Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Acute cholecystitis (AC) is a prevalent condition that carries significant risks of morbidity and mortality. AC may present with a spectrum of disease stages ranging from a mild self-limited illness to a fulminant potentially life-threatening illness. The 2018 Tokyo guidelines for the management of AC stratifies each presentation as mild (Grade I), moderate (Grade II), or severe (Grade III) based on clinical and biochemical parameters Patients presenting with Grade III AC will manifest systemic symptoms due to organ damage. Although laparoscopic or open surgical removal of the inflamed gallbladder remains the gold standard therapy when the patient is a surgical candidate, patients with moderate or severe AC often require early biliary drainage to control the gallbladder inflammation. This minimally invasive nonsurgical approach has been suggested as a definitive therapy in critically ill and elderly patients, as well as to provide a bridge to surgery. The overall goal of percutaneous cholecystostomy (PC) is gallbladder decompression and drainage for prevention of gallbladder perforation and sepsis. The technique of PC also offers a minimally invasive means of access to the biliary system for other interventions such as stent placement and stone retrieval. The technical success rate for PC is high and the complication rate is low.
There are two primary clinical reasons patients are referred for PC:
To decompress the gallbladder for management of cholecystitis or, less commonly, acute cholangitis.
To provide a portal of access to the biliary tract for therapeutic purposes.
A multidisciplinary approach to determine whether to proceed with PC is ideal and should be guided by clinical symptomatology, laboratory data, and supporting imaging evidence. The clinical manifestations of cholecystitis include fever, elevated white blood cell count, right upper quadrant pain, and Murphy sign. Patients may suffer from either calculous or acalculous cholecystitis ( Figs. 95.1, 95.2, 95.3, 95.4, and 95.5 ). Those with calculous cholecystitis have gallstones, and possibly sludge, causing mechanical obstruction of the cystic duct. The exact pathogenesis of acalculous cholecystitis is unclear but tends to occur in the critically ill, debilitated, or intensive care patient. Associations with diabetes, malignant disease, vasculitis, and congestive heart failure also exist. It can also occur secondary to mechanical obstruction of the cystic duct from biliary stent placement in the common bile duct. Empirical cholecystostomy may be indicated in patients with fever of unknown origin or other clinical evidence of sepsis where there is no apparent source other than classic imaging features of cholecystitis.
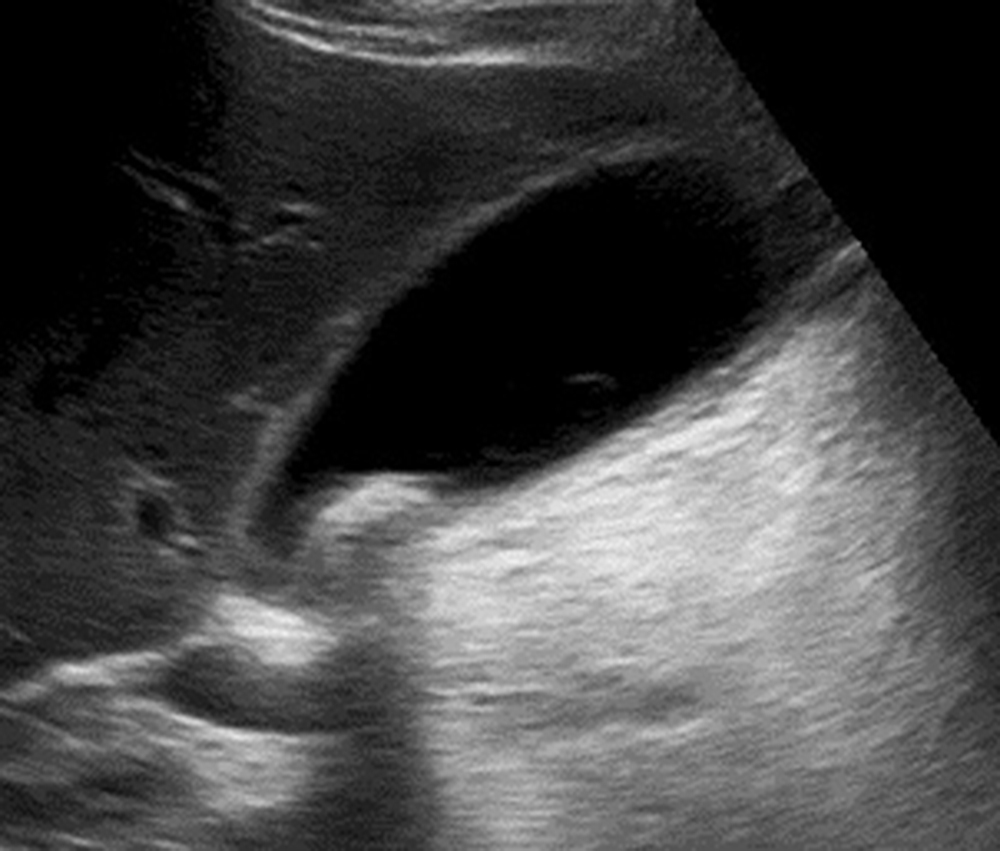
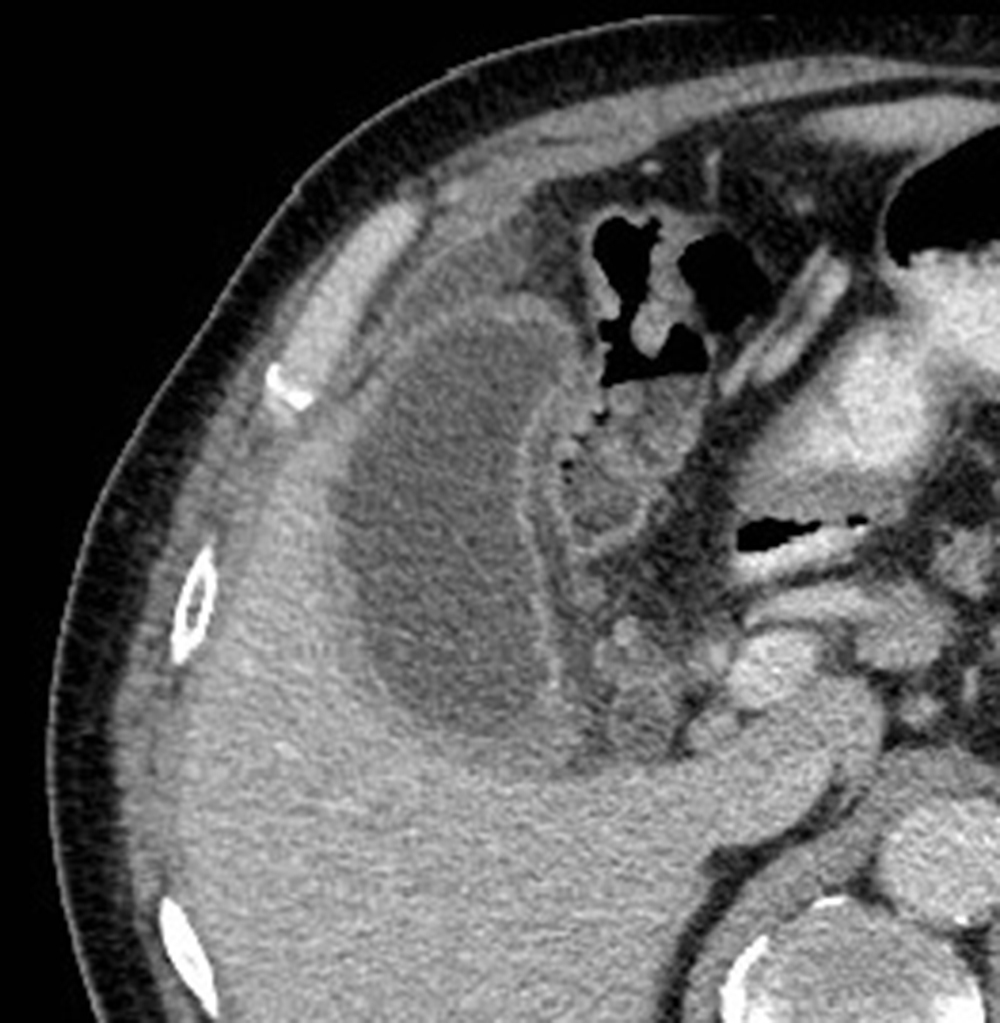
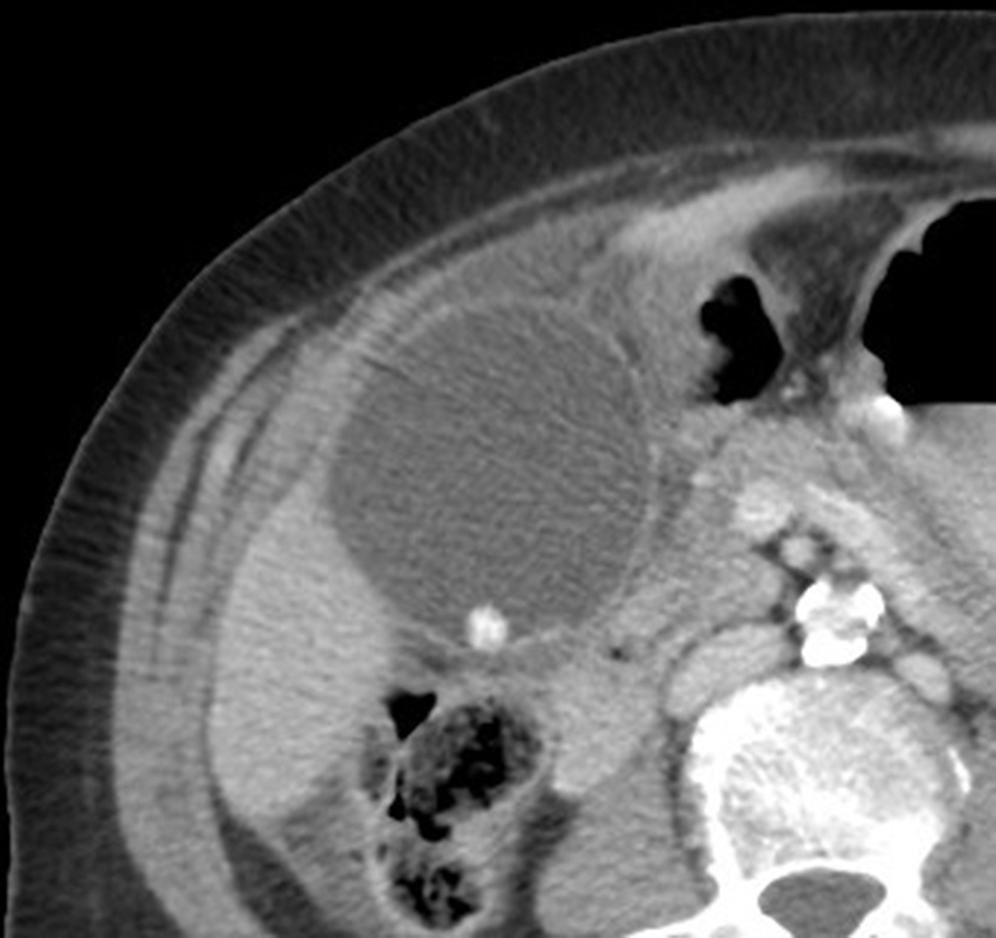
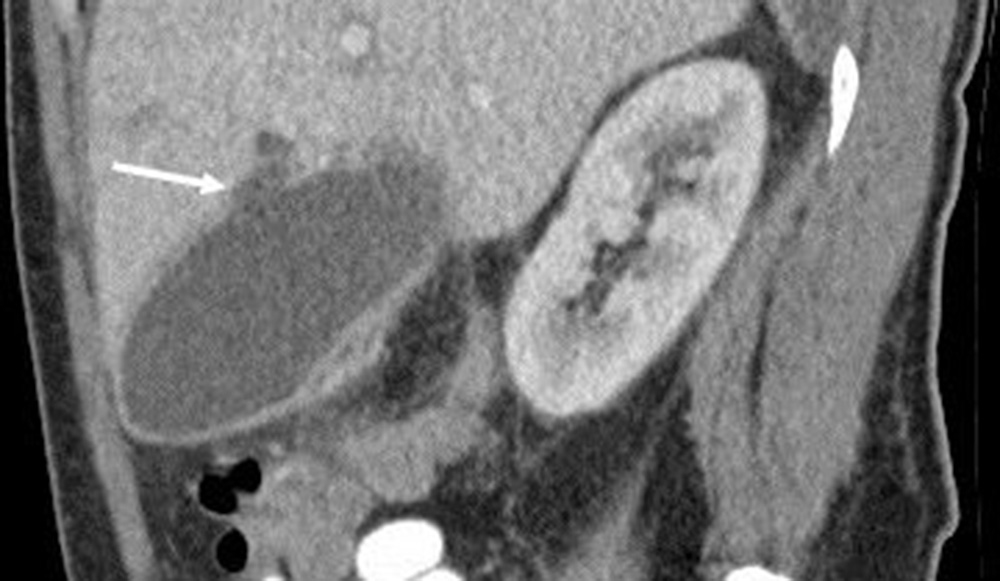

Sonographic, computed tomography (CT), or magnetic resonance imaging findings of uncomplicated cholecystitis include gallbladder-wall thickening, pericholecystic fluid/stranding, gallbladder distension, sonographic Murphy sign (right upper quadrant pain with probe pressure), or a gallstone impacted in the neck of the gallbladder or cystic duct ( Fig. 95.6 ). Findings of complicated cholecystitis such as a pericholecystic abscess ( Fig. 95.4 ), intraluminal membranes, and/or gas suggest a gangrenous or perforated gallbladder ( Fig. 95.7 ). Mortality rates in cases of gallbladder perforation range from 12% to 16%. Hepatobiliary nuclear scintigraphy with technetium-99m iminodiacetic acid derivatives provides highly specific diagnostic confirmation, with nonvisualization of the gallbladder at 4 hours suggesting cystic duct obstruction and cholecystitis.


PC may also be employed as a means to access the biliary system when transhepatic or endoscopic routes are not feasible or contraindicated. This portal to the biliary system provides a pathway for a variety of therapeutic interventions, including internal/external biliary drain placement, metallic stent placement, gallstone extraction, dissolution, lithotripsy, and even gallbladder ablation.
Although PC is seldom the first-line treatment in the management of AC, it is frequently performed in gravely ill and high-risk patients, and there are few absolute contraindications. Interposed bowel (e.g., as in Chilaiditi syndrome) may preclude safe access to the gallbladder. Coagulopathy is a relative contraindication, and a severe bleeding diathesis may not allow transhepatic access. Other relative contraindications include gallbladder tumor that may be seeded by percutaneous access, or a gallbladder greatly distended by calculi ( Fig. 95.8 ) that prevents drainage tube formation and locking. Finally, it may be difficult or impossible to place a PC tube in a perforated, decompressed gallbladder.

Percutaneous access to the gallbladder can be achieved via direct image guidance with ultrasound, fluoroscopy, or CT. The preferred method of ultrasound guidance is normally performed with a midrange frequency 2- to 8-Hz curvilinear array sector probe. The procedure may be performed at the bedside when necessary but catheter insertion is best performed in a fluoroscopy suite. CT/Cone beam CT fluoroscopic guidance is rarely necessary but can be helpful when a significantly diseased or calculous gallbladder limits sonographic visualization of the lumen. but may be helpful when a significantly diseased or calculous gallbladder limits sonographic visualization of the lumen. Standard sterile technique should always be used.
Local anesthesia and moderate sedation with subcutaneous lidocaine 2% and intravenous midazolam and fentanyl is sufficient for most patients, although critical care support is needed in critically ill patients. Intravenous antibiotics with Gram-negative coverage should be administered. Ideally these antibiotics are given 12 to 24 hours before the procedure.
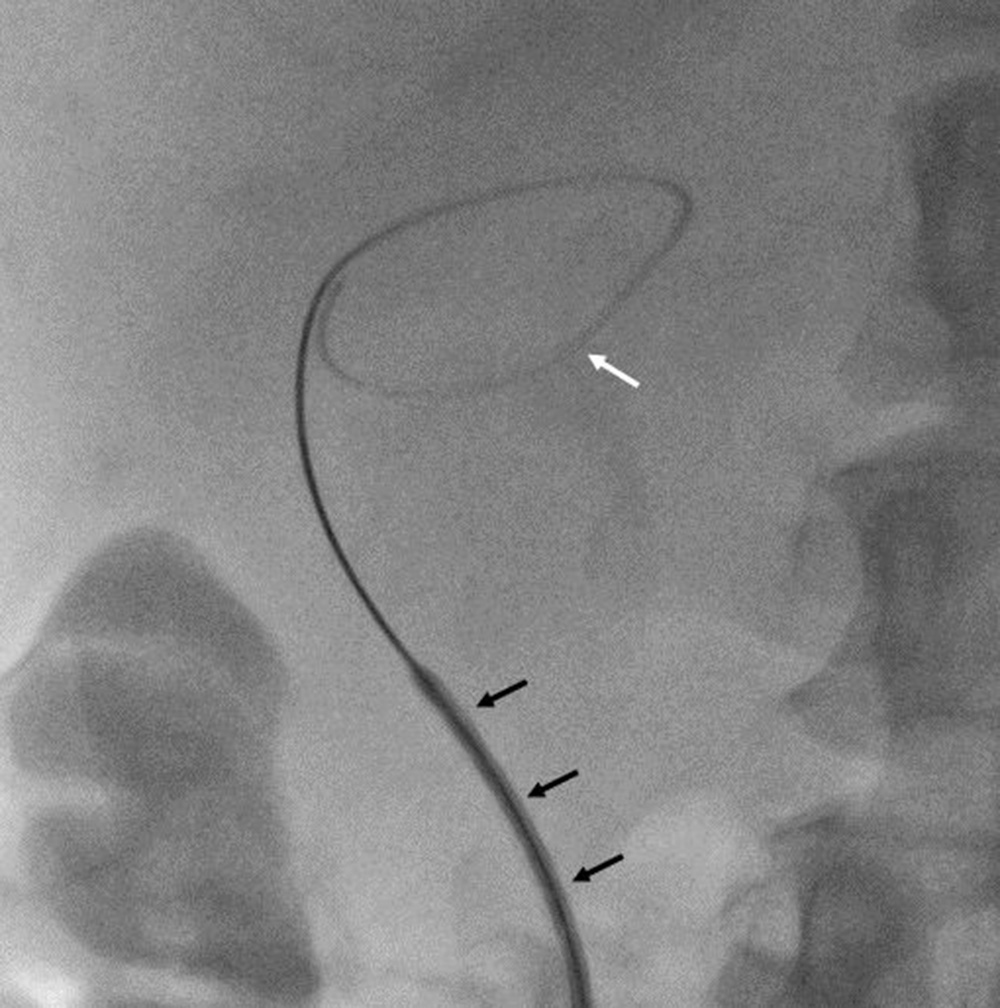
The gallbladder is usually accessed with an 18-gauge (G) percutaneous entry needle or trocar needle, with length dependent on the distance measured to the gallbladder. A 21-G micropuncture or 22-G Chiba needle with a 0.018-inch wire may be employed with a wire guide exchange set that allows transition to a 0.035-inch system; 8F and 10F tissue dilators are often required. Once accessed, the biliary system is opacified with iodinated contrast such as Omnipaque (Iohexol; GE Healthcare, Chicago, IL). A 0.035-inch Rosen (Cook Medical, Bloomington, IN) or short Amplatz Super Stiff wire (Boston Scientific, Natick, MA) have the necessary stiffness to support drainage tube placement and may also be partly looped within the gallbladder ( Fig. 95.9 ). A self-retaining all-purpose drain with distal side holes (e.g., Flexima [Boston Scientific]) is used for gravity drainage and connected to a bag. A variety of cholangioplasty balloons and snares and lithotripsy may be employed when gallstone extraction is contemplated. The gallbladder and biliary system may be directly visualized with a 15F choledochoscope, which will require an 18F tract.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here