Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The organ at risk from carotid and vertebral artery disease is the brain. Central nervous system ischemia can be severely debilitating and even lethal. Vascular imaging has a major role in the diagnosis of all aspects of cerebrovascular disease. Catheter-based interventions are frequently utilized in the therapy of occlusive disease and acute stroke. This chapter focuses primarily on diagnosis and catheter-based interventions in the extracranial carotid and vertebral arteries, but also includes stroke treatment.
The right common carotid artery (CCA) arises from the brachiocephalic artery, while the left CCA usually originates directly from the aortic arch ( Fig. 5-1 ). The common carotid arteries ascend through the mediastinum and lie posterior and medial to the internal jugular veins in the neck (see Fig. 2-41 ). Typical internal diameters of the CCA are 6-8 mm. The CCA bifurcates into the external carotid artery (ECA) and internal carotid artery (ICA) in the upper neck, typically at the upper edge of the thyroid cartilage (between the third and fifth cervical vertebrae). The ICA arises posterolateral to the ECA in approximately 90% of individuals; a medial origin is present in the remaining 10%. The ICA and ECA are normally the only branches of the CCA; small cervical branches directly from the CCA are extremely rare ( Fig. 5-2 ).


The ECA supplies the structures of the neck, face, and scalp ( Fig. 5-3 ). The ECA branches that supply the midline structures of the face frequently anastomose with one another. Many memorable (but unprintable) mnemonics have been devised for the branches of the ECA.

The ICA is usually a branchless vessel until it reaches the base of the skull ( Fig. 5-4 ). The internal diameter of this vessel ranges from 4 to 6 mm. Rarely, persistent embryonic branches to the basilar artery from the cervical ICA may be encountered at the C1-C2 (persistent hypoglossal artery) and C2-C3 (proatlantal intersegmental artery) levels. At the skull base the internal carotid artery enters the serpentine carotid canal within the petrous bone, traveling medial and anterior toward the cavernous sinus. Small branches can communicate from this portion of the ICA with the internal maxillary artery. The ICA exits the petrous canal into the cavernous sinus. An anomalous branch from the cavernous ICA to the basilar artery, the persistent trigeminal artery, is found in 0.5% of patients ( Fig. 5-5 ). Typically, the ophthalmic artery is the first major branch of the distal ICA, arising just above the cavernous sinus. The posterior communicating and anterior choroidal arteries arise from the ICA within the subarachnoid space just before the bifurcation into anterior and middle cerebral arteries.


The vertebral arteries arise from the proximal subclavian arteries in almost 95% of patients, traveling in a posterior and medial direction toward the skull ( Fig. 5-6 ). In 5% of patients the left vertebral artery arises directly from the aortic arch. The diameter of the cervical vertebral artery is 3-5 mm. The left vertebral artery is equal to or larger than the right in 75% of individuals. Unlike the CCA and ICA, the cervical portion of the vertebral artery has many small unnamed muscular branches. The vertebral arteries lie within a series of bony rings formed by the transverse processes of C6 or C5 to C1, before looping posteriorly into the spinal canal between the skull base and C1 (see Fig. 5-4 ). The segment from the artery origin to where it enters the lowest transverse process is termed V1 ; the section within the transverse processes up to C2 is V2 ; the section between C2 and the spinal canal is V3 ; the final section (V4) travels medially through foramen magnum to the basilar artery. Within the skull the vertebral arteries are subarachnoid and give rise to the posterior inferior cerebellar arteries before joining to form the basilar artery. The basilar artery, which runs along the posterior surface of the clivus, terminates by branching into the posterior cerebral arteries. Numerous small branches to the pons, as well as the paired anterior inferior and superior cerebellar arteries, arise from the basilar artery before it bifurcates.

The majority of anatomic variations of the CCA, ICA, and vertebral arteries occur at vessel origins ( Table 5-1 ). These anomalies are related to the development of the thoracic arch (see Chapter 9 ).
| Variant | Incidence |
|---|---|
| Left common carotid artery from brachiocephalic artery (“bovine arch”) | 22% |
| Left vertebral artery directly from aortic arch | 5% |
| Combined left common carotid and left subclavian artery origin | 1% |
| Aberrant right subclavian artery (last branch from aortic arch) | 1% |
| Persistent trigeminal artery | 0.5% |
| Persistent hypoglossal artery | 0.03% |
| Congenital absence of the internal carotid artery | 0.01% |
There are two levels of cerebrovascular collaterals: extracranial and intracranial. The ECA is an important source of collateral blood supply to both the ipsilateral and contralateral ICA. In the setting of a proximal ICA occlusion, retrograde flow in the ophthalmic artery can reconstitute the intracranial portion of the distal ICA, thus supplying the brain ( Fig. 5-7 ). With occlusion of a CCA, collateral flow from the contralateral ECA and the ipsilateral vertebral artery can reconstitute the cervical ICA ( Fig. 5-8 ). Rarely, the superficial temporal and middle meningeal arteries can provide collateral supply through the skull to leptomeningeal arteries on the surface of the brain.


In the neck, the vertebral artery is an additional potential source of collateral blood supply to the carotid arteries. Muscular branches of the vertebral artery communicate with the occipital branch of the ECA, which can then reconstitute the ICA. Conversely, the ECA can provide collateral blood supply to the distal cervical vertebral artery through the same pathway. The distal cervical vertebral artery can be reconstituted by muscular arteries of the neck such as the ascending cervical artery.
Within the skull the anterior (carotid) and posterior (vertebral) circulations communicate through a vascular ring, the circle of Willis, located at the base of the brain ( Fig. 5-9 ). This network potentially allows perfusion of the entire brain via any one of four vessels that supply the head. Similarly, the circle of Willis serves as a potential collateral pathway to the upper extremities. The circle of Willis is incomplete or contains hypoplastic elements in more than 50% of individuals. One or both posterior communicating arteries are absent in up to a third of patients. A hypoplastic or absent A1 segment of the anterior cerebral artery is found in approximately 15%. The posterior cerebral artery arises directly from the ICA in up to 20%. These variants can occur in isolation or in conjunction with other circle anomalies.

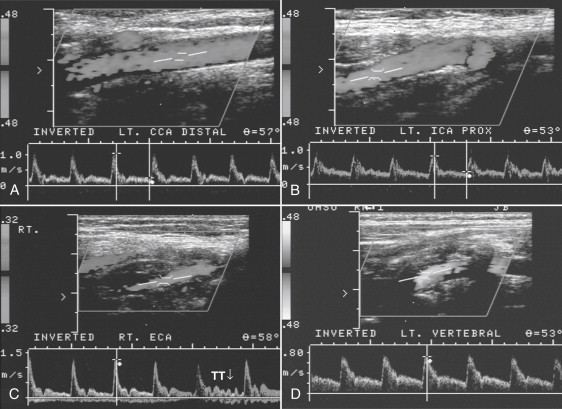
The most widely used imaging tool for the extracranial cerebral circulation is ultrasound with pulsed Doppler and duplex color flow. Grayscale imaging with a 4- to 7.5-MHz linear array transducer is sufficient in most patients to identify the CCA, ICA, ECA, and areas of plaque. Grayscale imaging alone does not perform well in the determination of the degree of stenosis, because hypoechoic “soft” plaque may be indistinguishable from the residual lumen, and calcification in the anterior wall of the vessel can reflect the ultrasound beam so that the lumen cannot be visualized. Sometimes it can be difficult to distinguish the ICA from the ECA. Doppler interrogation of flow improves identification of the vessels and quantification of stenoses. The normal CCA, ICA, and ECA have distinctive Doppler waveforms ( Fig. 5-10 ). The CCA, ICA, and vertebral artery have low-resistance waveforms, whereas the ECA has a high-resistance waveform. Color flow is helpful in localizing vessels and selecting the best place to measure velocities in a stenosis.
The intracranial arteries cannot be directly visualized with current ultrasound units owing to the reflective properties of the skull. Transcranial Doppler (TCD) uses low-frequency (2-MHz) pulsed-wave Doppler to evaluate the intracranial arteries. The low-frequency sound waves can penetrate the thinner portions of the skull. The arteries of the circle of Willis can be evaluated through the temporal bone, the ophthalmic artery through the orbit, and the vertebral artery through the foramen magnum. Direction of flow and alterations in flow velocity and waveforms can be used to infer the presence of occlusive disease.
A number of potential pitfalls exist with carotid ultrasound. The quality of the study is dependent upon a skilled and knowledgeable sonographer. The great vessel origins cannot be reliably imaged. A complete study may not be possible in a patient with a high carotid artery bifurcation situated behind the ramus of the mandible. Lastly, the cervical vertebral arteries are difficult to image in their entirety with ultrasound owing to the surrounding bony vertebra, although direction of flow can be readily determined.
The cervical vessels are excellent subjects for magnetic resonance angiography (MRA). Imaging should cover from the arch to the circle of Willis (intracranial MRA requires dedicated imaging sequences). Two-dimensional (2-D) and three-dimensional (3-D) time-of-flight (TOF) MRA with a superior saturation band were the first clinically useful techniques developed for imaging the cervical arteries. The superior saturation band eliminates jugular venous flow, but also masks reversed flow in a vertebral artery. Calcification of lesions does not impair the ability of MRA to image the carotid arteries, but the degree of stenosis is routinely overestimated. The 3-D techniques provide higher resolution than 2-D, but the area imaged is much smaller. The great vessel origins cannot be adequately evaluated with TOF, and flow in kinked or tortuous carotid arteries loses signal due to saturation. Lastly, very slow flow distal to a severe stenosis may become completely saturated and produce no signal, so that the vessel appears occluded.
Dynamic gadolinium-enhanced 3-D sequences overcome many of the limitations of TOF carotid MRA. Rapid acquisitions during breath-holding are necessary to avoid enhancement of the adjacent jugular veins. However, stenosis, tortuosity, and slow flow do not impair gadolinium-enhanced 3-D carotid MRA. The absence of signal loss from turbulence allows more accurate grading of stenoses. A larger field of view may be used than with TOF MRA, so that diagnostic images can be obtained from origin of the great vessels to the carotid siphon ( Fig. 5-11 ). Dedicated separate sequences should be used to image the circle of Willis and the intracranial circulation. When coupled with anatomic and perfusion/diffusion brain imaging, MR with MRA has the potential to provide complete cerebrovascular evaluation.

Limitations of all forms of carotid MRA include signal loss due to presence of metal (e.g., stents or adjacent surgical clips), motion artifacts (e.g., when swallowing or yodeling during the study), and spatial image resolution.
Computed tomography angiography (CTA) is also used extensively to image the cervical carotid and vertebral arteries (see Fig. 5-4 ). Rapid bolus injection of iodinated contrast with a short delay is necessary to avoid venous enhancement. Imaging should be inclusive from the arch through the brain. Thin slices and careful postprocessing allows accurate evaluation of stenoses, dissections, and aneurysmal disease. Slow flow in a vessel distal to a pinpoint lesion can be reliably detected with CTA, although reversed flow cannot be distinguished from flow in the normal direction. The degree of vascular calcification is readily apparent, but metal in the teeth or cervical spine can create limiting streak artifacts. Major advantages of CTA are that image acquisition times are short (and includes the brain), the adjacent soft tissues can be evaluated as well, and CT scanners are readily available.
Imaging of atherosclerotic plaque is of great interest in the cervical carotid, in that plaque composition as well as degree of stenosis influences the risk of stroke. Plaques with a lipid core greater than 25%, a thin overlying fibrous cap, or intraplaque hemorrhage are associated with an increased stroke risk (“vulnerable plaque”). Plaque imaging is not yet mainstream, but several techniques appear promising. These include high-resolution magnetic resonance imaging (MRI) that can identify plaque components and internal hemorrhage, as well as positron-emission tomography (PET) CT or MRI in which increased metabolic activity is associated with vulnerable plaque. Characterization of the plaque components may become an essential part of carotid imaging for atherosclerotic disease.
Catheter angiography of the extracranial carotid and vertebral arteries is the standard against which other imaging modalities have been validated. Although infrequently used for diagnosis, this modality remains important for resolving diagnostic dilemmas and for interventions. The study should begin with a flush aortic injection through a 5-French pigtail catheter positioned so that the side holes are in the transverse portion of the aortic arch. Filming should be rapid (4-6 frames per second) in the left anterior oblique (LAO) projection (the exact degree depends on patient anatomy, but is usually about 45 degrees). This obliquity opens up the arch to show the origins of the brachiocephalic, left common carotid, and left subclavian vessels to best advantage. If there is a question about the right common carotid or subclavian artery origin, a second injection in the right anterior oblique (RAO) projection should be obtained (see Fig. 5-1 ). The common carotid arteries can be selected with 5-French catheters, usually with an H-1, Davis, or Berenstein-type shape. When the great vessels arise from the arch at a steep angle, a Simmons shape (S1 for the left CCA and S2 for the right CCA) may be necessary. A short segment (1-2 cm) of soft guidewire (e.g., Bentson) should protrude from the tip of the catheter during selection of the vessel to minimize the risk of trauma. Selection of the ICA and ECA can be accomplished with the same catheters and a hydrophilic-coated or a Bentson guidewire. Carotid injections should be viewed in two planes, usually anteroposterior (AP) and lateral ( Table 5-2 ). Imaging in an anterior oblique view may be necessary to profile ICA and ECA origins.
| Location | Injection Rate | Total Volume | Projections | Filming Rate | Duration |
|---|---|---|---|---|---|
| Arch | 20-25 mL/sec | 30-50 mL | LAO, RAO | 4-6 sec | 10 sec |
| CCA | 7-9 mL/sec | 11-12 mL | AP, Lat, AO | 2-4 sec | 15 sec |
| ECA | 2-4 mL/sec | 4-6 mL | AP, Lat | 2-4 sec | 15 sec |
| ICA | 6-7 mL/sec | 8-9 mL | AP, Lat, AO | 2-4 sec | 20 sec |
| Vertebral | 3-5 mL/sec | 5-7 mL | AP, Lat | 2-4 sec | 15 sec |
Vertebral arteries are selected with the same catheter shapes used for the CCA. An H-1, Davis, or Berenstein catheter is advanced into the subclavian artery, rotated so that the tip points superiorly, and gently withdrawn with intermittent puffs of contrast until the vertebral artery orifice is engaged. Careful selection of the vertebral artery is then performed with a hydrophilic or Bentson guidewire. When selection of the vertebral artery is difficult, a subclavian artery angiogram with the ipsilateral brachial artery outflow temporarily occluded with a blood pressure cuff inflated to suprasystolic pressures will opacify the vertebral artery. Vertebral artery angiograms should be performed in at least two planes (AP and lateral) (see Fig. 5-6 ).
In the unusual situation of performing selective carotid angiography from the upper extremity approach, the preferred access is in the right arm. A Simmons 1 catheter (see Fig. 2-39 ) can be used to select both carotid arteries. Selection of the right CCA from a left arm access can be challenging and usually requires a Simmons 2 catheter.
Extreme care is necessary when manipulating or flushing any catheter in the aortic arch or cerebral vessels, because small thrombi or air bubbles create huge problems in this vascular bed. Double flush all catheters in these locations every 90 seconds. Many angiographers administer a bolus of 3000-5000 U of heparin during diagnostic studies after obtaining vascular access. The overall risk of permanent stroke during cerebral angiography is about 0.5% with current techniques and equipment. Reversible ischemic events occur in as many as 2% of patients. In patients with ongoing transient ischemic attacks (TIAs), the neurologic complication rates are slightly higher.
The most common pathologic condition in the extracranial carotid and vertebral arteries is occlusive atherosclerotic disease. About 7% of adults older than 65 years of age have asymptomatic narrowing of cervical carotid arteries of 50% or more due to atherosclerosis. More than 90% of carotid artery stenoses are localized to the bifurcation of the CCA or the proximal ICA ( Fig. 5-12 ). Origin stenoses of the common carotid artery are present in fewer than 5% of patients with concurrent disease at the CCA bifurcation (see Fig. 5-8 ). Similarly, occlusive disease in the distal ICA is found in 5% of patients with ICA bifurcation disease. Stenoses of the cervical vertebral arteries are found in approximately one third of patients with ICA stenosis, but are rarely symptomatic.

The risk to patients from carotid atherosclerosis is stroke, with about 15% of all strokes thought to be due to debris or thrombus from carotid plaque ( Boxes 5-1 and 5-2 ). Asymptomatic stenosis of the internal carotid artery of less than 75% has only a 1% yearly risk of stroke, which increases to 2%-5% for tighter lesions. Symptomatic lesions (i.e., those causing reversible episodes of cerebral ischemia, or TIAs) have stroke rates approaching 35% over 5 years. The characteristics of the carotid plaque influence the risk of stroke, with softer, more vulnerable plaques having a higher risk.
Smoking
Hypertension
Diabetes
Elevated cholesterol
Male sex
Advanced age
African-American or Asian
Family history
Hemiplegia
Hemiparesis
Aphasia, dominant hemisphere
Neglect, nondominant hemisphere
Gaze deviation toward affected hemisphere
The most widely accepted criteria of carotid stenosis on MRA, CTA, and catheter angiography uses the ratio of the diameter of the lumen at the point of maximal stenosis to the diameter of the lumen in the closest normal nontapered segment of cervical internal carotid artery (the NASCET technique: North American Symptomatic Carotid Endarterectomy Trial) ( Fig. 5-13 ). The estimated or true maximal diameter of the ICA bulb or CCA is less accurate and should not be used. A method to calibrate measurements during angiography is to place a radiopaque object with a known diameter on the ipsilateral neck as a reference (especially for sizing stents and balloons).
![Figure 5-13, Technique to measure internal carotid artery (ICA) stenosis. The diameter of the lumen in the most narrow portion is divided by the diameter of the most normal appearing adjacent cervical ICA. The degree of stenosis is [(B − A)/B] × 100. Figure 5-13, Technique to measure internal carotid artery (ICA) stenosis. The diameter of the lumen in the most narrow portion is divided by the diameter of the most normal appearing adjacent cervical ICA. The degree of stenosis is [(B − A)/B] × 100.](https://storage.googleapis.com/dl.dentistrykey.com/clinical/CarotidandVertebralArteries/12_3s20B978032304584100005X.jpg)
The mechanism of stroke due to carotid disease is predominantly embolic, either from thrombus or platelet aggregates that form within a lesion, or debris released when an unstable plaque ruptures into the vessel lumen. Irregularities of the plaque surface that look like pits are termed ulcers and may have a higher propensity for causing stroke (see Fig. 5-12 ). Acute carotid occlusion or extreme carotid stenosis can result in ipsilateral stroke when the intracranial collateral circulation is insufficient or thrombus embolizes from the ICA, but cases with adequate collateral perfusion may remain clinically silent.
Patients with carotid stenosis may present with symptoms of transient cerebral or retinal ischemia, presumably due to small emboli that spontaneously lyse or fragment. A TIA is manifested clinically by a neurologic or visual abnormality that usually reverses completely within minutes, but may last up to 24 hours. The risk of a stroke increases 10-fold in patients experiencing TIAs, but only one third of patients with carotid distribution TIAs have moderate or severe carotid artery disease. In other words, plaque composition and degree of stenosis influences risk, and cardiac and aortic sources of emboli are common.
Vertebral and basilar artery occlusive disease has a different clinical presentation than ICA stenosis. The neurologic territory at risk involves the brainstem, cerebellum, and posterior cerebral lobes. Occlusive disease of the posterior circulation results in a complex of symptoms referred to as vertebrobasilar syndrome ( Box 5-3 ). Asymptomatic moderate to severe vertebral artery stenoses result in stroke in about 5% of patients. Patients with TIAs related to posterior circulation lesions have a risk of subsequent stroke of about 22% within 90 days. The anatomic distribution of symptomatic lesions is predominantly at or near the vertebral artery origin (V1 and V2), with about 8% occurring in the basilar artery. Occlusive lesions of the subclavian artery origin cause retrograde flow in the ipsilateral vertebral artery which results in vertebrobasilar syndrome in 25% of patients (see Fig. 3-11 ).
Bilateral motor/sensory deficits
Ataxia
Diplopia
Dysarthria
Dysmetria
Bilateral homonymous hemianopsia
When carotid occlusive disease is suspected, the first imaging examination for the majority of patients is grayscale and Doppler ultrasound ( Fig. 5-14 ). Velocity measurements proximal, within, and distal to the area of stenosis allow accurate determination of the degree of stenosis ( Table 5-3 ). The flow through an area of stenosis is at first accelerated and remains so until the lumen becomes severely narrowed. Flow then decreases and may be barely detectable by ultrasound. Doppler waveforms distal to the stenosis broaden with first loss in amplitude and ultimately loss of pulsatility. The generally accepted sensitivity and specificity of ultrasound for clinically significant carotid stenosis are each greater than 90%.

| Stenosis | PSV (cm/s) | Plaque (%) | EDV (cm/s) | VICA/VCCA |
|---|---|---|---|---|
| <50% | <120-139 | <50 | <40 | <2 |
| 50%-69% | 140-230 | ≥50 | 40-100 | 2-4 |
| >70% ∗ | >230 | >50 | >100 | >4 |
∗ For asymptomatic patients, consider using PSV, EDV, and VICA/VCCA to increase positive predictive value.
The presence of severe disease or occlusion in one ICA may result in ultrasound overestimation of the degree of stenosis in the other ICA owing to normal compensatory increased flow. A pinpoint residual ICA lumen with very slow distal flow may be indistinguishable from a total occlusion by ultrasound. This distinction is important because the management is different (see later).
Contrast-enhanced MRA has a sensitivity of greater than 90% and a specificity of greater than 90% for the detection of hemodynamically significant (>50% reduction in luminal diameter) carotid stenosis ( Fig. 5-15 ). However, as a rule, the degree of stenosis is overestimated by MRA, particularly on 2-D TOF sequences. Precise determination of the degree of stenosis requires high-resolution gadolinium-enhanced 3-D sequences. The vertebral arteries are reliably imaged with MRA techniques. The origins at the subclavian arteries or arch can be seen best with gadolinium enhanced 3-D sequences, although motion artifact can degrade images.

The sensitivity and specificity of CTA for detection of carotid stenoses are reportedly slightly less than MRA, but are also greater than 90% each ( Fig. 5-16 ). The vertebral arteries can be evaluated for patency, but direction of flow cannot be determined. Heavily calcified plaque, streak artifact from dental amalgam, and vascular tortuosity can make image interpretation difficult.

Selective common carotid angiography remains widely accepted as a reliable technique for evaluation of ICA stenosis. However, owing to the cost, patient inconvenience, and small risk of stroke, routine use of angiography for diagnosis alone is uncommon. The current indications for catheter angiography include discordant results of noninvasive imaging modalities, technically inadequate noninvasive studies, suspected concurrent great vessel origin or intracranial ICA occlusive disease, and differentiation of severe stenosis from occlusion of the ICA. In the later case, delayed filming in the lateral plane should be obtained in order to detect a “string sign” ( Fig. 5-17 ).

There continues to be great debate over intervention for ICA stenosis. The debate is framed by the morbidity and mortality associated with the intervention versus the risk associated with medical management. Medical management, surgical technique, and catheter-based interventions have all improved rapidly, making comparisons at one point in time difficult to extrapolate to current clinical practice. Furthermore, randomized prospective controlled trials necessarily study homogeneous patient populations that do not reflect the variety of daily practice. Nevertheless, the intervention that is still used as a benchmark is surgical carotid endarterectomy (CEA), which has a reported operative stroke rate of 2%-3%, mortality of less than 1%, cranial nerve injury in 1%-2%, and a symptomatic restenosis rate of 1%-2% ( Fig. 5-18 ). The adoption of surgical patch angioplasty rather than eversion endarterectomy has further decreased restenosis rates.

A number of prospective studies comparing CEA with medical therapy profoundly influenced the management and subsequent investigation of this disease. The North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST), both reported in the 1990s, were randomized comparisons of optimal medical therapy (of that time) and combined CEA and medical therapy in patients with symptomatic carotid stenosis. For patients with 70%-99% stenoses, the cumulative risks of any ipsilateral stroke at 2 years were 26% and 32% (NASCET and ECST, respectively) in the medical patients and 9% and 16% (NASCET and ECST, respectively) in the surgical patients. In the NASCET trial, the risk for a major or fatal ipsilateral stroke was 13.1% for medical patients versus 2.5% for surgical patients. The risk reduction for symptomatic patients with 50%-70% stenoses was less pronounced, but still significant.
Asymptomatic patients were studied in the Asymptomatic Carotid Atherosclerosis Study (ACAS), the Veterans Affairs Cooperative Study Group, and the Asymptomatic Carotid Surgery Trial. In these studies, asymptomatic men and women with 60% or greater stenoses of the ICA were randomized to either CEA and medical therapy or medical therapy alone. The risk of stroke or death within 30 days of surgery was up to 3.3% in the CEA group, significantly higher than the first 30 days of medical therapy. However, over time, CEA patients fared better. In the ACAS trial the aggregate risk of stroke at 5 years was 5.1% for the surgical group and 11% for medical therapy. These studies established 60% diameter reduction of the ICA as the threshold for intervention in patients with asymptomatic stenoses.
Carotid artery stenting (CAS) is undergoing intensive investigation as an alternative to CEA. The studies have evolved as techniques and devices have matured, skills improved, and target patient populations changed. For example, in the Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVATAS), only high-risk surgical patients were included, distal protection was not available, and stents were not used in all patients. However, this study did show that, when used, stents reduced the risk of procedural stroke compared to angioplasty alone. In the Stenting and Angioplasty with Protection in Patients at Risk for Endarterectomy study (SAPPHIRE), distal protection and dedicated stents were used in all patients. The majority of patients had asymptomatic carotid stenosis. There was an initial advantage of CAS over CEA, with 1-year risk of stroke or death at 1.9% versus 5.3%, respectively. At 3 years, the two treatments became equivalent.
The Stent-protected Percutaneous Angioplasty of the Carotid vs. Endarterectomy (SPACE) trial studied symptomatic patients with greater than 50% stenosis. Distal protection devices were used in only 27% of CAS cases. This study demonstrated no difference in ipsilateral stroke that persisted through 2 years. Another study, the Endarterectomy vs. Angioplasty in Patients with Symptomatic Severe Carotid Stenosis (EVA-3S) was stopped early due to safety concerns related to high stroke rates in CAS patients. Distal protection was initially not mandated in the study, and operators with limited experience were allowed to participate.
The International Carotid Stenting Study (ICSS) and the Carotid Revascularization Endarterectomy vs. Stenting Trial (CREST) are the two largest studies of CAS. Asymptomatic and symptomatic patients were included. The ICSS trial allowed a variety of stents and distal protection was used in 72% of patients. At 120 days, the incidence of stroke, death, or procedural myocardial infarction (MI) was 8.5% and 5.2% for CAS and CEA, respectively, a significant difference. The CREST trial was not only larger, but had a strict credentialing process for investigators and uniformity in the stent and protection device (with 96% application). The primary endpoint was any periprocedural stroke, MI, death, or postprocedural ipsilateral stroke for up to 4 years. At 2.5 years, there was no significant difference (7.2% and 6.8% for CAS and CEA, respectively), but there were more strokes in the CAS group and more MIs in the CEA group during the first 30 days whether analyzed in aggregate or by symptom status. Interestingly, the rate of stroke and death in the CAS patients at 30 days for both symptomatic (6%) and asymptomatic patients (2.5%) were equivalent to those reported for CEA in the ACAS and NASCET trials.
The indications for carotid stenting are in flux, and local talent has great influence on which procedure to perform. Assuming the availability of both skilled interventionalists and surgeons, for symptomatic patients younger than 70 years with low surgical risk, CAS and CEA are equivalent in terms of overall outcomes, with the tradeoff between increased stroke in CAS and increased MI and cranial nerve injury in CEA. In patients younger than 60 years, the stroke outcomes with CAS may be better than with CEA. Symptomatic patients at high surgical risk are good candidates for CAS, but age older than 80 years increases CAS risk substantially. Asymptomatic patients are more challenging to triage, but CAS should be considered in patients with greater than 70% stenosis and high surgical risk.
Carotid stenting should be performed within the context of adequate training in the technique, competence in cerebral angiography (performance and interpretation), and access to specialty stroke-related support. Meticulous technique is essential during carotid stent procedures (one small air bubble can ruin everything). A standardized catheter and sheath flush protocol should be in place, with careful debubbling of all pressure infusion set-ups for sheaths. Patients at increased risk of procedural complication with CAS include those with poor access (i.e., tortuous or diseased iliac arteries, thoracic aorta, or carotid arteries), heavily calcified lesions, age older than 80 years, and multiple or tandem lesions, especially those involving the carotid siphon.
A very important component of the procedure is the use of a cerebral embolic protection apparatus. The two basic approaches to cerebral protection are distal ICA filters or occlusion, or flow reversal in the ICA ( Fig. 5-19 and see Fig. 4-19 ). Distal devices require crossing the lesion in order to position the protection system but allow continued antegrade cerebral perfusion, whereas flow reversal systems require an intact circle of Willis and positioning of occlusion balloons in the CCA and ECA to control inflow. Distal protection devices can induce spasm in the ICA, which resolves with removal of the device. Each patient and lesion should be evaluated for suitability for the available devices, because no single device can be used for every patient or lesion.

The patient undergoing carotid artery stenting should be pretreated with dual antiplatelet medication such as clopidogrel and aspirin, and anticoagulated during the procedure with heparin. A 6- or 7-French guiding catheter in the carotid artery is necessary to provide a stable working platform. The lesion is carefully crossed, a protection device deployed, the lesion predilated with an undersized balloon using short inflation times, a self-expanding stent deployed with or without postdilation, angiographic confirmation of a satisfactory result, and then removal of the protection device ( Fig. 5-20 ). Dedicated balloon and stent systems that use 0.014- to 0.018-inch guidewires are often used. Typical angioplasty balloon diameters are 4-6 mm for the ICA. Self-expanding stents are preferred in this region, because it is subject to rotation and external compression, which could crush a balloon-expandable stent. Perhaps more important, self-expanding stents conform better to the anatomy, which can involve disparate diameter vessels and tortuosity. Stent placement across the origin of the ECA is frequently necessary to adequately treat ICA-origin stenoses and is well tolerated. Stretching of the carotid bulb during the procedure can trigger a reflex bradycardia or asystole, so atropine 1 mg should be available or given intravenously before balloon inflation, and a transvenous or transcutaneous pacemaker should be close at hand. Persistent hypotension for 12-24 hours can also occur, such that close hemodynamic monitoring overnight is required. The goal of stenting is to increase flow across the lesion, not make it equal or better than new. This is a vascular bed in which the old adage “the enemy of good is better” applies.

Patients can be followed with duplex ultrasound or angiography. The restenosis rate (>70%) is approximately 3%-6% over 4 years, with a similar incidence of stent fractures.
The endovascular treatment of symptomatic vertebral artery atherosclerotic stenosis depends on the location of the lesion. Balloon-expandable stent placement in origin lesions produces relief of symptoms, with a restenosis rate of approximately 10% at 1 year, and subsequent stroke is less than 2%. The restenosis rate may be reduced with the use of drug-eluting stents.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here