Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The gallbladder is a distensible pear-shaped reservoir, the function of which is to store bile and deliver it to the duodenum for digestion (see Chapter 62 ). It is located along the undersurface of the liver and composed of 3 regions: the fundus, body, and neck. Gallbladder filling and emptying occur in both the interdigestive and postprandial periods. Emptying of bile into the duodenum in response to the presence of food in the upper GI tract is regulated primarily by CCK.
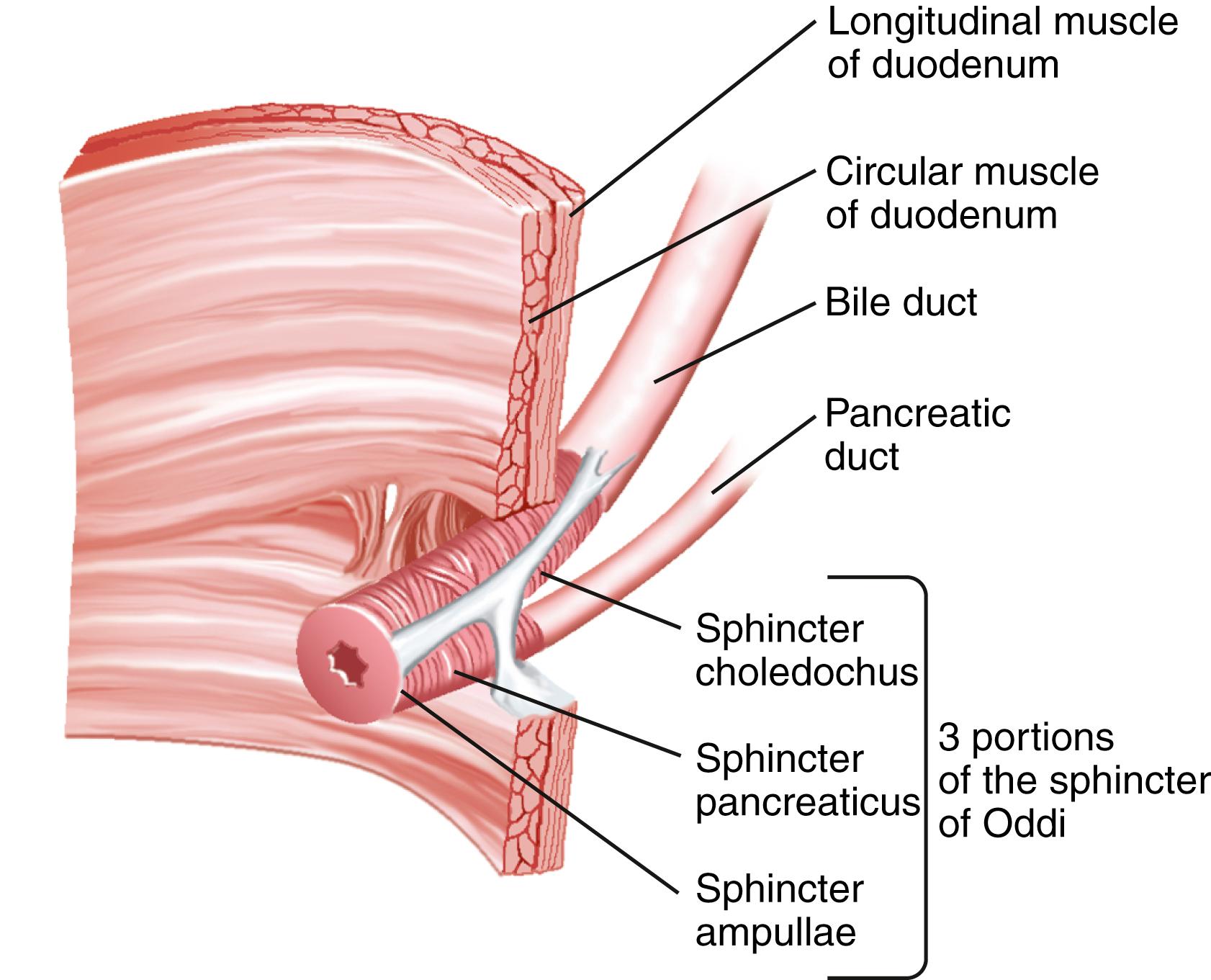
The sphincter of Oddi (SO) is composed of layers of smooth muscle that are embedded in, but functionally separate from, the muscle of the duodenal wall and that serve as a 4- to 10-mm high-pressure zone (see also Chapter 62 ). The SO comprises 3 parts: a small segment (sphincter ampullae) that covers the common channel formed by the union of the bile and pancreatic ducts (when a common channel is present); a second small portion (sphincter pancreaticus) that surrounds the beginning of the main pancreatic duct; and the largest portion (sphincter choledochus) that covers the distal bile duct ( Fig. 63.1 ). In addition, the fasciculi longitudinales are muscle bundles that span intervals between the bile and pancreatic ducts. The SO functions primarily as a resistor, with tonic contraction that limits bile flow during the interdigestive period. It also serves as a pump, with phasic contractions that facilitate the flow of bile into the duodenum, perhaps serving a housekeeping function for the distal bile duct. The SO participates in the migrating motor complex, with motilin-induced increases in the frequency and amplitude of sphincter contractions shortly before and during bursts of intense duodenal contractions.
The complex neurohormonal control of biliary motility involves sympathetic, parasympathetic, spinal, and enteric nerves. Almost every neurotransmitter in the enteric nervous system has been identified in the biliary tract. Reflex pathways between the gallbladder and SO coordinate the flow of bile.
Although acalculous gallbladder pain has been attributed to dysmotility, the correlation is far from perfect. Gallbladder stasis clearly predisposes to sludge and stone formation, but whether gallbladder dysfunction (or dyskinesia)—delayed emptying of the gallbladder in the absence of stones or sludge—causes biliary symptoms remains unclear. Based on a single small randomized controlled trial (RCT) and several observational studies, delayed gallbladder emptying has been reported to predict pain relief after cholecystectomy ; however, this finding remains controversial. Delayed gallbladder emptying occurs in normal asymptomatic persons and is even more common in patients with functional GI disorders. It also appears to be associated with many unrelated diseases such as obesity and diabetes mellitus. Dysmotility may be an important contributor to gallbladder inflammation, which is present in many resected acalculous specimens, but confirmation of a gallbladder source of symptoms based on histologic diagnosis of chronic cholecystitis has been disputed.
A meta-analysis of 9 studies and a systematic review of 23 studies concluded that existing evidence does not support gallbladder ejection fraction as a predictor of symptom relief after cholecystectomy (see Chapter 67 ). Other smaller meta-analyses, however, have demonstrated a statistically significant benefit associated with cholecystectomy in symptomatic patients with gallbladder dysfunction. Despite the controversial nature of this diagnosis, gallbladder dysfunction is the primary indication for cholecystectomy in up to 20% of adults and 50% of pediatric patients in the USA. Indeed, cholecystectomy for acalculous biliary pain is 3.5 times more frequent in the USA than in other developed countries, suggesting that it is over-used.
Patients who experience typical biliary pain but have no evidence of gallstones on transcutaneous US should undergo EUS to look for microlithiasis and sludge. If the result of EUS is negative, but the clinical history is classic for biliary-type abdominal pain, no further evaluation may be needed, because many patients with biliary pain, no stones on US, and normal gallbladder motility experience symptomatic improvement after cholecystectomy. If the pain history is atypical, the patient is likely to have a functional abdominal pain syndrome, and surgery should not be offered. If the clinical history is neither classic nor atypical, then gallbladder emptying may be assessed with scintigraphic imaging during intravenous infusion of CCK, although, as mentioned earlier, the ability of this test to predict response to cholecystectomy remains highly controversial.
A multidisciplinary consensus panel unanimously agreed that a large, multicenter RCT comparing surgery with conservative management in patients with typical biliary pain, a normal gallbladder ultrasound result, and abnormal CCK cholescintigraphy is necessary. Although, as mentioned earlier, the most natural role for this test may be in the evaluation of patients with neither classic nor atypical symptoms, the panel recommended that if CCK cholescintigraphy is considered, it should be reserved for patients with typical biliary pain (i.e., those meeting Rome IV Consensus Committee criteria [see Chapters 12, 14, 22,and 67 ]) who are not experiencing symptoms or hospitalized at the time of the test. Indeed, a prospective study of 93 subjects with a low gallbladder ejection fraction showed that patients with typical biliary pain had a substantially higher likelihood of responding to cholecystectomy than those with atypical symptoms (odds ratio 22.3, P <0.001). Conversely, some studies have demonstrated spontaneous symptom improvement without cholecystectomy in patients with atypical symptoms. The panel also recommended against making clinical decisions based solely on the provocation of pain by CCK infusion.
SOD is a benign, noncalculous obstructive disorder that occurs at the level of the SO. The pathogenesis of SOD can be divided into 2 subtypes: SO stenosis, which results from passive obstruction at the SO caused by fibrosis, inflammation, or both; and SO dyskinesia, which results from intermittent obstruction caused by sphincter muscle spasm. These 2 mechanisms of functional obstruction at the SO are not mutually exclusive. The term ampullary stenosis has generally been used interchangeably with the SO stenosis subtype.
The frequency of manometrically detected SO hypertension in patients with an intact gallbladder has not been well studied. Elevated basal SO pressure has been observed in 40% of patients with gallbladder stones, regardless of whether abdominal pain or elevated serum liver enzyme levels were present. It has also been reported that 70% of 81 patients with biliary-type pain and an intact gallbladder but no gallstones had delayed gallbladder emptying, SOD, or both. By contrast, a basal SO pressure elevation of greater than 30 mm Hg was not found in 50 asymptomatic volunteers without gallstones.
The frequency of SO hypertension in postcholecystectomy patients with persistent or recurrent biliary-type pain has been better studied but depends on the criteria for patient selection. Pain resembling preoperative biliary pain occurs in 10% to 20% of postcholecystectomy patients. The most common explanation for this pain is that the preoperative symptoms were not caused by gallbladder disease. The most likely diagnosis in this group of patients is a functional GI disorder such as IBS or functional dyspepsia. SOD has been reported in 9% to 14% of patients evaluated for postcholecystectomy pain. When other causes of postcholecystectomy pain have been excluded and SO manometry (SOM) has been performed in a more carefully screened group, the frequency of SOD has been reported to be 30% to 60%.
SOD has been associated with 3 clinical conditions: (1) persistent or recurrent biliary-type pain following cholecystectomy; (2) recurrent idiopathic (unexplained) pancreatitis; and (3) biliary-type pain in patients with an intact gallbladder but without cholelithiasis. SOD generally occurs spontaneously but has also been described with increased frequency in patients who have undergone LT, have AIDS, are chronic opium users, or have hyperlipidemia ( Table 63.1 ).
| Definite | Biliary-type pain after cholecystectomy |
|---|---|
| Probable | Biliary-type pain in a patient with an intact gallbladder |
| Possible | After LT |
| AIDS-associated viral and protozoal infections | |
| Chronic pancreatitis | |
| Hyperlipidemia | |
| Idiopathic recurrent acute pancreatitis | |
| Opium use |
Although biliary SOD has been diagnosed in all age groups, it is most common in middle-aged women. The female preponderance varies from 75% to 90%. The pain is typical of biliary pain; it is severe and occurs in the epigastrium or the RUQ and may radiate to the back or right shoulder blade. The pain is generally episodic, lasts more than 30 minutes, and occurs at least once a year. The Rome Consensus Committee has proposed diagnostic criteria for SO disorder, based predominantly on expert opinion ( http://www.romecriteria.org/criteria ). Although these criteria may be helpful in selecting patients who are most likely to benefit from intervention, they require prospective validation.
Because ERCP remains the only reliable diagnostic and therapeutic intervention for SOD, and brings with it substantial risks, defining the clinical characteristics that reliably predict the presence of SOD and the response to sphincter ablation is of paramount importance. Limited data suggest that patients are more likely to respond if their pain is intermittent, accompanied by nausea and vomiting, and absent for at least 1 year after cholecystectomy. Transient elevations of serum aminotransferase levels during attacks of pain support the diagnosis of SOD. A poor response to sphincterotomy (see later) has been associated with delayed gastric emptying, daily opioid use, and age less than 40 years. These predictors, however, have not been rigorously validated and, with the exception of elevated liver biochemical test levels, do not appear to play a clear role in clinical practice. An ongoing multicenter prospective cohort study (The RESPOnD Study) aims to rigorously characterize patients with suspected SOD who undergo ERCP with the ultimate objective of defining clinical and procedural characteristics associated with response to therapy.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here