Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Bronchiolitis is a general term used to describe inflammatory lung diseases primarily affecting the small conducting airways and often (but not always) sparing the more distal lung parenchyma. It may occur in isolation, but sometimes it may be a component of a disease involving proximal airways (bronchiectasis, asthma). Bronchiolitis occurs in a wide variety of clinical settings ( Table 21.1 ) and manifests varied histopathologic changes, resulting in an equally varied and sometimes confusing terminology. Diseases of small airways involve airways of 2 mm in diameter or less, roughly corresponding to ninth-generation airways. Their fundamental histopathologic feature is complete or partial luminal obstruction brought about by bronchiolar wall thickening and inflammation, intraluminal growth, or peribronchiolar fibrosis. This can translate into physiologic changes of obstruction, but not uncommonly, restrictive defects may accompany these changes or occur alone. Radiographic characteristics of bronchiolitis include bronchiolar wall thickening, bronchiolar dilatation, and luminal impaction due to either secretions or cellular or fibrotic intraluminal tissue. Impaction is manifested radiographically as 2- to 4-mm nodular or linear branching centrilobular opacities on computed tomography of the chest. It can produce a tree-in-bud radiographic pattern, which is regarded as typical of bronchiolitis, in which branching linear structures have more than one contiguous branching site, somewhat resembling the childhood toy “jacks.”
| Inhalational Injury | Postinfectious | Drug- or Chemical-Induced Reactions | Idiopathic |
|---|---|---|---|
| Toxic fume inhalation Grain dusts Irritant gases Mineral dusts Fumes (eg, welding) Cigarette smoke |
Viral:
Other infectious agents:
|
Hexamethonium L-Tryptophan Busulfan Free-base cocaine Gold Cephalosporin Sulfasalazine Amiodarone Acebutolol Sulindac Paraquat poisoning |
No associated diseases:
Associated with other diseases
|
By definition, bronchioles are airways that do not have cartilage in their walls. The membranous (or terminal) bronchioles serve purely an air conducting function ( Fig. 21.1 ), whereas the respiratory bronchioles, which bear alveoli, also participate in gas exchange. Diseases affecting small airways may originate intrinsically within the bronchioles or may result from extension of diseases that involve primarily the bronchi (bronchitis, bronchiectasis) or the lung parenchyma (bronchopneumonia). As noted, this group of diseases has a broad spectrum of etiologies that includes infectious and noninfectious agents such as bacteria, viruses, toxic fumes, and inhaled dusts. Some diseases of small airways are associated with connective tissue disorders, others result from drug usage, and others occur in the clinical setting of organ transplantation. Given the histologic overlap between the manifestations of this spectrum of conditions, it is sometimes difficult to determine a specific cause of the bronchiolitis in an individual case. Bronchiolitis may also represent one of several features of another pulmonary disorder, such as hypersensitivity pneumonia or respiratory bronchiolitis–interstitial lung disease (RB-ILD). In these conditions, bronchiolitis is a component of a disease that involves distal lung parenchyma.
Diseases of small airways have been classified according to etiology or clinical setting, and also by histopathology ( Tables 21.1 and 21.2 ). This chapter will discuss the major clinicopathologic entities classified as small-airway diseases.
| Primary bronchiolar disorders |
|
| Interstitial lung disease with a prominent bronchiolar involvement |
|
| Bronchiolar involvement in diseases also involving large airways |
|
Acute bronchiolar injury secondary to acute exposure to a variety of infectious and noninfectious agents
Common clinical syndrome, often treated symptomatically without need for biopsy
Worldwide distribution
Mortality is less than 1% overall
Immunocompromised patients with respiratory viral infections have a higher mortality, especially with adenovirus
Obliterative bronchiolitis is a potential consequence and is a cause of chronic respiratory dysfunction
Affects both genders
No specific racial predilection
Age distribution depends on particular cause
Symptoms include fever, tachypnea, dyspnea, prolonged expiration, wheezing
Etiologies include infectious agents (especially respiratory viruses, but also bacteria, Mycoplasma, Chlamydia, fungi, and mycobacteria) and inhaled toxic fumes and vapors
This injury pattern can also be seen in settings of asthma, aspiration, bronchiectasis, inflammatory bowel disease, and connective tissue disorders
Obstructive ventilatory defects can be observed
Variable changes, including centrilobular nodules, diffuse bilateral reticulonodular opacities, linear or ground-glass opacities, or patchy pneumonic consolidation
Hyperinflation is particularly common in children
Atelectasis can also be observed
The prognosis is variable, depending on the diffuseness and severity of the injury
Most patients have relatively mild symptoms and can be given supportive care, leading to full recovery
With more severe disease, supplemental oxygen, antimicrobial therapy, corticosteroids, or bronchodilators may be administered
Neutrophilic infiltration of the bronchiolar epithelium, with or without epithelial or mucosal necrosis, and fibrinous material in airway lumens
With time, luminal exudates resolve or organize
With respiratory syncytial virus infection, bronchiolar epithelial hyperplasia may be conspicuous
Viral changes may be present ( Chapter 13 )
Can be helpful for identification of specific respiratory viruses (respiratory syncytial virus, adenovirus, parainfluenza, influenza)
Spectrum of etiologies, including infectious agents and noninfectious etiologies
DPB
Obliterative bronchiolitis
The term acute bronchiolitis is commonly used clinically to describe an illness in infants and children characterized by acute wheezing and signs of respiratory infection. It can also be used histologically to refer to acute inflammatory and sometimes necrotizing injury to the bronchiolar epithelium. The bronchiolar epithelium is vulnerable to acute injury by infectious agents (especially respiratory viruses, but also bacteria, Mycoplasma, Chlamydia, fungi, and mycobacteria) and inhaled toxic fumes and vapors. Acute injury to the bronchioles can also be seen in settings of asthma, aspiration, bronchiectasis, inflammatory bowel disease, and connective tissue disorders. The clinical, radiographic, and pathologic features described here apply primarily to acute viral bronchiolitis, but overlap to some extent with acute bronchiolar injury due to bacterial infections or inhaled toxic substances.
Most patients present with an acute onset of fever, tachypnea, dyspnea, prolonged expiration, and wheezing. In infants, nasal flaring and chest retractions may be seen. Crackles are usually heard on auscultation. Adults and children can be affected, and age predilections depend on the specific etiologic agent. Infectious agents that cause acute bronchiolitis and its potential sequela, obliterative bronchiolitis, are discussed in more detail in other chapters. In brief, respiratory syncytial viruses (RSVs) are responsible for annual outbreaks of bronchiolitis and pneumonia, primarily in infants and young children. Adenovirus and parainfluenza viruses can also produce acute bronchiolitis in children and adults, but more commonly cause upper respiratory tract infections. Cases of acute bronchiolitis caused by M. pneumoniae, C. trachomatis, and C. pneumoniae have been described in adults and children. Toxic inhalational exposures occur primarily in the adult population.
Obstructive ventilatory defects can be observed.
Radiographic studies show variable changes, including centrilobular nodules, diffuse bilateral reticulonodular opacities, linear or ground-glass opacities, or patchy pneumonic consolidation. Hyperinflation is particularly common in children. Atelectasis can also be observed.
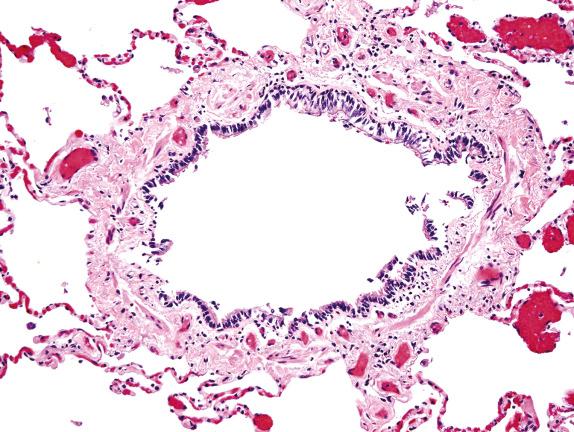
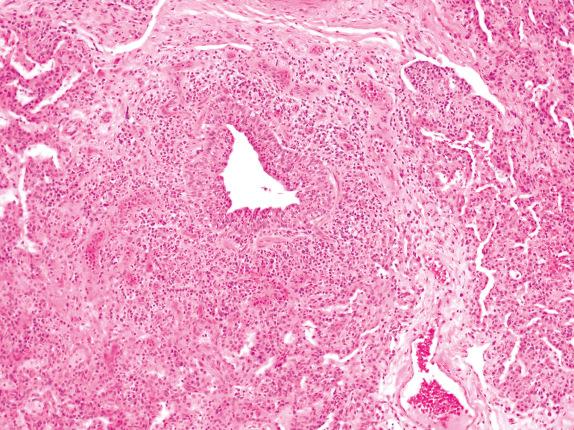
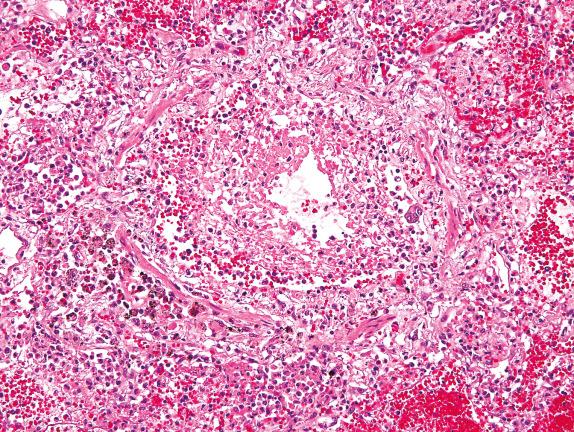
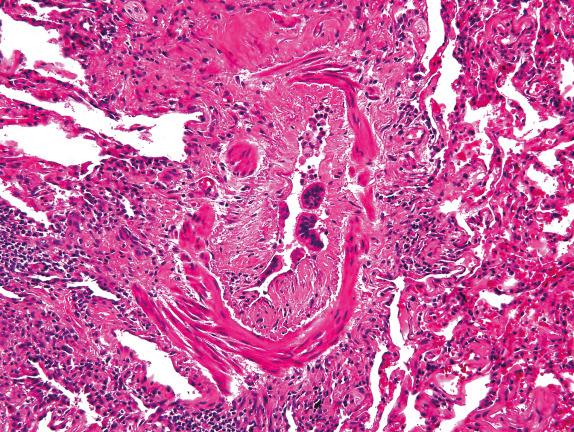
Pathologic features of acute infectious bronchiolitis are primarily those of an acute bronchiolitis, with neutrophilic infiltration of the bronchiolar epithelium and the surrounding peribronchiolar tissues ( Fig. 21.2 ). Epithelial or mucosal necrosis may be present ( Fig. 21.3 ), and neutrophils and fibrinous material can accumulate in the lumens of bronchioles and alveolar ducts. Similar changes can occur in bronchiolar injuries associated with toxic inhalations, although some examples may show lesser degrees of inflammatory cell infiltration and more hypocellular necrosis. In cases of RSV infection, this phase is often followed by a pronounced regenerative hyperplasia of the bronchiolar epithelium, in which the epithelium develops small papillary projections extending into the bronchiolar lumens ( Fig. 21.4 ). Over time, the mural or luminal exudates can resolve or become organized and fibrotic, producing luminal obstruction. In the latter case, the process is then referred to as bronchiolitis obliterans or obliterative bronchiolitis. At these later points, lymphocytes and plasma cells can be seen in the fibrous tissue, and complete or partial loss of the bronchiolar epithelium is common. Other secondary changes include inflammation of alveolar walls and the presence of foamy macrophages in the peribronchiolar alveoli (endogenous lipoid pneumonia).
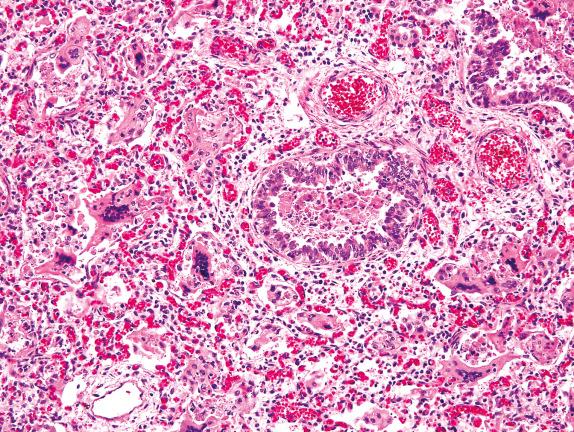
Acute bronchiolitis is often recognized from its clinical and radiographic features, and biopsy is usually not necessary. Biopsy is more commonly performed in severe or atypical cases, in patients where there is another indication to perform the biopsy, or in immunocompromised patients who may have multiple potential etiologies (with differing treatments) for their respiratory illnesses. For the most part, the histologic appearance does not point to a specific etiology, although there are exceptions. RSV and parainfluenza can produce multinucleated giant cells and intracytoplasmic inclusions ( Fig. 21.4 , also discussed in Chapter 13 ). “Smudge cells” and intranuclear inclusions may indicate adenovirus. Immunohistochemical staining for respiratory viruses can be helpful, as can cultures; immunofluorescence staining; or molecular, serologic, or antigenic testing. Patient age and history are also important for defining more likely etiologic agents.
The differential diagnosis may also include diffuse panbronchiolitis (DPB), which can include a component of acute inflammation, but also shows characteristic centrilobular accumulations of foamy macrophages in interstitial regions and airspaces. Constrictive bronchiolitis (CB) may also show acute inflammatory infiltrates in bronchiolar mucosae, but will feature dense, mature collagenous thickening of the bronchiolar wall, which will not be observed in acute bronchiolitis.
The prognosis is variable, depending on the etiology and the diffuseness and severity of the injury. Most patients have relatively mild symptoms and can be given supportive care. With more severe disease, supplemental oxygen, antimicrobial therapy, corticosteroids, or bronchodilators may be administered. Overall, the mortality rate is less than 1%, but mortality associated with the respiratory viral infections appears to be higher with immunocompromise. Evolution of acute bronchiolitis into obliterative bronchiolitis occurs in some patients, particularly after adenovirus infection and after some toxic inhalations.
A bronchiolar disease characterized clinically by chronic cough and dyspnea, functionally by limitation of air flow, and histopathologically by mural and peribronchiolar fibrosis
The actual incidence is not known, but CB is more prevalent in the setting of organ transplantation, exposure to toxic agents, connective tissue disorders, and after viral infections
Worldwide distribution
High mortality rate
Most important cause of mortality in long-term survivors of lung transplantation
Frequently complicated by superimposed infections
Affects adults and children of both genders
No evident racial predilection
Symptoms include chronic cough and dyspnea
CB occurs in a variety of clinical settings:
As a complication of lung transplantation, in which it represents chronic airway rejection
After bone marrow transplantation, where it usually represents a manifestation of graft-versus-host disease
After exposure to inhaled toxic agents such as nitrogen dioxide, sulfur dioxide, ammonia, chlorine, and phosgene
With usage of some drugs such as gold, penicillamine, and lomustine
As a sequela to infections with adenovirus and other respiratory viruses
In the setting of systemic disorders such as rheumatoid arthritis, systemic sclerosis, ulcerative colitis, and ankylosing spondylitis
In association with consumption of the tea leaves of S. androgynous (an appetite suppressant)
Microwave popcorn workers exposed to diacetyl
Some cases of CB are idiopathic
Progressive airway obstruction, with lack of response to bronchodilators
Chest images may be normal or show hyperinflation, peripheral attenuation of vascular markings, and sometimes nodular or reticulonodular opacities
The course of CB is progressive, and its prognosis is poor
Numerous treatments have been attempted with little success, and lung transplantation may represent the only option
New immunomodulatory agents are under investigation and may offer benefit to some patients with this disorder
Bronchioles have thickened fibrotic hypocellular walls with concurrent luminal narrowing; complete replacement of the lumen by mature collagen may occur
The mature collagen is often circumferential in distribution, but not always so; it may replace some or all of the bronchiolar smooth muscle and extend out into peribronchiolar tissues
The bronchiolar epithelium may have a reactive or attenuated appearance, with squamous metaplasia, or resemble type II pneumocytes
Trichrome and elastic van Gieson stains are helpful for assisting in the identification of obliterated bronchioles by highlighting their muscle coats (trichrome stain) or the bronchiolar elastica (elastic van Gieson), as well as for enhancing the visibility of the fibrous tissue
Most cases show a predominance of T-cells, with fewer B-cells
Although there are numerous antecedents to CB, the specific cause of an individual case cannot usually be determined histologically
Organizing pneumonia with fibrosis
CB, also known as bronchiolitis obliterans or obliterative bronchiolitis, is characterized clinically by chronic cough, dyspnea, limitation of airflow, and lack of response to bronchodilators and prednisone. Its main histopathologic features are irreversible mural and luminal fibrotic scarring of bronchioles with narrowing or obliteration of the airway lumens. CB occurs in a variety of clinical settings, often as a complication of lung or bone marrow transplantation; after exposure to inhaled toxic agents such as nitrogen dioxide, sulfur dioxide, ammonia, chlorine, and phosgene; with use of some drugs such as gold, penicillamine, and lomustine; as a sequela to infections with adenovirus and other respiratory viruses; and in the setting of systemic disorders such as rheumatoid arthritis, systemic sclerosis, ulcerative colitis, and ankylosing spondylitis. In the Far East, an outbreak of CB occurring in association with consumption of tea leaves of Sauropus androgynous (as an appetite suppressant) has been reported. Another rare syndrome, Swyer-James syndrome (also known as MacLeod syndrome ) is characterized by CB in association with recurrent pulmonary infections, decreased exercise tolerance, and unilateral hyperlucency on chest radiographs. More recently, a microwave popcorn production facility, where workers were exposed to diacetyl, reported increased mortality from CB. Finally, some cases of CB are idiopathic.
The pathogenesis of this process is not well understood. Streichenberger and colleagues studied the complex interaction between lysyl oxidase (LOX), the main collagen-cross-linking enzyme, and protein matrix components (tenascin, fibronectin) of the extracellular matrix and identified three stages of the disease (inflammatory, fibroinflammatory, and fibrotic), suggesting that persistence of LOX might account for the irreversibility of the fibrotic process in the later stages of the disease. In the transplant literature, there is information about the roles of lymphocytes and fibroblasts, as well as a variety of mediators (growth factors, adhesion molecules, oxidants, and others) in the genesis of this process.
Obstructive ventilatory defects are observed, without significant response to bronchodilators. In the setting of lung transplantation, progressive airway obstruction is characterized by decreasing FEV 1 (bronchiolitis obliterans syndrome).
Chest radiographs may be normal or show nonspecific changes such as hyperinflation, peripheral attenuation of vascular margins, and sometimes nodular or reticulonodular opacities. Bronchial wall thickening and bronchiectasis can occasionally be seen.
Typically, bronchioles in CB have thickened fibrotic hypocellular walls with concurrent luminal narrowing ( Fig. 21.5 ). The mature collagen is often circumferential in distribution, but not always so. In the fibrotic walls, a variably dense mononuclear inflammatory infiltrate including lymphocytes (usually predominantly T-cells, with fewer B-cells) and plasma cells may be seen. The dense collagen may replace some or all of the bronchiolar smooth muscle and extend out into peribronchiolar tissues. As the fibrosis progresses, the lumen can eventually become obliterated ( Fig. 21.6 ). The bronchiolar respiratory epithelium may have a reactive or attenuated appearance, with squamous metaplasia, or resemble type II pneumocytes.
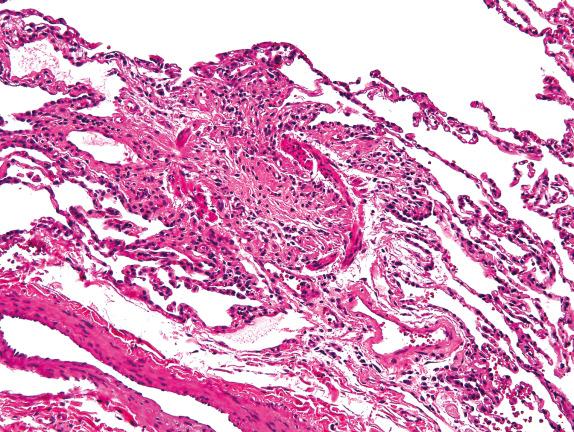
Trichrome stains are helpful for assisting in the identification of obliterated bronchioles by highlighting their muscle coats when their lumens have been replaced by fibrotic scars and by clarifying the presence and degree of fibrosis. A Verhoeff–van Gieson elastic stain is also helpful for identifying the obstructed airways by highlighting the elastic layer of the obliterated bronchioles. Another clue to the diagnosis lies in finding a small pulmonary artery branch that is unpaired with a bronchiole. Because the pulmonary arteries and the airways travel together, the absence of a bronchiole adjacent to a small artery should prompt consideration of obliterative bronchiolitis as a diagnostic possibility. In these cases a trichrome stain can be very helpful (it will show smooth muscle fibers that were a portion of the bronchiole).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here