Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
In congenital sensorineural hearing loss, approximately 20% of inner ears demonstrate a radiographically detectable abnormality.
Many patterns of deformity appear to result from disturbances in the embryogenesis of the inner ear during the first trimester.
Enlargement of the vestibular aqueduct is the most common anomaly, followed in frequency by semicircular canal and cochlear malformations.
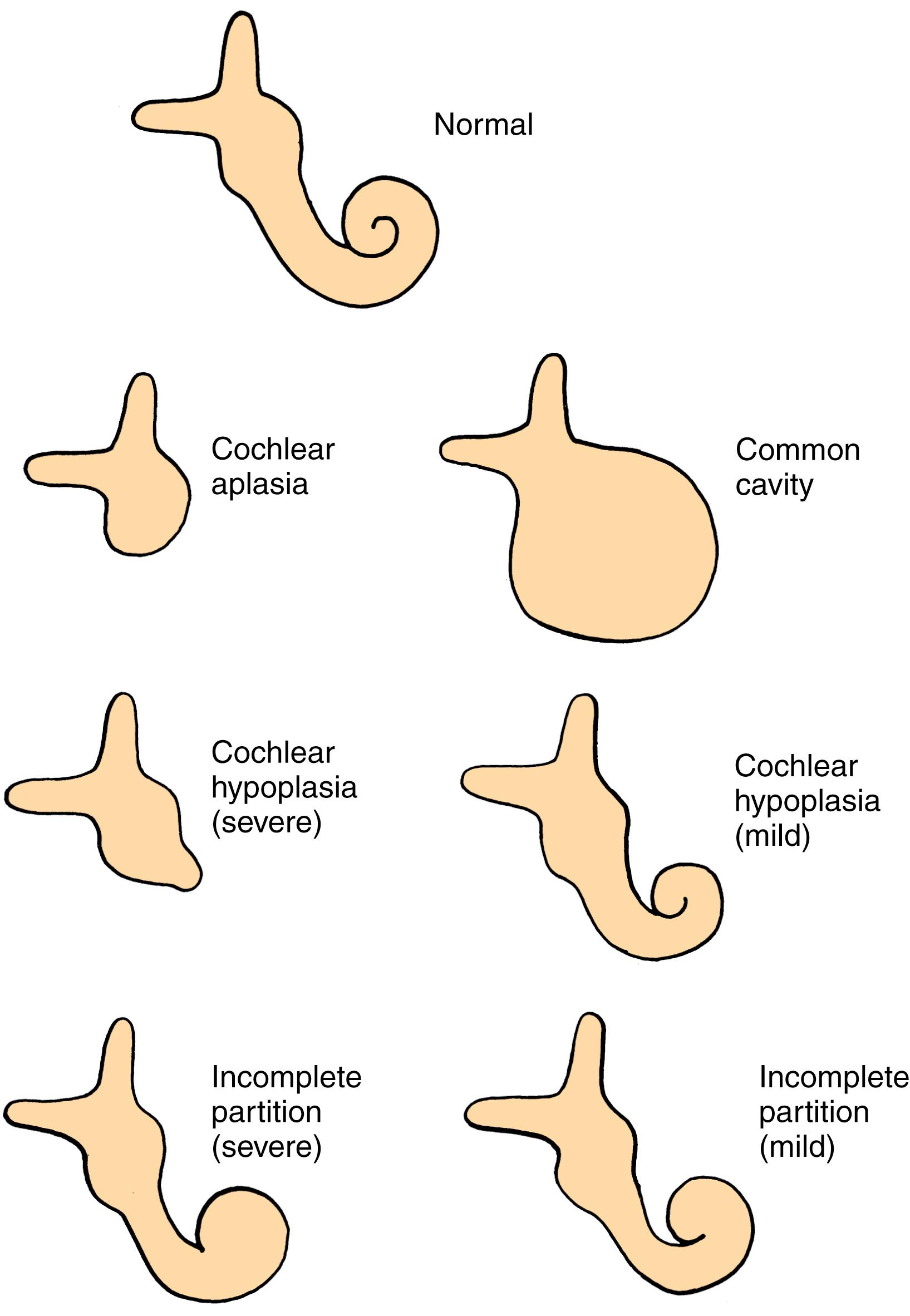
Cochlear anomalies apparent on imaging include aplasia, hypoplasia, incomplete partition, and common cavity.
Semicircular canals may be absent (aplastic) or deformed (dysplastic).
The eighth cranial nerve may be aplastic or hypoplastic, especially when the internal auditory canal is narrow. Similarly, the cochlear nerve alone may be aplastic and hypoplastic, associated with bony stenosis/atresia of the cochlear aperture.
Congenital ear malformations may be a feature of syndromes such as Pendred syndrome, branchio-oto-renal syndrome, CHARGE ( c oloboma, h eart defects, a tresia of the choanae, r etardation of growth and development, g enital abnormalities, and e ar abnormalities or hearing loss) syndrome, and various trisomies.
High-resolution T2-weighted magnetic resonance imaging (MRI) is superior to computed tomography (CT) for demonstration of the endolymphatic sac, eighth cranial nerve, and brain parenchyma.
Hearing loss associated with milder deformities is variable but tends to worsen over time.
Stapes surgery for pseudoconductive hearing loss carries a high risk for anacusis and occurrence of cerebrospinal fluid (CSF) “gusher.”
Predilection for stapes gusher caused by modiolar defects may be inherited in an X-linked pattern.
Head trauma in patients with congenital cochleovestibular malformations may cause sudden decrease in hearing, transotic CSF leak, and recurrent meningitis.
Surgery on the endolymphatic sac or middle ear windows has not been shown to improve or stabilize hearing.
Several molecular diagnostic tools for genetic testing are available to complement imaging modalities.
Cochlear implantation in ears with congenital malformations is usually successful but carries a small heightened risk for CSF leak, meningitis, and facial nerve stimulation.
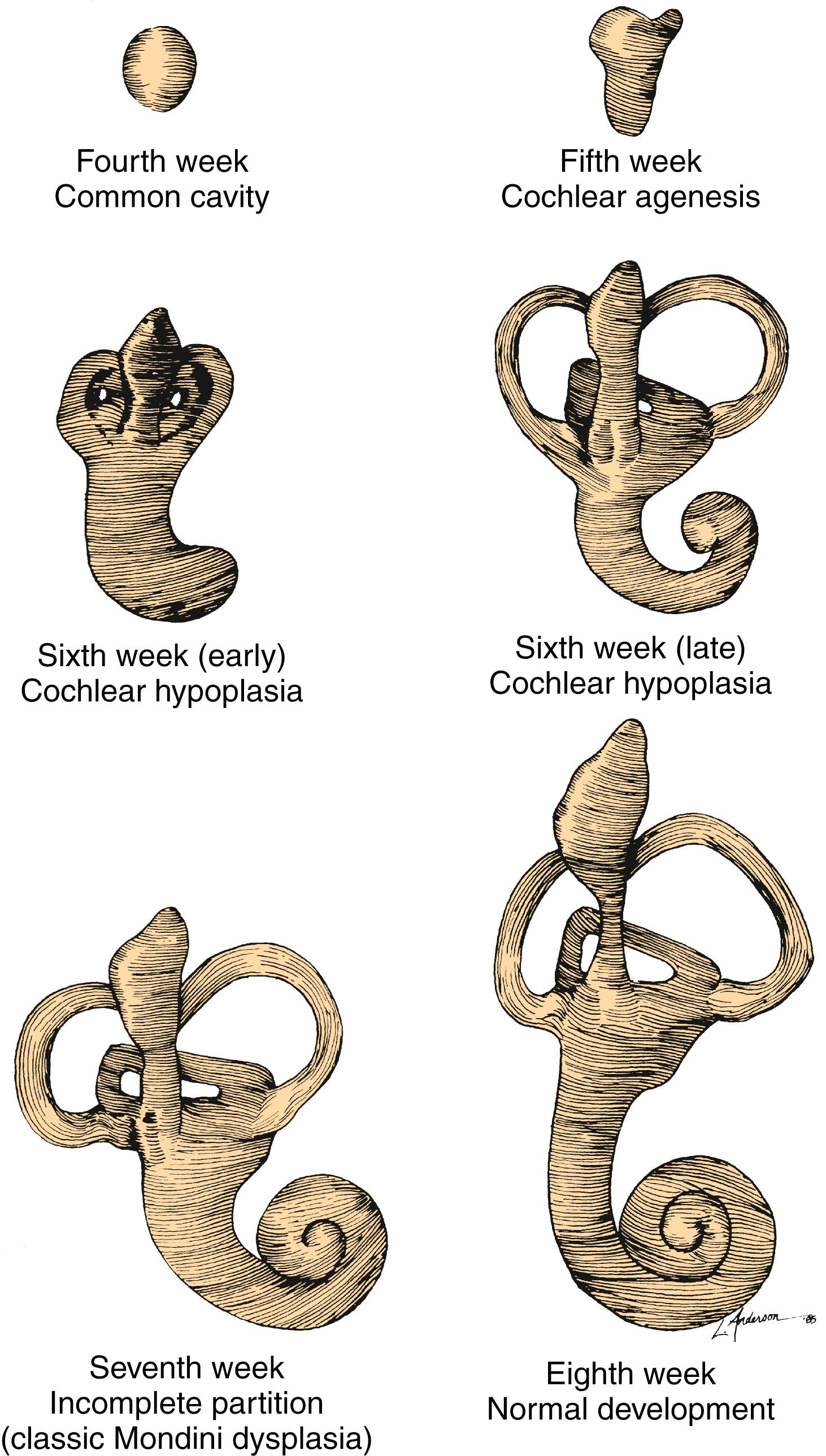
Development of the inner ear begins early in embryogenesis. By the end of the eighth week, the membranous labyrinth has assumed its characteristic convoluted shape. Gradual ossification of the otic capsule develops around the membranous labyrinth and is complete by birth. Maturation of the sensory epithelium occurs long after formation of the membranous labyrinth, during the late second and early third trimesters. By weeks 26 to 28 of gestation, hair cell and auditory neural development are largely complete. Thus the normal human fetus may be able to hear 2.5 to 3 months before birth.
Most inner ear malformations arise when formation of the membranous labyrinth is interrupted during the first trimester of pregnancy. This interruption may be either a result of an inborn genetic error or a consequence of a teratogenic/infectious exposure during the period of inner ear organogenesis between the fourth and eighth weeks of gestation. Genetic conditions may manifest as sensorineural hearing loss (SNHL) alone (nonsyndromic) or be associated with any of a number of syndromes. A partial list of syndromes associated with radiologically detectable inner ear malformation includes Pendred, Waardenburg, Apert, Wildervanck (cervico-oculoacoustic), branchio-oto-renal, and Alagille syndromes. Nonsyndromic familial inner ear malformations have also been described. , Teratogenic influences known to affect inner ear organogenesis include in utero viral infections (e.g., rubella, human cytomegalovirus infection), chemical teratogens (e.g., thalidomide), and radiation exposure. Abnormalities in otic capsule structure and deficiencies in the organ of Corti appear to arise as secondary effects of earlier errors in development of the membranous labyrinth. Derangement of the otic capsule ossification process alone does not appear to be a major mechanism in congenital hearing loss. Ossification of the labyrinthine lumen, however, is a common finding in early acquired deafness, typically arising as a consequence of meningitis.
Developmental damage to cochlear structure and function is not restricted to agents that cause gross structural malformations. Even in doses lower than those that would be ototoxic in the adult, aminoglycoside antibiotics administered in the first trimester of pregnancy cause severe hearing loss in humans and several other species. This time frame corresponds to the maturation of the outer hair cells and initiation of the cochlear potentials. In 35 of the infants delivered by 72 women who received streptomycin prophylaxis for tuberculosis during the first 4 months of pregnancy, auditory deficits ranging from minor high-frequency threshold elevations to severe bilateral SNHL were noted. The risk is not restricted to the first trimester; even at low doses, slight hearing losses were noted when aminoglycoside antibiotics were administered during the human equivalent of the last two trimesters of pregnancy. These findings have obvious implications for use of these drugs in pregnant women and in premature infants who have not yet reached functional cochlear maturity.
Congenital anomalies of the inner ear may be considered in two broad categories: malformations with pathologic changes limited to the membranous labyrinth and malformations that involve both the osseous and membranous portions of the labyrinth. Only malformed otic capsules are evident on inner ear radiographs and thus detectable during life. By inference, children with congenital SNHL and radiographically normal inner ears may be assumed to possess anomalies limited to the membranous labyrinth or neural pathways. Although several types of membranous deformities have been described, their classification is not yet of clinical use because differentiation requires histopathologic examination. Among the deformities that affect the otic capsule, a variety of morphologic patterns may be recognized radiographically, and classification may have prognostic and even therapeutic importance.
Most children with congenital SNHL, with the possible exception of auditory neuropathy, would have detectable abnormalities in their inner ears if they could be examined histologically. Because even most children with profound bilateral SNHL have radiographically normal inner ears, it can be inferred that malformations limited to the membranous labyrinth predominate. The reported incidence of malformations varies, depending on the hearing level of the study population, the sophistication of imaging used, and the definition of abnormality used by the observer. As a rule of thumb, approximately 20% of cases of congenital SNHL will demonstrate inner ear malformations with modern imaging technology. In a series of 234 children who had SNHL of varying degrees of severity, Reilly found cochlear anomalies in only 4% of those evaluated by high-resolution computed tomography (CT). With improvements in CT imaging technology and greater awareness of inner ear deformities, Antonelli and colleagues found anomalies in 31% of 157 children with SNHL of variable degree. In another CT study, anomalies were found in 17% of 185 ears of children with SNHL and none of the ears of 309 children without SNHL. A large Korean study found a 22% incidence of anomalies on radiologic imaging in 590 ears with profound SNHL. Although it has been shown that the genetic etiologies of hearing loss can vary greatly among different ethnic groups, large cohorts of hearing loss patients from China and Korea showed similar incidences of anomalies (20% to 22%). , The use of magnetic resonance imaging (MRI) as an alternative diagnostic tool for congenital hearing loss has gained prominence, particularly when the integrity of the cochlear nerve is in question. , In fact, a systematic review found that MRI may be as sensitive as CT at detecting enlarged vestibular aqueduct (VA) and cochlear abnormalities.
The incidence of deformities of the semicircular canals (SCCs) and inner ear aqueducts has been less well studied than that of cochlear deformities. In a series of patients with radiographically detectable malformations of the inner ear, the cochlea was involved in 76%, the SCCs were involved in 39%, and the VA was affected in 32% of ears. The total is more than 100%, because many cases demonstrate abnormalities of more than one portion of the inner ear. A heightened awareness of enlarged vestibular aqueduct (EVA), combined with the greater sensitivity of axial CT scans in demonstrating this deformity, has led to a substantial increase in its detection. The rapid accrual of cases by clinicians interested in inner ear malformations suggests that EVA will ultimately prove to be the most common radiographically detectable inner ear anomaly.
Among deaf children with radiographically normal inner ears, histopathologic studies indicate that cochleosaccular dysplasia (Scheibe dysplasia) is by far the most common deformity. Because of the paucity of pathologic specimens available for examination, it is impossible to estimate the relative frequency of the various membranous malformations.
The traditional nomenclature used to describe congenital anomalies of the inner ear involves a confusing array of eponyms that stem from the first reports of the various morphologic patterns, usually by 18th- or 19th-century authors. In this chapter, a descriptive classification system is used, along with the traditional eponymous terminology, to improve the logic, ease of learning, and clinical relevance ( Box 13.1 ). The classification of membranous malformations is based on histopathologic changes in the inner ear; radiographic appearance is used to distinguish the combined osseous-membranous deformities. Correct use of the terminology of pathoembryology is important, although these terms frequently are applied imprecisely in the earlier literature. Key terms are aplasia (complete lack of development), hypoplasia (incomplete development), and dysplasia (aberration in development). The classification scheme used in this chapter has proved to be of practical clinical use and has been employed in most modern published studies. Other classification schema that categorize observed anomalies have been proposed.
Complete membranous labyrinthine dysplasia
Limited membranous labyrinthine dysplasia
Cochleosaccular dysplasia (Scheibe)
Cochlear basal turn dysplasia
Complete labyrinthine aplasia (Michel)
Cochlear anomalies
Cochlear aplasia
Cochlear hypoplasia
Incomplete partition (Mondini)
Common cavity
Labyrinthine anomalies
Semicircular canal dysplasia
Semicircular canal aplasia
Aqueductal anomalies
Enlargement of the vestibular aqueduct
Enlargement of the cochlear aqueduct
Internal auditory canal anomalies
Narrow internal auditory canal
Wide internal auditory canal
Eighth cranial nerve anomalies
Hypoplasia
Aplasia
In malformations limited to the membranous labyrinth, which account for more than 90% of cases of congenital deafness, the bony labyrinth is normal. In its most severe form, membranous dysplasia involves the entire labyrinth, including the cochlea, SCCs, utricle, and saccule. A limited form of membranous labyrinthine dysplasia, involving only a portion of the inner ear, also has been described.
Complete membranous labyrinthine dysplasia was first described by Siebenmann and Bing and is extremely rare. It has been reported in association with Jervell and Lange-Nielsen and Usher syndromes.
Incomplete development of the pars inferior is the most frequent histopathologic finding in congenital deafness. It was first described by Scheibe and commonly is known as cochleosaccular dysplasia. The spectrum of pathologic findings in this anomaly, which is confined to the cochlea and the saccule, has been well described. , The organ of Corti is either partially or completely missing. The cochlear duct usually is collapsed, with Reissner membrane adherent to the limbus. Less commonly, the duct is distended, presumably as a result of endolymphatic hydrops. The stria vascularis is typically degenerated and may contain colloidal inclusions. Schuknecht described characteristic strial changes consisting of aplasia alternating with regions of hyperplasia and gross deformity. Cochlear changes may be severe in the basal turn and gradually lessen in intensity toward the apex, or they may be severe throughout. The saccule usually is collapsed and has degenerated sensory epithelium. In cochleosaccular dysplasia, the SCCs and utricle are normal. Auditory neuronal survival is variable but may remain normal into adulthood, at least in some cases. Cochleosaccular dysplasia also has been demonstrated in a number of animal species, including the deaf white cat, Dalmatian dogs, and various mouse mutants. ,
Congenital anomalies of the inner ear that deform the otic capsule are of special interest to the clinician because they may be recognized and differentiated during life through radiographic imaging. As discussed previously, only approximately 20% of congenitally deaf people demonstrate radiographically anomalous inner ears. The clinical manifestations and natural history of these deformities are highly variable. Although some patients are deaf from birth, most maintain some residual hearing into adulthood. Slowly progressive deterioration of hearing during childhood, with eventual stabilization, is common, whereas fluctuating hearing loss is unusual. Sudden decrements in hearing are frequent and may appear to be spontaneous or may be triggered by even minor head trauma. Presumably, most of these cases are due either to internal fistulization secondary to membrane rupture within the cochlea, with admixture of perilymph and endolymph, or to external fistulization to the middle ear. Endolymphatic hydrops is an atypical finding. In some patients, hearing may be best preserved in very high frequencies (>8000 Hz), which are not measured by conventional audiometry. Residual ultraaudiometric hearing should be suspected in hearing-impaired children who manifest substantially better auditory function than would be predicted by pure-tone results in the speech frequencies. Occasionally, malformation of the inner ears may be associated with normal hearing, , especially for SCC anomalies. Vestibular symptoms, occasionally severe, are present in approximately 20% of patients. Retardation of motor development has been documented in some children with malformed inner ears, particularly those in whom SCCs are absent. A few patients experience vertigo when exposed to loud sounds, which is known as the Tullio phenomenon, presumably through a third window mechanism.
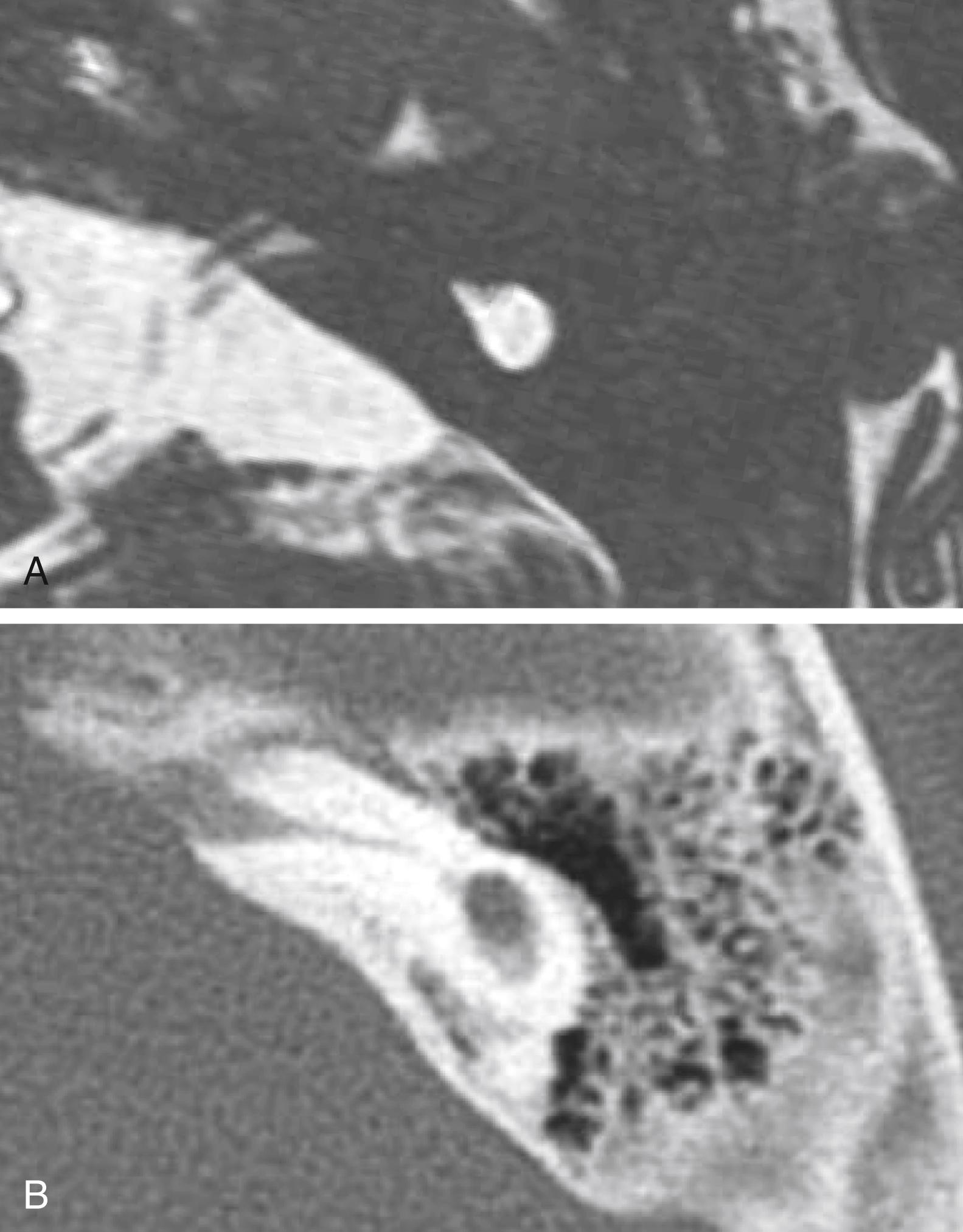
A wide variety of morphologic patterns of inner ear malformation has been observed radiographically and may involve the cochlea, SCCs, or VA ( Fig. 13.1 ). , Similar diversity has been observed on histologic analysis. , A majority of combined osseous and membranous malformations appear to arise from a premature arrest in the development of one or more components of the inner ear ( Fig. 13.2 ). The strongest evidence for this theory comes from the resemblance of most malformed inner ears to the appearance of the inner ear during embryogenesis, particularly between the fourth and eighth weeks of gestation. As a general rule, the earlier the developmental arrest, the more severe the deformity and the worse the hearing will be.
Other anomalies cannot be explained by a premature arrest in development alone and appear to arise from an aberrant embryologic process. An example of this type of anomaly is a cochlea of normal length but abnormal size or coiling geometry. In humans, the inner ear is of adult size at birth and shows little radiographic variation in size among individuals. However, histopathologic studies of human temporal bones demonstrate remarkable variability by as much as 1.5 mm in height; cochlear duct length ranges from 25 to 45 mm. Pappas and colleagues suggested that some children with congenital SNHL and apparently normal inner ear morphology on CT possess subtle abnormalities in the dimensions of inner ear structures. They hypothesize that such dimensional variations arise from a teratogenic insult during the second or third trimester, after the membranous labyrinth has formed but before it has reached adult size. Other studies have demonstrated that inner ear dimensions of children and some adults with SNHL do indeed differ from those with normal hearing despite overall normal gross appearance. These observations may potentially be used in the design of cochlear implants for patients with SNHL and grossly normal cochlea; however, further investigation is warranted.
Whereas some inner ear malformations involve only one portion of the inner ear, many patients have a combination of anomalies involving more than one component. Between the fourth and fifth weeks of development, the spheric otic cyst develops three buds that ultimately form the cochlea, SCCs, and VA (see Fig. 13.2 ). An inner ear malformation may be limited to one of these anlages, involve a combination of two, or even affect all three.
The frequent coexistence of deformities involving the cochlea, SCCs, and VA has several possible explanations: (1) the anomaly is genetically predetermined; (2) an insult to the embryo occurred before the fifth week; or (3) each of the buds was susceptible to some teratogenic influence at a later stage of development. A majority of inner ear malformations are bilateral and symmetric. In cases in which radiographs detect an anomaly on only one side, the opposite “normal” inner ear has a hearing loss in approximately 50% of cases.
Before the evolution of high-resolution imaging technology, clinicians and histopathologists alike tended to categorize these malformations together under the term Mondini dysplasia, after the first report by Carlo Mondini. We are indebted to the late Dr. Peter Phelps and Latin scholar Gordon Hartley for an English translation of Mondini’s original article. Mondini presented his work before the Academy of Sciences of the University of Bologna, describing the inner ear findings in a deaf 8-year-old boy who was struck on the foot by a wagon and later died of gangrene. The cochlea possessed only 1.5 turns and had a hollow apical cavity. An enlarged vestibule and VA also were noted. This deformity is the most common form of cochlear anomaly ( Table 13.1 ). Although numerous other distinct anatomic patterns of inner ear malformation are discernible radiographically and histologically, many clinicians continue to use the term Mondini dysplasia to describe them all. To avoid a confusing and overly broad nomenclature system, this designation is best reserved for the particular subtype of cochlear malformation first described by Mondini, whether or not it is associated with other inner ear malformations.
| Malformation | Incidence (%) |
|---|---|
| Incomplete partition (Mondini dysplasia) | 55 |
| Common cavity | 26 |
| Cochlear hypoplasia | 15 |
| Cochlear aplasia | 3 |
| Complete labyrinthine aplasia (Michel aplasia) | 1 |
The most severe deformity of the membranous and osseous labyrinth, complete labyrinthine aplasia, was first described by Michel. Presumably, a developmental arrest occurs before the formation of an otic vesicle, resulting in a complete absence of inner ear structures. As the otic capsule is entirely absent ( Figs. 13.3–13.5 ), these ears are, of course, uniformly deaf. Complete labyrinthine aplasia has been reported in association with anencephaly and thalidomide exposure. , An association with external ear abnormalities has also been reported. A purported case of Michel aplasia actually described a cystic inner ear of the common cavity type. This is but one example of the inaccurate use of traditional eponyms—a frequent occurrence in the literature. Complete labyrinthine aplasia is exceedingly rare, but the incidence is overestimated in the radiographic literature because it is confused with labyrinthine ossification. In the latter condition, which usually is acquired during life, a sizable and dense otic capsule is evident radiographically.
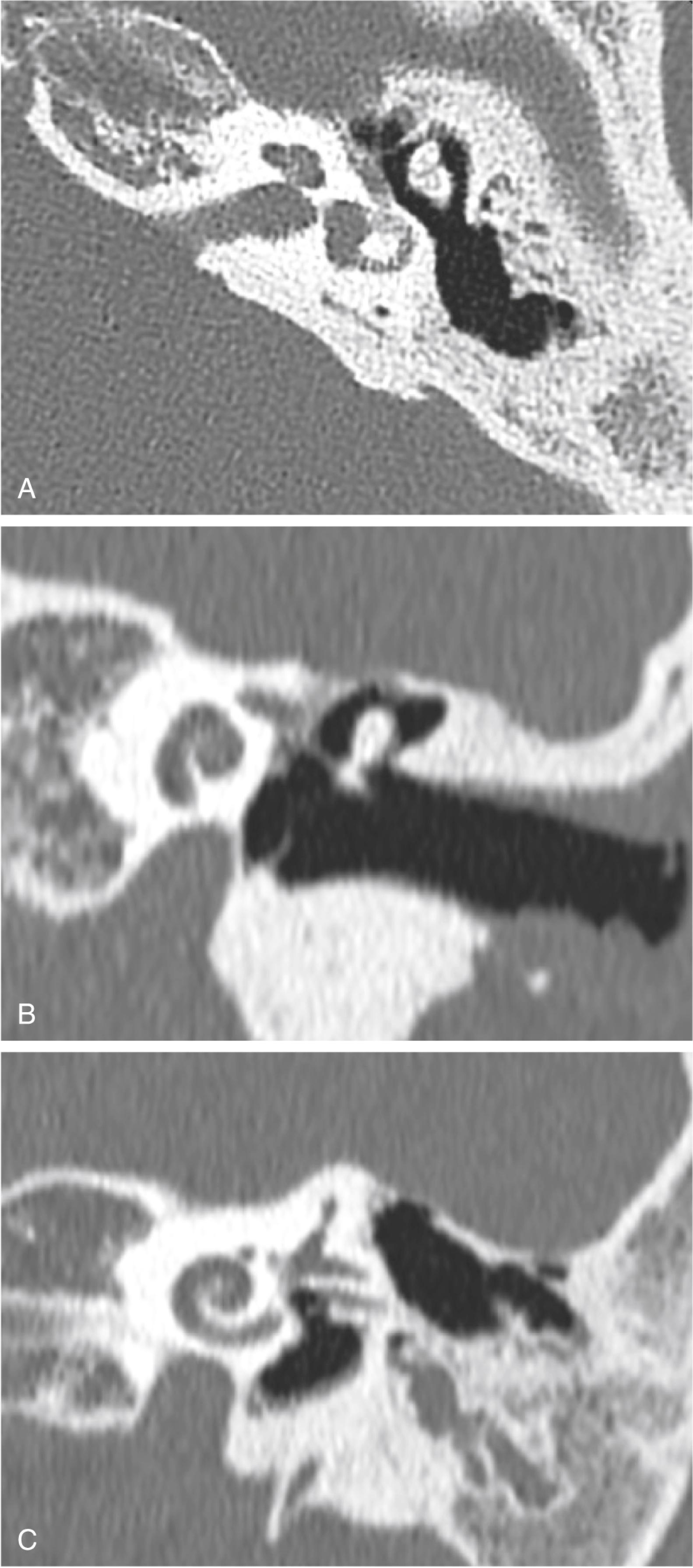
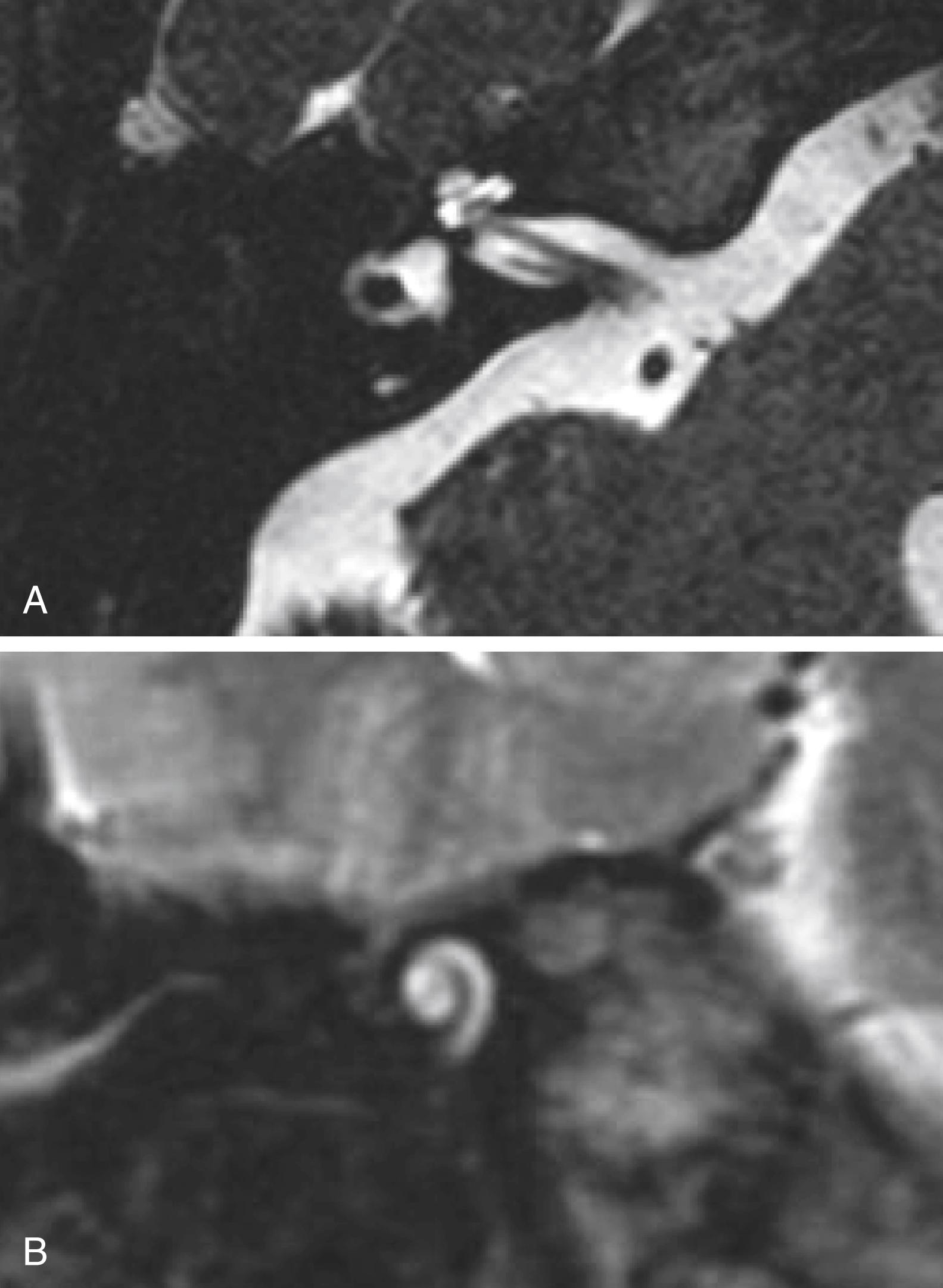
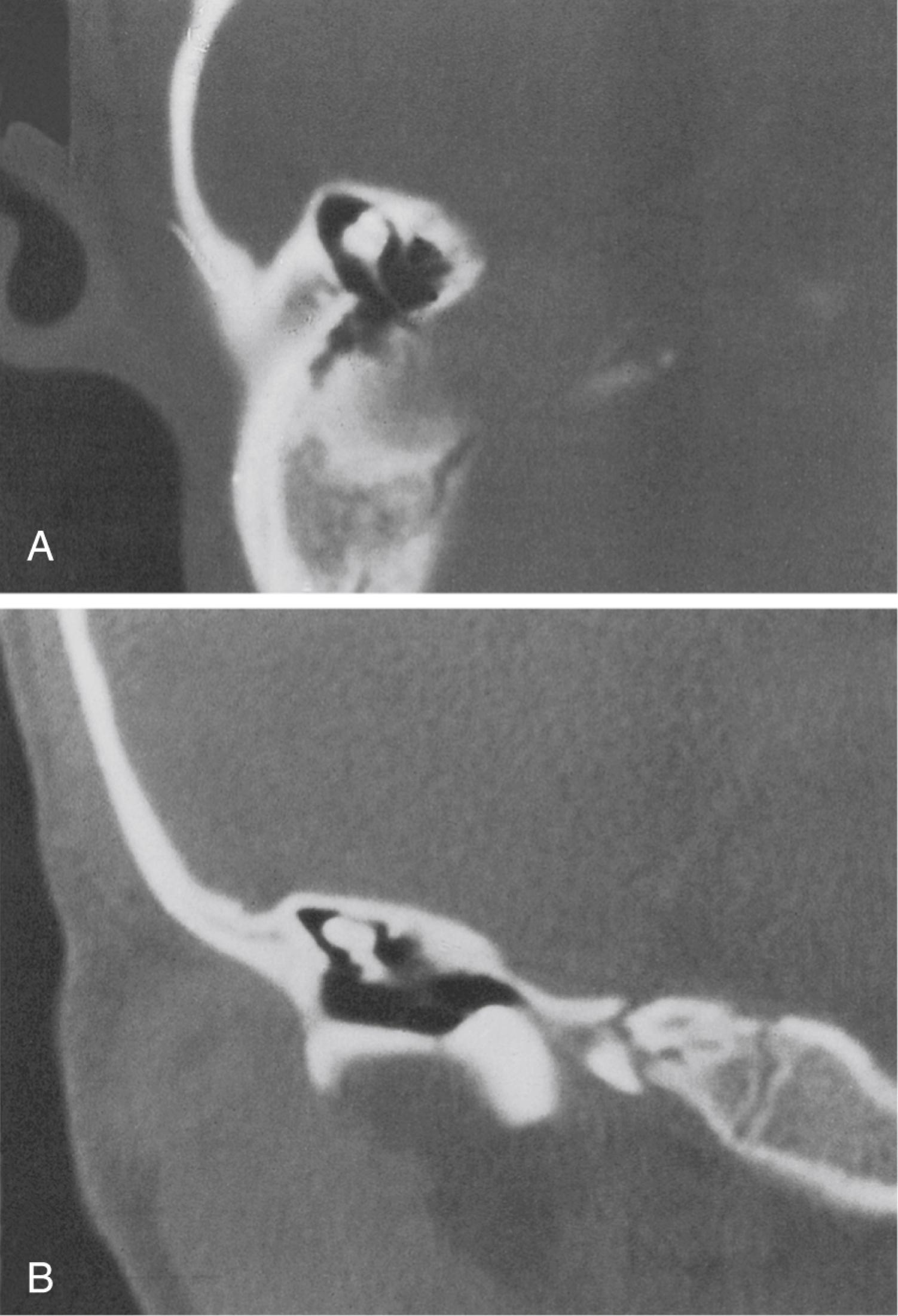
In cochlear aplasia, the cochlea is completely absent, presumably as a result of arrested development of the cochlear bud at the fifth week of gestation (see Fig. 13.1 ). This morphologic pattern is rare. Radiographically, only a vestibule and SCCs (usually deformed) are present ( Fig. 13.6 ). To differentiate this anomaly from labyrinthine ossification, it is necessary to assess the amount of otic capsule bone anterior to the internal auditory canal (IAC). In cochlear aplasia, the otic capsule is absent, whereas in osseous obliteration, it is dense and of normal dimensions. Ears with cochlear aplasia are devoid of auditory function.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here