Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Referrals for management of vascular access problems are among the most common requests for vascular intervention in centres where haemodialysis is performed.
Embrace the dialysis patients; they will be one of the most important training grounds for vascular access, catheter and wire manipulation, angiography, angioplasty/stenting and thrombolysis!
For patients on haemodialysis, their fistula, graft or dialysis catheter is a lifeline. Unfortunately, problems are common and anyone working on a site with a dialysis unit will frequently see patients with problematic access. Stenoses lead to inadequate dialysis, prolonged bleeding, arm oedema and thrombosis. Large shunts may cause steal phenomena. The key to these procedures is to understand the anatomy and the physical examination.
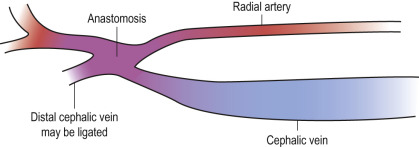
Patients with chronic kidney disease should have a fistula formed several months before they require dialysis, this allows the fistula to ‘mature’. The commonest fistula is the radio-cephalic (Brescia–Cimino) fistula fashioned at the wrist of the non-dominant arm ( Fig. 50.1 ). If this fails, it may be revised or a more proximal fistula formed, usually between the brachial artery and the cephalic or basilic vein. Sometimes the basilic vein is ‘transposed’ onto the brachial artery to increase the options. Once the non-dominant arm sites are exhausted, the dominant arm is used; if this fails, a fistula may be formed at the groin.
These are an alternative to fistula formation and have the advantages of being ready to use immediately and allowing higher flow rates. The price for this is the frequency with which they develop stenoses and thrombose. Grafts often have a loop configuration. Typical sites are between the brachial artery and the cephalic or basilic vein or between the femoral artery and vein.
Feel the fistula for the ‘thrill’ at the anastomosis and in the draining vein. The vein adjacent to the anastomosis usually has a spongy feel. If the fistula is underfilled, there is a problem with the inflow. A tense, distended vein indicates venous outflow obstruction. Venous stenoses are often palpable as ‘defects’ in the draining vein associated with a change in the degree of venous filling and thrill.
Hone your examination skills by trying to establish the problem and then confirming with ultrasound.
Imaging may be required to assess suitability for access formation and then to evaluate a maturing fistula. The majority of imaging comes about because of problems with the access.
Imaging is required whenever there is a problem relating to dialysis or the examination of the fistula. Typical problems are:
Pre-dialysis: reduced thrill, aneurysm development, difficulty needling, arm swelling
During dialysis: poor flow rates, recycling
Post-dialysis: prolonged bleeding.
The same questions need to be answered for both fistulae and grafts, namely, the state of the inflow, the condition of any anastomoses and the condition of the draining veins from the periphery to the central veins. Ultrasound is invariably the first-choice investigation and is ideally suited for the evaluation of anastomoses, as access sites are superficial. Ultrasound cannot demonstrate the central venous anatomy or the origins of the subclavian arteries. If there is a fistula in situ, then a DSA study of the fistula (fistulogram) will also image the central veins. Magnetic resonance angiography (MRA) or computed tomography angiography (CTA) are alternatives for central venous imaging.
CT is generally preferred to contrast-enhanced MRA due to the risk of nephrogenic systemic sclerosis.
Basic angiography set with a micro-puncture set
Ultrasound to guide puncture
You will need an arm-board to support the patient's arm slightly out from their side. Start with the patient's arm palm up. To cover from the chest to the wrist you will probably need to rotate the angiography table. Multiple oblique views are often necessary to sort out the anatomy.
To obtain oblique views, consider turning the patient's arm rather than rotating the C-arm.
Retrograde arterial puncture of the ipsilateral brachial artery or the inflow limb of the loop graft is the ideal method. Performing the study via a 3F arterial puncture optimizes visualization of the inflow and allows complete assessment. The alternative, which seldom produces satisfactory images, is to place a needle in the draining veins of the fistula and use a supra-systolic tourniquet to achieve retrograde flow through the arterial anastomosis.
Remember that the patient will be heparinized during dialysis so do not perform the study straight afterwards.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here