Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Total laryngectomy remains the standard by which other forms of treatment for advanced primary laryngeal carcinoma are evaluated. It should still be considered as a primary treatment modality for selected patients.
Total laryngectomy is also occasionally indicated for advanced thyroid cancers or tumors of the oropharynx or neck that invade the larynx.
The special subset of patients with laryngeal cancer who require a total laryngectomy instead of organ-preservation therapy presents management issues that are particularly complex.
Higher complication rates can be expected in the setting of preoperative radiotherapy and chemoradiotherapy with longer and more complex salvage procedures. Pharyngocutaneous fistula is much less common in nonirradiated patients, and closure of the pharynx should be done in a meticulous fashion. For selected tumors, even in some salvage laryngectomy cases, a linear stapler can be used for resection and closure.
Other factors that may predispose to complications include positive margins, technical errors, diabetes mellitus, hypothyroidism, and poor nutritional status.
Total laryngectomy is also important for management of chronic aspiration as a result of diseases that render the larynx incompetent.
Rehabilitation of swallowing and voice with tracheoesophageal speech allows the best voice-related quality of life after total laryngectomy for most patients.
The tracheal stoma is the hallmark of total laryngectomy. Effective ways to create and manage an adequate stoma are available.
Total laryngopharyngectomy is used for more advanced laryngeal and pharyngoesophageal carcinomas.
Prognosis with hypopharyngeal carcinoma is poor compared with laryngeal carcinoma, and functional organ-preservation rates are also poor. Although controversial, surgery that incorporates adequate reconstruction for swallowing and voice is the best choice for many patients.
The key to successful management of total pharyngeal defects following laryngopharyngectomy is free-flap reconstruction. Fasciocutaneous flaps have significant advantages over visceral flaps. The anterolateral thigh flap has become the workhorse flap for circumferential defects, but radial forearm flaps and jejunal flaps are good options for selected patients.
In rare cases, regional pedicled flaps such as the pectoralis major myocutaneous flap and supraclavicular flap can be substituted for free tissue transfer to prevent complications in salvage laryngectomy and even laryngopharyngectomy.
Although Patrick Watson of Edinburgh is often credited with performing the first total laryngectomy in 1866, no record exists to prove that the operation was actually done by him. Research into Watson's own article apparently answers this question: Watson stated he performed only a tracheotomy while the patient was alive and then did a postmortem laryngectomy of the syphilitic larynx. On December 31, 1873, Billroth of Vienna carried out the first total laryngectomy for a patient with laryngeal cancer. One month earlier, he had performed a vertical cricothyrotomy and local intralaryngeal excision of this patient's lesion. Gross pathologic recurrence necessitated further radical ablation, and the total laryngectomy was punctuated by considerable bleeding, coughing, and arousal from the anesthetic. The patient died 7 months after surgery. In 1875, Bottini of Turin performed a total laryngectomy on a patient who survived for 10 years. By 1880, the operative or early postoperative mortality rates were approximately 50%.
This high mortality rate led Gluck of Germany to develop a two-stage procedure in which the tracheal separation was performed first, such that a healed tracheocutaneous stoma was present when the laryngectomy and pharyngeal closure were performed 2 weeks later. In the 1890s, with his pupil Sorenson, Gluck developed a successful single-stage operation, similar to contemporary techniques in which the larynx was removed from above downward. Advancing from partial laryngectomies in the 1860s, Solis-Cohen reported at the 1892 Philadelphia County Medical Society Meeting on carrying out a total laryngectomy by use of similar Gluck-Sorenson techniques, although Frederick Lange of New York apparently reported performing the first total laryngectomy in the United States in 1879. Radiation therapy (RT) was a popular treatment for patients with laryngeal cancer during the first half of the twentieth century, although with improvements in surgical and anesthetic technique and recognition of RT's limitations, surgery, including total laryngectomy, maintained a prominent role in the second half of the century. In the past two decades, increased focus has been placed on organ preservation. For intermediate and advanced-stage tumors, concurrent chemotherapy and RT have become part of the standard of care, particularly for those patients who are in some way unsuitable for organ-preservation surgery. However, total laryngectomy as a primary treatment modality is still relevant for many patients. The attention on chemoradiation therapy (CRT) has resulted in an increase in salvage total laryngectomy and laryngopharyngectomy procedures, complicated by a greater potential for complications as a result of the tissue damage following CRT.
With the spectrum of organ-preservation surgery now available, the need for total laryngectomy as the only surgical option for those with laryngeal cancer has decreased. Organ-preservation surgery includes specific procedures for supraglottic and glottic cancer. Two major organ-preservation surgical strategies are the transoral (endoscopic) and open approaches. These are discussed in detail in other chapters. Transoral procedures range from the very limited to extensive laser or robotic procedures that require greater surgical experience and specialized instrumentation. Open procedures include the more conventional vertical partial laryngectomy procedures and the horizontal supraglottic partial laryngectomy procedures to supracricoid partial laryngectomy. Organ-preservation surgery has been well documented in the literature and is not new. Organ-preservation surgery can safely be used after RT, but the complication rate is higher.
Another operation that avoids total laryngectomy is the near-total laryngectomy. This procedure is not strictly an organ-preservation operation, because it does not maintain an airway without a tracheostome. Essentially, it can be viewed as a total laryngectomy with an epithelialized voice fistula. Nonsurgical treatment for patients with laryngeal malignancy also is established as primary treatment in some centers. Management includes definitive radiation alone with surgery for salvage for patients with primary lesions up to T3 or neoadjuvant chemotherapy and RT, with total laryngectomy reserved for those with unresponsive tumors. The frequently cited Veterans Affairs study randomly assigned patients with advanced laryngeal cancer to chemotherapy and RT or total laryngectomy. Although present, the increased survival in the surgical arm was not significant. Criticisms of the study prompted a head and neck intergroup trial that randomly assigned patients to three groups and compared radiation alone versus concurrent versus sequential chemotherapy with RT. This trial demonstrated that concurrent chemotherapy with RT (CRT) is superior to sequential chemotherapy followed by RT or radiation alone in terms of local control and organ preservation. However, there was no surgical arm to this study, and it thereby fell short of establishing a new standard of care. Furthermore, using primary concurrent CRT, the 5-year results for both disease-free survival (39%) and laryngectomy-free survival (46%) show that this method leaves the majority of patients either dead or absent their larynx at 5 years. Therefore this leaves much room for improvement in treatment of laryngeal cancer. Other studies have shown that if nonsurgical organ preservation is to be used, concurrent chemotherapy with hyperfractionated RT is more effective than RT alone and that hyperfractionated RT is more effective than standard radiation alone. Subsequent trials investigated the impact of induction chemotherapy to assess tumor response. A complete or near-complete response to chemotherapy then selects the patients for concurrent chemotherapy and RT. No biologic marker yet identified can reliably predict which patients are better treated surgically. This is also the topic of investigations in concurrent studies. Because the survival of the two treatment strategies is equivalent, quality-of-life issues are of paramount importance. A study demonstrated that in the intergroup trial, patients who had total laryngectomy after RT had a high complication rate that included a risk of pharyngocutaneous fistula of up to 30%, which was the highest in the concurrent chemotherapy group. In addition, studies that have evaluated the quality of life after nonsurgical management of advanced laryngeal cancer suggest that organ preservation is associated with improved quality of life. Advances in nonsurgical treatment for laryngeal cancer are beyond the scope of this chapter but the previously mentioned studies remain the classically cited literature. Free tissue transfer has clearly improved the outcomes for patients undergoing salvage total laryngectomy. Systematic review of complications of salvage total laryngectomy from articles published between 2000 and 2015 shows that about two-thirds of patients will experience complications and nearly 29% of patients developed pharyngocutaneous fistula. Although the details of such studies are beyond the scope of this chapter, the results indicate that more extensive analysis of quality of life is important. These studies are difficult to accomplish because many patients are not available after the study and the quality of life of the survivors might be significantly different than that of the patients who had died, particularly if they died of local complications related to uncontrolled primary site disease. Consensus of numerous studies in the organ preservation literature shows that patients who require tracheostomy, who have very advanced T4 lesions, or who have preoperative dysphagia are unlikely to have successful functional organ preservation and should be considered for primary total laryngectomy. This is especially true for hypopharyngeal cancers where the organ preservation rate is even lower but is true of laryngeal cancer as well.
Total laryngectomy remains a viable option as the primary surgery for advanced cancer or as salvage surgery after RT and, finally, for a group of less common conditions. Overlap among these indications occurs. For example, a patient with radionecrosis of the larynx may be found to have residual tumor on permanent sections and, as such, the surgery was a salvage procedure in hindsight. Similarly, a tumor that fails RT may also be causing chronic aspiration and may be too large to allow for any sort of organ-preservation surgery. This sort of patient has at least three of the following indications for undergoing the procedure, and maybe more:
Advanced tumors with cartilage destruction and anterior extralaryngeal spread, which often manifests initially with laryngeal dysfunction that includes vocal cord paralysis; airway obstruction; or severe aspiration. Such patients are not good candidates for organ preservation, because the organ already has been damaged and will not likely function even if it can be preserved anatomically.
Posterior commissure or bilateral arytenoid/cricoarytenoid joint tumor involvement, as is sometimes seen in advanced supraglottic tumors.
Circumferential submucosal disease with or without bilateral vocal cord paralysis.
Subglottic extension with extensive invasion of the cricoid cartilage.
RT or chemoradiation failures, including those who have also had partial laryngectomy failure.
Completion laryngectomy for failed conservation or extensive endoscopic surgery.
Hypopharyngeal tumors that originate at or spread to the postcricoid mucosa and advanced piriform sinus cancers.
Massive neck metastases and thyroid tumors (usually recurrent) that invade both sides of the larynx from outside the laryngeal skeleton.
Advanced tumors of certain histologic types that are incurable by endoscopic resection, chemotherapy, or RT (e.g., adenocarcinoma, spindle cell carcinoma, soft tissue sarcomas, minor salivary gland tumors, and large cell neuroendocrine tumors) and chondrosarcomas of the thyroid cartilage.
Extensive pharyngeal or tongue-base resections in patients who are at high risk for aspiration problems.
Radiation necrosis of the larynx, despite tumor control, that is unresponsive to adequate antibiotic and hyperbaric oxygen management (this condition can be painful and also predisposes patients to aspiration, and tumor is often found when total laryngectomy is performed).
Severe irreversible aspiration, with the laryngectomy used for complete separation of the air and food passages (this indication should be rare, considering the variety of other separation or closure procedures available).
The following patient requirements should be met before a total laryngectomy is performed:
The patient should be a candidate for general anesthesia; consider severe comorbid conditions as a relative contraindication.
Informed consent includes realistic understanding of total laryngectomy state and lifestyle after surgery, including the risk of drowning, the need to avoid swimming and certain risky activities, and the lack of sense of smell in the event of fire, smoke, or toxic fume exposure.
Sufficient performance status, especially dexterity, to allow basic self-care of the stoma.
The workup required for a total laryngectomy includes the anesthetic-related assessment of general health (not elaborated here) and specific tests relevant to the larynx. Assuming the patient has a laryngeal carcinoma, the following are required:
History and physical examination should be performed, and details of any previous radiation are especially important.
A comprehensive head and neck examination should be done, but especially the neck, for detection of cervical metastasis.
Biopsy proof of malignancy and careful endoscopic assessment of tumor location; use of both microscopic and telescopic endoscopy can help determine the need for total laryngectomy and can also help determine which patients are likely to have extensive subglottic extension or submucosal extension in the hypopharynx.
Synchronous primary tumor screening should include bronchoscopy, esophagoscopy, and/or barium swallow, chest radiography, and chest computed tomography (CT) in selected cases.
Metastatic screening should be done when indicated.
Neck CT should be done for assessment of cartilage or preepiglottic space invasion in those with advanced or radiation-recurrent lesions and for assessment of radiologically detectable neck metastasis. Positron emission tomography (PET) and magnetic resonance (MRI) scans may also be useful.
In the laboratory evaluation, diabetes and hypothyroidism should be evaluated and managed appropriately, because they increase the risk of complications. A nutritional screening is also indicated, and evaluation for the potential for postoperative alcohol withdrawal is also important. Careful attention should be paid to evidence of anemia and malnutrition and these should be corrected prior to surgery.
The role of metastatic workup is detailed in other chapters, as are indications for different imaging studies.
As mentioned earlier, nutrition and hemoglobin as well as hypothyroidism should have been addressed. Airway management must be discussed. A perioperative briefing, including all members of the operative team, can be very helpful. In general, prophylactic antibiotics should be used. The antibiotic most commonly used in practice is amoxicillin and sulbactam and the dosing is usually 1500 mg every 8 hours beginning about 1 hour preoperatively and continued for at least 24 hours. A case can be made for extending coverage for 48 to 72 hours in complicated cases (salvage or flap reconstruction cases or patients at increased risk of infection). This antibiotic will cover most of the organisms but there are some infections that are caused by resistant organisms (most commonly methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa ), and in such cases vancomycin and/or an antipseudomonal antibiotic (such as ticarcillin) should be utilized.
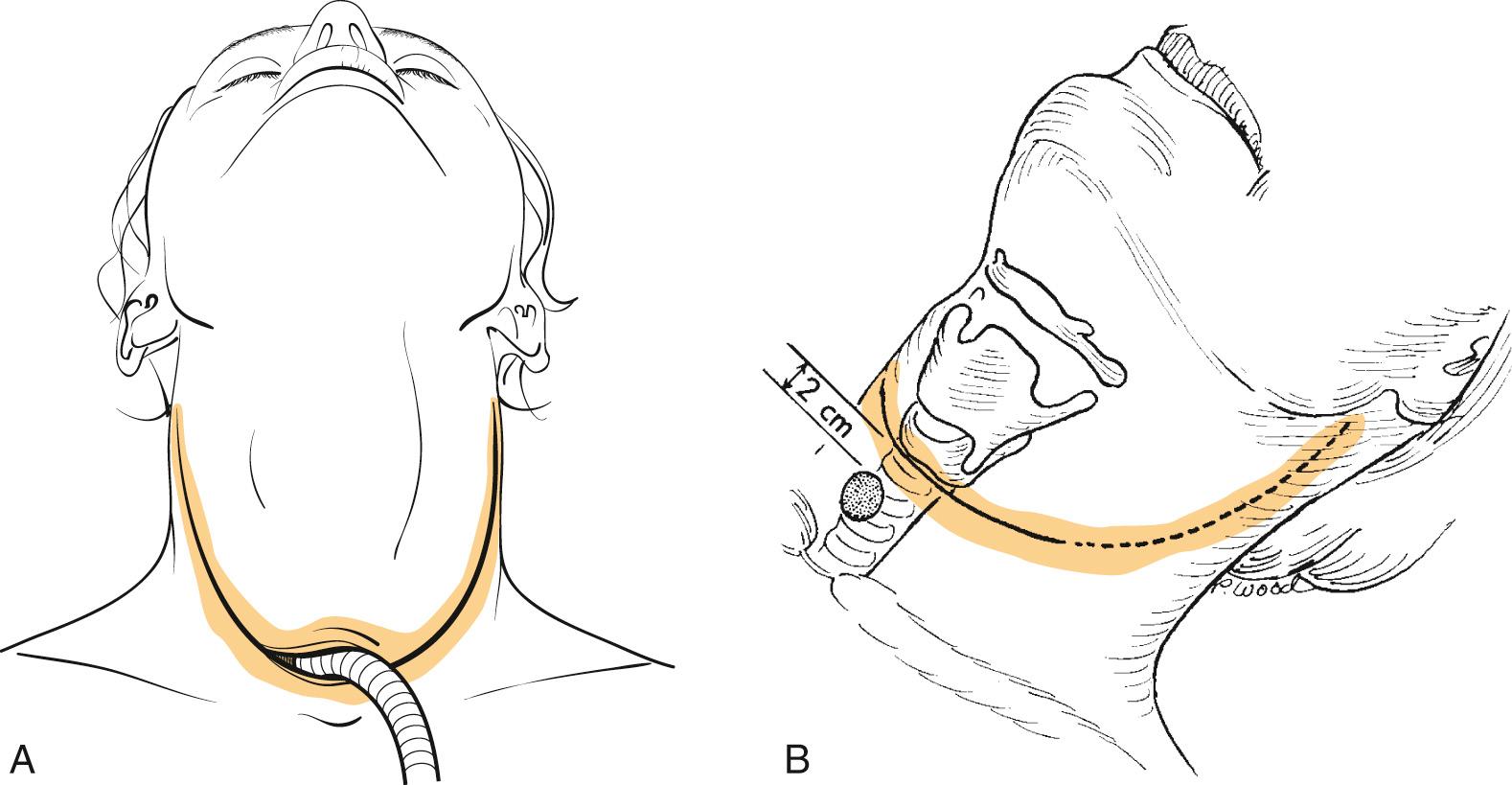
Proper patient positioning provides access to the anterior part of the neck for the surgeon and the assistant. Positioning is best achieved by placing the patient on a table fitted with a head holder that allows the head to be cantilevered out but well supported. This also assists bilateral neck dissection, which is often performed in continuity, and allows surgeons to position themselves all the way around the head. The table is turned 180 degrees from the anesthesiology team to further assist access to the patient. Before the operation day, airway management is planned with the anesthesiologist so that an agreement is reached regarding timing of tracheotomy and intubation. In the unobstructed larynx, the anesthesiologist may pass an orotracheal tube with anesthetic induction; this tube may be removed at subsequent tracheotomy, or it may be left in situ until tracheal transection is performed at the end of the laryngectomy. With an obstructed airway or when intubation may displace malignant tissue into the lower airway, a preliminary tracheotomy with the patient under local anesthesia is performed. The tracheotomy skin incision is made at the intended site of the final stoma, which can be placed in the line of the incision (long flap) or 2 cm to 3 cm inferior to the incision ( Fig. 109.1A and B ). The advantage of the former is that creation of the stoma is more reliable and avoids a bipedicled bridge of skin between the flap incision and the tracheostomy incision, which can result in stenosis of the stoma. The advantage of the latter ( Fig. 109.2 ) is that in the event of pharyngocutaneous fistula, which requires diversion, the stoma is less likely to be involved in the resulting wound. The latter consideration is perhaps more important in previously irradiated patients, because the risk of fistula in primary total laryngectomy is low. This configuration also avoids the technical nuances of bilateral, three-point closures at the stoma necessitated by exteriorizing the lower-cut tracheal end through the laryngectomy skin incision. In the long-flap approach, the three-point closure will later be performed after the inferior aspect of the stoma is completed. This is somewhat more difficult to accomplish with the stoma created 2 to 3 cm into the inferior flap, because the trachea is not anchored to the lateral aspect of the dissection. Ultimately, the comfort level of the surgeon determines the choice of incision.

Every attempt should be made to enter the trachea with a horizontal cut at the ultimate level intended for tracheal transection, but in the event that a tracheotomy is already in place, the tracheal transection should be 2 cm inferior to the existing tracheotomy site if possible. A precurved or flexible reinforced cuffed tube is then passed into the trachea, and adequate ventilation is confirmed. The cuff of the tube is prepped into the field so that the tube can be removed intermittently for suture placement during creation of the stoma.
For access to the larynx, a curved, horizontal neck skin incision is preferred because of its minimal intersection with the pharyngeal closure and its potential for extension laterally into a neck dissection incision. Once the incision is deepened through, but not beyond, the platysma, flaps are elevated superiorly and inferiorly in the subplatysmal plane, until exposure extends above to the upper border of the hyoid bone and below to the cervical trachea. The anterior jugular veins and the prelaryngeal delphian node are left undisturbed on the specimen, as are the strap muscles. The sternocleidomastoid muscle then is identified along its anterior border on each side, and the investing layer of cervical fascia is incised longitudinally from the hyoid above to the clavicle below. The omohyoid is then divided, which allows entry to the loose areolar compartment bounded laterally by the sternomastoid muscle and carotid sheath and medially by the pharynx and larynx contained in the visceral compartment of the neck. Appropriate neck dissections are performed. The extent of neck dissection is beyond the scope of this chapter, but a few points merit mention. For supraglottic carcinoma, the minimal neck dissection to be performed is selective neck dissection, stations II and III bilaterally. It is extended to Level IV and possibly IB and V if lymphadenopathy indicates the need. For advanced glottic carcinoma with supraglottic involvement, the same procedure is recommended. Unilateral (ipsilateral) neck dissection can be considered for T3 glottic carcinoma. For patients who have previously been irradiated, evidence still supports selective neck dissection. In general, both neck dissections can be pedicled at the thyrohyoid membrane area, and the resection can easily be done en bloc. The role of dissecting Level IIB in laryngeal cancer has been investigated as well and for the N0 neck, it appears to be unnecessary.
The strap muscles are divided inferiorly from their sternal origins and are elevated to expose the thyroid gland ( Fig. 109.3A ). Controversy exists with regard to thyroidectomy as part of a total laryngectomy. Studies note that involvement of the thyroid gland is rare. However, when nodal disease is present in the jugular chain from glottic or subglottic cancer, the thyroid is at high risk because of the paratracheal and parapharyngeal lymphatics associated with the thyroid. The classic literature shows that in patients who have invasion of the thyroid or cricoid cartilage in close proximity to the thyroid gland, the gland may become directly involved by the tumor. But more recent studies show that routine thyroidectomy is not necessary. The risk to the thyroid is the highest with transglottic cancers that extend more than 1 cm below the glottis. A recent study suggests that anterior commissure involvement (in addition to thyroid cartilage invasion and transglottic spread) may be a risk factor for thyroid gland invasion and that even when thyroidectomy is used selectively, taking these risk factors into account, actual invasion is only seen in about 20% of patients. MRI has been shown to have excellent predictive value for thyroid gland invasion and should be recommended in patients who have the risk factors noted earlier. Most recently, CT has been shown to be reliable as well. In some cases, both lobes of the thyroid should be removed because of these risk factors. When the lobe of the thyroid is to be removed, the superior and inferior thyroid vascular pedicles are ligated and divided, as is the middle thyroid vein. Any lobes to be preserved are then dissected off the laryngotracheal skeleton from medial to lateral, thereby preserving blood supply to the remaining thyroid and parathyroid parenchyma by way of inferior thyroid vessels; the superior thyroid artery can be preserved also, if this is oncologically sound, but it is not necessary. An effort should be made to preserve the vascularity to the parathyroid glands, but if a parathyroid gland is noted to be poorly vascularized after the procedure, this can be reimplanted into the neck musculature, as is done for parathyroidectomy in thyroid cancer. Next, after dividing and ligating the upper and lower extent of the anterior jugular veins, the superior aspect of the hyoid bone is skeletonized by detaching the mylohyoid, geniohyoid, digastric sling, and hyoglossus in sequence from medial to lateral (see Fig. 109.3B ). So-called cold knife dissection should be used lateral to the lesser cornu, and excess electrical stimulation or direct damage to the hypoglossal nerve should be carefully avoided. Caution is advised for supraglottic cancers that involve the aryepiglottic fold, piriform sinus, or vallecula, because too much skeletonization of the hyoid bone and thyrohyoid membrane area may put the surgeon in close proximity to the deep extent of the tumor, which might result in a close or positive margin histologically. This is not a concern with completely endolaryngeal cancers; the sternohyoid and thyrohyoid muscle attachments on the lower border of the hyoid bone remain undisturbed. Further laryngeal cartilage skeletonization is performed at this point if the tumor does not extend outside the piriform fossa. The posterior border of the thyroid cartilage lamina is rotated anteriorly by upward traction, which allows sharp release of the constrictor muscles from the inferior to the superior cornu (see Fig. 109.3C ). Above the superior cornu, the laryngeal branch of the superior thyroid artery should be identified, ligated, and divided before it penetrates the thyrohyoid membrane.
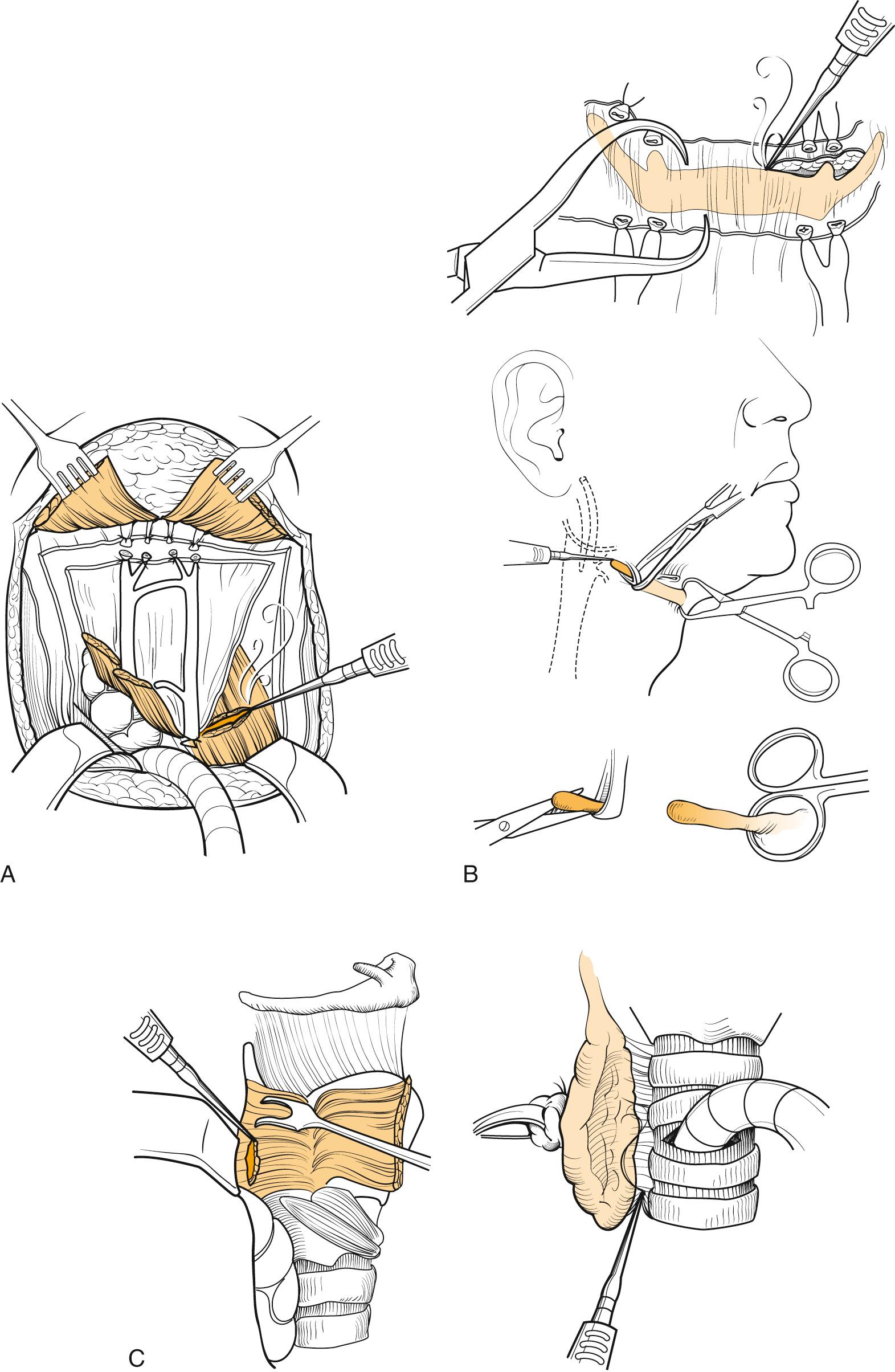
The pharyngotomy incisions and definitive laryngeal removal are now performed. To avoid contact with the neoplasm or cutting through its submucosal extensions, the pharynx is entered contralateral to the tumor. If superior extension to the tongue base is present, lateral pharyngotomy behind the thyroid cartilage is performed, and by use of a headlamp, the extent of the tumor is inspected. A safe 2-cm margin of normal-looking mucosa is preserved with further cuts from below, progressing superiorly behind the thyrohyoid membrane, around the hyoid bone, and then transversely across the vallecula or tongue base. By contrast, if the disease is confined below the level of the hyoid, entry by way of the vallecula is feasible. This is preceded by a mobilization of the pyriform sinus ( Fig. 109.4A ) and transection of the trachea (see Fig. 109.4B ). Once these steps are completed the vallecula can be entered (see Figs. 109.4 and 109.5 ) in the horizontal plane of the upper hyoid border. Strict maintenance of this plane, avoiding excessive inferior traction on the hyoid itself, precludes violation of the preepiglottic space. Once the mucosa is breached, the tip of the epiglottis is identified; if free of tumor, it is grasped with an Allis forceps and gently pulled anteriorly out of the pharyngotomy. A view of the endolarynx and pharynx is now possible to assess tumor extent and to plan appropriate mucosal cuts.
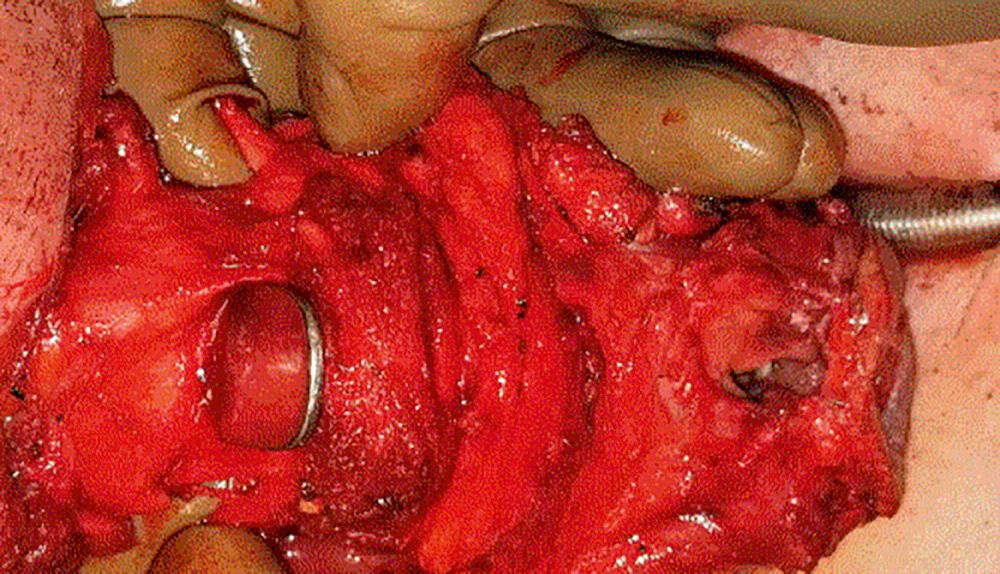
With a Mayo scissors, bilateral, inferiorly directed cuts are made to release the lateral pharynx from the larynx; the inside scissors blade is on mucosa, and the outside blade is on constrictor musculature. As these incisions are made from the vallecula to the piriform sinus, the larynx is further angled anteriorly out of the wound, until it is released to the apices of the piriform sinuses. The postcricoid mucosa is exposed and incised sharply in the transverse direction to connect the inferior extent of both lateral incisions across the lower half of the cricoid lamina. Next, a plane of blunt dissection is opened that is initially behind the posterior cricoarytenoid muscle; from there, it proceeds down between the trachea and longitudinal esophageal muscle, until the desired level of tracheal transection is reached. Optimum exposure of the trachea at this stage is achieved by further lateralization of the preserved thyroid lobe followed by knife transection of the trachea. This cut is beveled upward from anterior to posterior taking great care not to encroach on any subglottic tumor extension. If the latter is present, a 1.5- to 2-cm margin of healthy-appearing trachea should be resected in continuity with the larynx to avoid stomal recurrence. If a preliminary tracheotomy was not performed, the oral endotracheal tube is next withdrawn from the tracheal stump and a new, cuffed, flexible tube is inserted for connection to new anesthesia tubing. As an alternative, the order of steps can be altered slightly as indicated by the pathology. In some cases the initial entry into the pharynx must be from inferior or from the lateral aspect if there is concern about involvement of the vallecula or base of tongue. As long as extensive subglottic spread is not evident, preliminary tracheotomy and subsequent tracheal transection greatly assists the resection; this is performed after dissection of the thyroid gland and skeletonization of the thyroid cartilage. If not previously done, the trachea is entered 2 cm below the inferior extent of tumor, and careful inspection is done upon entry. The endotracheal tube is withdrawn, and the trachea is further incised laterally. A reinforced tube is placed, and a sterile connector is passed through the drapes to connect to the circuit. The trachea is then transected by making a notched incision in the posterior wall; this is taken down to the esophageal musculature. Once the ligamentous attachments and the recurrent laryngeal nerve are divided, blunt dissection can be performed up to the level of the posterior cricoarytenoid musculature. Then, when the surgeon enters the larynx and completes the mucosal cuts from superiorly along the aryepiglottic folds, the specimen is pedicled on the postcricoid mucosa only; this assists the final transection and can reduce the blood loss. The surgeon places a pack in the pharynx and neck while inspecting the specimen for orientation and margin assessment. After the specimen is passed from the table, it is carefully inspected for adequacy of resection, and a pathologist's frozen-section study of the patient's entire cut margins to include the trachea, tongue, and pharyngeal mucosa is requested. The tracheal margin is critical, because in some patients, submucosal occult microscopic disease spreads down the trachea despite relatively normal-looking mucosa; excising all disease helps prevent stomal recurrence. The wound is thoroughly irrigated, all clots are removed, and hemostasis is achieved.
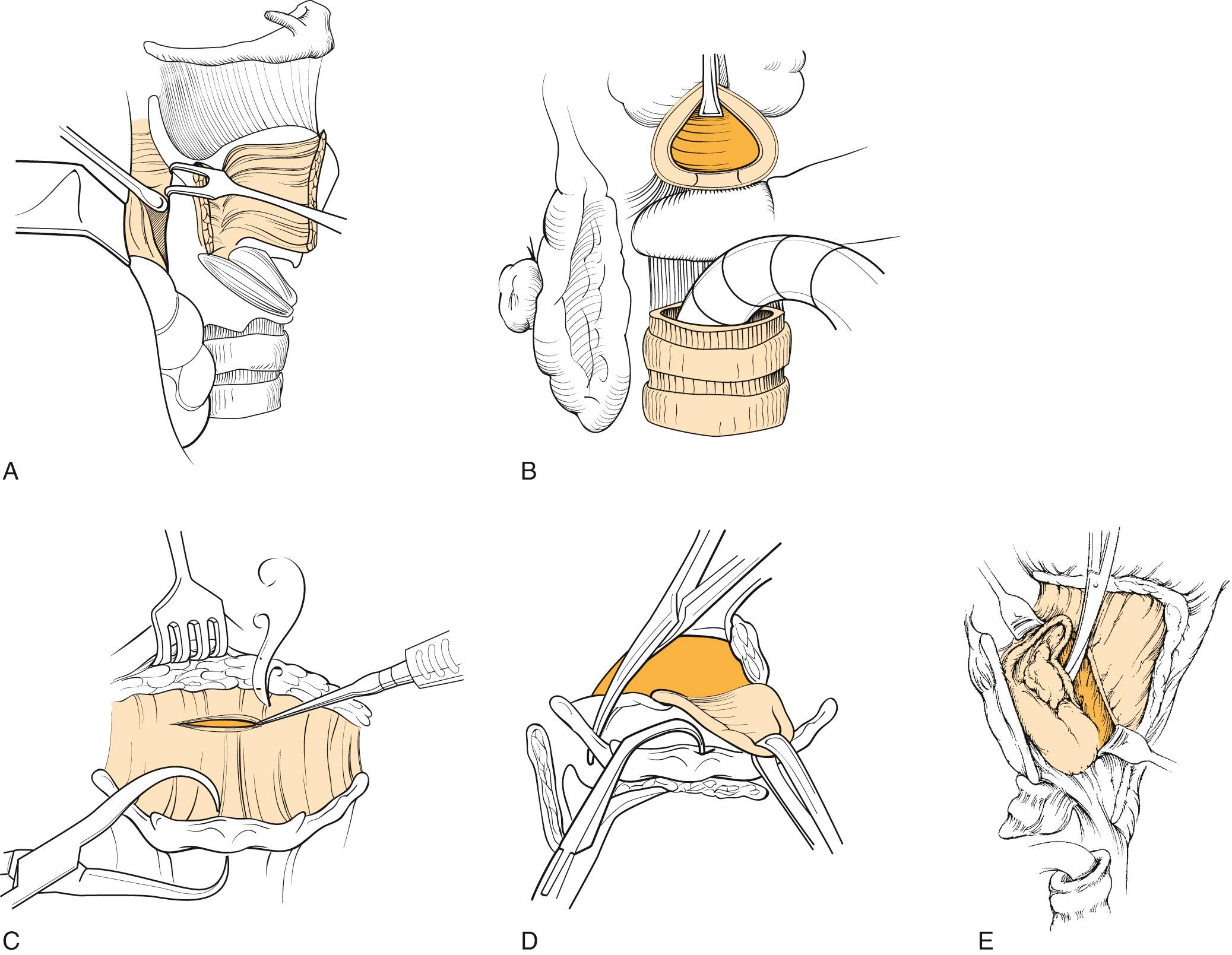
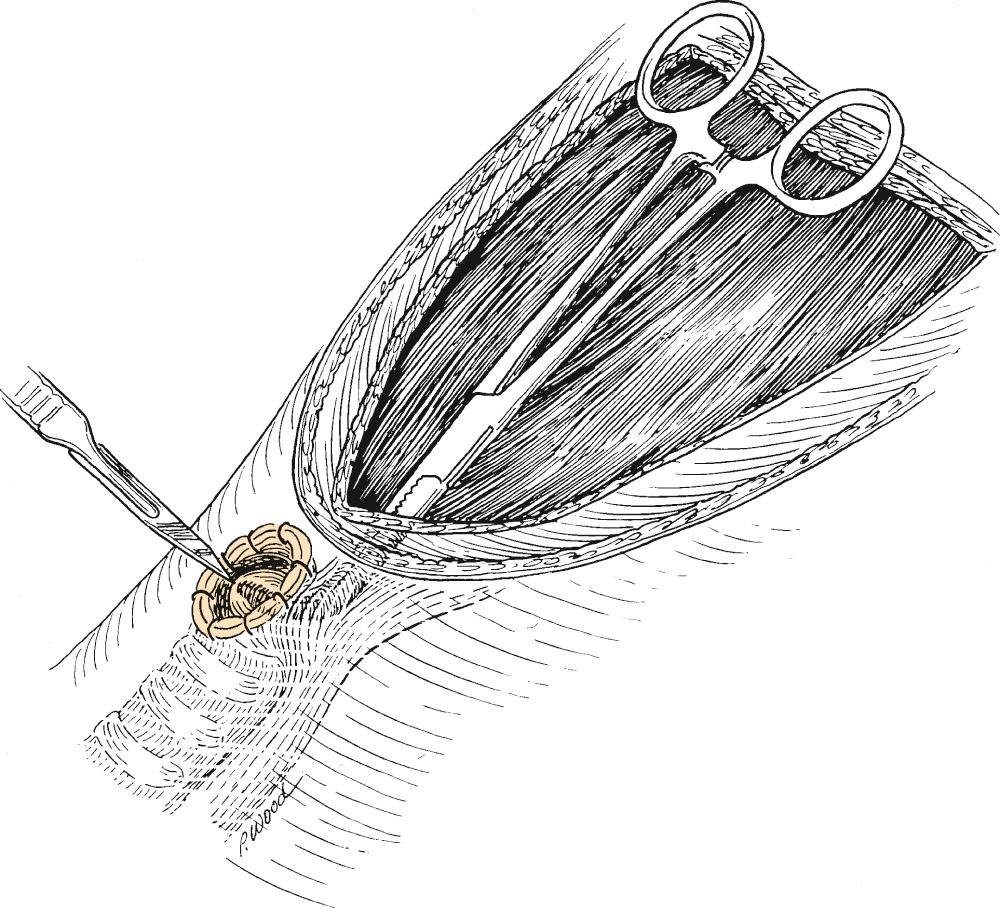
If a primary tracheoesophageal puncture (TEP) is to be performed, creating the tracheostome before pharyngeal repair may be considered to enable definitive positioning of the trachea relative to the esophagus and skin before a puncture site is selected. A pair of right-angled forceps is then passed into the esophagus, with the tip elevating the posterior tracheal wall at the intended puncture site ( Fig. 109.6 ). A tracheoesophageal stab incision is made, and the forceps tips are exposed; with these, a catheter is grasped, pulled into the pharynx, and then fed down the esophagus. This is secured to the anterior chest wall skin, and the prosthesis is inserted once the tract is fully healed. The prosthesis may also be inserted primarily in some patients.
The previously described resection technique clearly needs to be modified according to the extent of tumor spread. A common variation is the so-called wide-field laryngectomy, in which overlying neck skin is resected in continuity with the larynx and thyroid gland. This method is sometimes prudent for tumors that have invaded soft tissue outside the laryngeal skeleton, but it usually requires pedicles of free flap to close the neck and create a stoma. Another modification of the technique involves using a linear 75-mm stapler to do the resection. In this situation, the pharyngoplasty is performed simultaneously, as the stapler closes the pharynx while making the final tumor cuts. The appropriate indications and technical modifications are described very well in an article by Gonçalves and colleagues. Most importantly, this method requires extensive skeletonization of the larynx and is only recommended in selected cases of endolaryngeal tumors, with glottic involvement with extension to the thyroid cartilage through the anterior commissure or with extension to the subglottis. Involvement of piriform sinuses and aryepiglottic and glossoepiglottic folds is a contraindication to the stapler technique. A systematic review shows that appropriate use of the stapler technique offers the advantage of lower pharyngocutaneous fistula rates, earlier onset of oral feeding, and reduced length of hospital stay.
Another innovation that merits mention is the transoral robotic total laryngectomy, which allows the procedure to be done with a minimal incision, essentially just that needed to create the stoma. It has been demonstrated to be feasible and may be appropriate in selected patients.
Pharyngeal reconstruction is currently performed by direct closure or flap augmentation. Configurations for a direct repair are T -shaped or linear (horizontal or longitudinal; Fig. 109.7 ). Selection of closure type is based on an assessment of the shape and size of the pharyngeal defect, the elasticity of remaining tissue, and simulated wound approximation before suturing. The least-tensioned apposition of wound edges is the best; it is usually T -shaped and results in minimal or no horizontal pharyngeal shelf formation. However, a straight closure is less prone to technical failure in patients with abundant pharyngeal mucosa for closure.
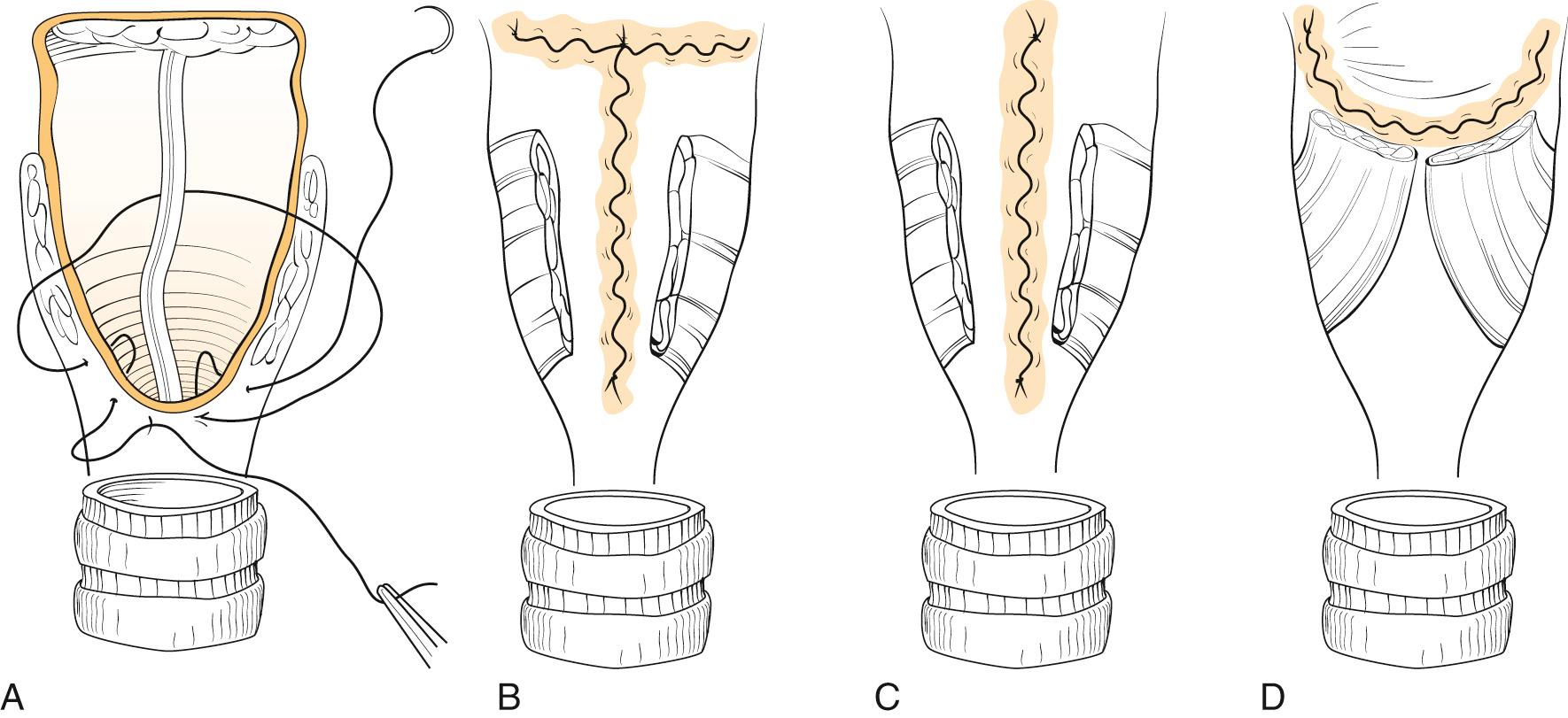
The pharyngeal wall is closed in a single layer. A running or interrupted closure, according to the surgeon's preference, is used with particular attention to inversion of the mucosal edges into the pharynx. This inversion is achieved with an absorbable stitch that runs horizontally through the submucosa, without penetration of the mucosal surface. A longer-retained material such as polyglycolic acid (3-0) is used and is adequate for irradiated tissue, and large series of stapled closures have also been reported. Although some advocate closure of the pharyngeal muscle, this is not necessary. Reinforcement of the suture line with muscle sutures may be performed in selected cases, where the mucosa has been compromised by radiation, but it is not a substitute for good mucosal closure. One study has shown that a mucosal closure alone is sufficient for sound healing, and closure of muscle can lead to difficulty with tracheoesophageal speech and dysphagia. Some surgeons recommend a closure of the muscle over the suture line with a constrictor myotomy performed laterally and a myotomy done inferiorly along the lateral aspect of the esophagus, sometimes called a cricopharyngeal myotomy —somewhat of a misnomer, given that the cricoid has been removed. This technique reinforces the closure with a second layer but avoids the circumferential effect of the muscle closure.
If pharyngeal wall is insufficient to close over a 36-Fr dilator, a flap repair should be considered to increase the circumferential dimension of the neopharynx. Hui and colleagues addressed the question of the width of the pharyngeal wall remnant relative to postoperative dysphagia and concluded that a remnant as small as 1.5-cm wide was sufficient to avoid dysphagia, although the study included only one patient with a remnant as small as 1.5 cm. Reconstructive options include a myocutaneous flap, a muscle flap, or a microvascular free flap. In extremely difficult cases, a controlled salivary fistula can be created to avoid catastrophic wound problems. In such patients, the flap will allow a vascularized bed that will ultimately allow removal of the conduit that is placed.
Following closure of the pharynx, saline or peroxide can be placed in the oral cavity to examine the suture line for leakage.
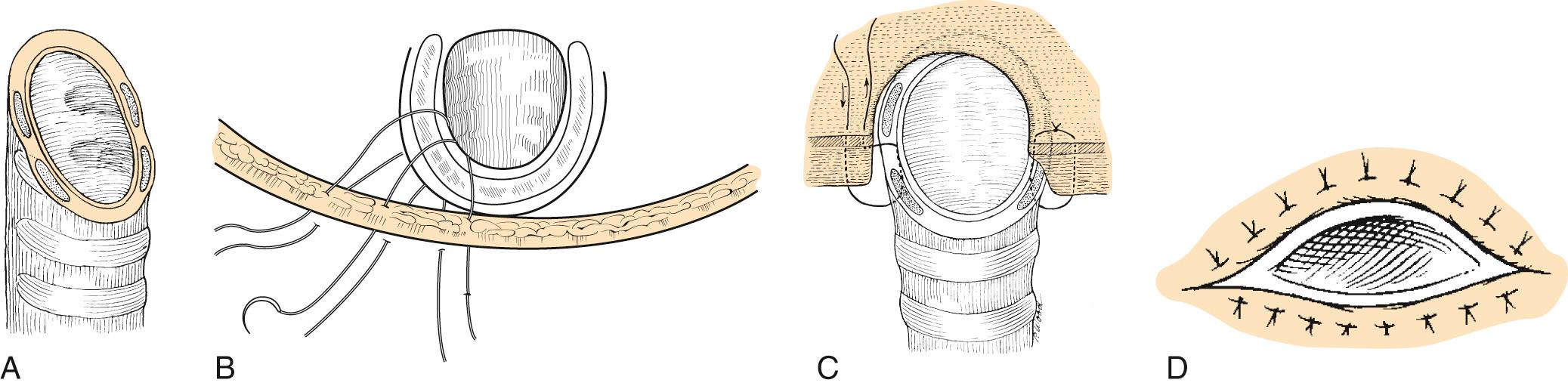
For the long-flap approach, the stoma is inserted into the center of the lower flap with a central suture of 2-0 Vicryl, excising an ellipse of skin if needed. In the short-flap approach, the permanent end-tracheal stoma is created by excising a shield-shaped skin island from the lower neck flap in the midline, just above the sternal notch. Any excess adipose tissue or bulky sternocleidomastoid muscle or tendon is excised deep to the skin flap to minimize tracheostenosis. The central suture is then secured to the lower aspect of the shield-shaped defect. The circumferential suture line should provide support for the trachea and should allow accurate skin-mucosa apposition without cartilage exposure. These sutures should be placed beginning in the center, with each subsequent suture placed lateral to the prior one. For each suture, the surgeon proceeds farther along the skin edge than the mucosal edge, which serves to pull the trachea outward; in addition, the trachea is not sewn in a circular fashion. By bringing the lateral trachea down to the inferior flap, the inferior aspect of the stoma is elongated to produce a more horizontally based trapezoid (shield) shape that avoids the circumferential stenosis or slitlike vertical stomas, which may result in a need for revision. This is best achieved by a modified (“half-buried”) vertical mattress suture that traverses skin peripherally, cartilaginous tracheal wall extramucosally, and skin centrally.
So, to summarize, we have Fig. 109.8 , which demonstrates the three ways to maximize stoma size: (1) bevel the trachea (which can usually be done during the resection); (2) elongate the base; and (3) cover the cartilage. A 2-0 Vicryl is used for the central suture, and a 3-0 Vicryl is used for the remaining inferior sutures. A trifurcating suture can be used (either 3-0 or 4-0 Vicryl), in which the superior flap comes into contact with the lateral aspect of the stoma bilaterally (in the long-flap approach). Absorbable sutures are preferable, because suture removal is undesirable in the stoma region.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here