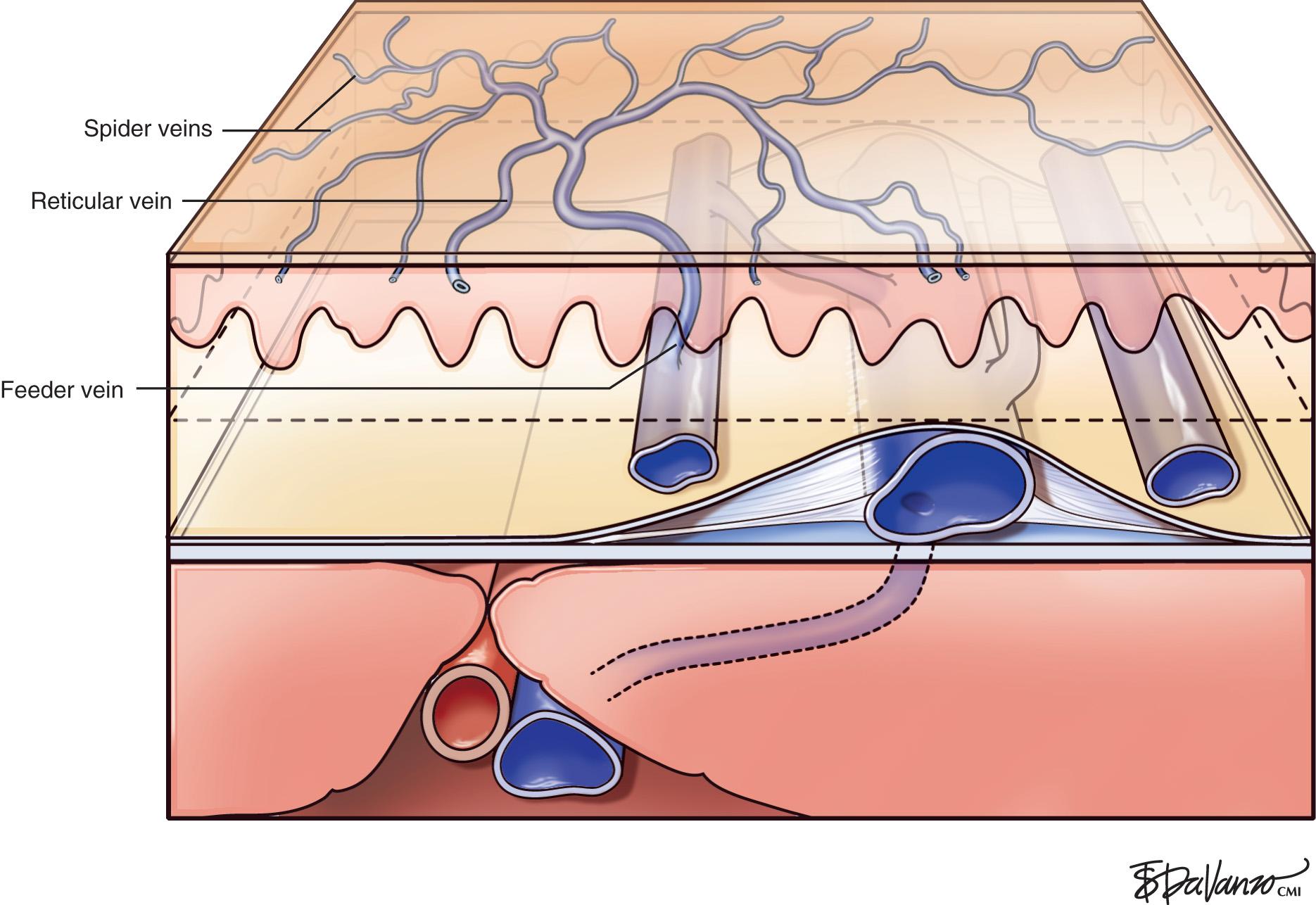







Patients with spider telangiectasias typically present with primarily cosmetic complaints. Patient selection for the treatment of spider telangiectasias, as with all medical treatments, begins with a thorough assessment, which includes not only an assessment of the person's telangiectasia, but also the medical history, chief complaint, family history, and the patient's expectations relating to their possible spider telangiectasias. Based on this assessment, the physician must determine whether or not the treatment can resolve the patient's cosmetic complaints. At times, the telangiectasia is the result of a more generalized, systemic problem such as venous insufficiency. If venous insufficiency is present, it must be treated before the treatment of spider telangiectasia; otherwise, the venous hypertension would likely thwart the desired outcome. Second, determine whether or not the patient's expectations are realistic and achievable. The patient must clearly understand that the treatment is elective and that it is not likely to produce any significant health benefits. The patient should also understand that multiple treatments are often necessary for optimal results. Some patients may not be willing to do this. As with all invasive procedures, the patient must be educated about the benefits, risks, and alternatives to treatment. They must be thoroughly aware of all potential adverse sequelae and possible complications. Last, the patient must be informed that the treatment of spider telangiectasias is not curative and that further development of telangiectatic areas is likely.
Although there are no absolute contraindications to this treatment, people taking certain medications and/or patients with some chronic illnesses, especially those that could affect the occurrence of sclerotherapy complications, should be approached with extreme caution. For example, conditions including diabetes and peripheral vascular disease may lead to serious complications, such as ulcers. Some medications, for example, minocycline or isotretinoin, can lead to adverse reactions if not discontinued before the treatment.
The basic endovascular instrumentation used for the treatment of spider telangiectasias includes needles for access and syringes to deliver the sclerosant to the affected areas. The needles used for telangiectasia are typically 30-gauge, although a 27-gauge butterfly needle may be used sometimes for larger reticular veins. Smaller needles, as small as a 33 gauge, can also be used, but they tend to bend too easily when they are penetrating the skin ( Fig. 23.9 ).

The syringes that are typically used vary from a 1-mL tuberculin syringe to a 3-mL syringe. Most prefer a 3-mL syringe because it exerts the lowest pressures during injection, and it is also manually manipulated more precisely by the practitioner than a 1-mL syringe, especially if it is only filled to 2 mL.
The environment of care for sclerotherapy should include a comfortable table for the patient, a comfortable room temperature, and ample lighting. The treatment table height should permit the physician to sit comfortably on a stool with their legs under the table, without having to lean over the table and the patient for access. Environmental lighting should be bright and capable of providing adequate indirect illumination without any glare on the patient's skin ( Fig. 23.10 ).

General supplies would include alcohol swabs, cotton balls, tape, and compression supplies such as ACE wraps or Coban. Patients can supply their own stockings, or they can be provided by the practice, which would require keeping a fairly large inventory ( Figs. 23.11 and 23.12 ).


Last, but also most important, is emergency equipment. Fortunately, life-threatening complications are very rare; however, they are always possible. Basic emergency equipment must minimally include oxygen, airway equipment, epinephrine, steroids, and antihistamines ( Fig. 23.13 ).

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here