Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Absorption of topical medications depends upon several factors, including cutaneous barrier function, the anatomic site, the active agent, and characteristics of the vehicle
In neonates, there is a greater risk of systemic toxicity with use of topical medications
Combination or rotational therapy using topical agents may result in increased efficacy and decreased risk of side effects
Topical medications are fundamental in the armamentarium of dermatologic therapeutics, offering the ability to deliver treatment directly to the skin while limiting systemic side effects. However, topical therapy can be time-consuming and messy, and it may not be practical for generalized skin disorders or effective for conditions with deeper involvement. Choosing an appropriate topical regimen requires consideration of the disease process and involved site(s) as well as the vehicle, application strategy, and duration of use of the selected agent. This chapter reviews general principles of topical therapy and topical medications not discussed elsewhere in the textbook. Table 129.1 lists topical medications covered in other chapters.
| TOPICAL MEDICATIONS DISCUSSED IN OTHER CHAPTERS | |
|---|---|
| Topical medications | Chapter(s) |
| Chapters on medical therapy or cosmetics | |
| Glucocorticoids | 125 |
| Retinoids | 126 |
| Antimicrobials (antibacterials, antifungals, antivirals) | 127 |
| Sunscreens | 132 |
| Anesthetics | 143 |
| Cosmeceuticals | 153 |
| Chemical peel agents | 154 |
| Other chapters | |
| Topical crisaborole for atopic dermatitis | 12 |
| Brimonidine and oxymetazoline for facial erythema in rosacea | 37 |
| Aluminum chloride for hyperhidrosis | 39 |
| Topical immunotherapy for alopecia areata (with squaric acid dibutyl ester or diphencyprone) | 69 |
| Sinecatechins for anogenital warts | 79 |
| Antiparasitic agents (including treatments for infestations) | 83, 84 |
| Insect repellents | 85 |
| Topical β-blockers (e.g. timolol) for infantile hemangiomas | 103 |
| Wound healing agents | 105, 141 |
| Hemostatic agents | 151 |
Topical formulations consist of an active ingredient in a non-active base (vehicle). To be effective, topical medications must gain entry into the skin and reach the desired target site, e.g. the epidermis below the stratum corneum or the dermis, in adequate concentrations. Successful topical therapy therefore requires percutaneous absorption, which depends upon factors related to the skin being treated as well as the agent and its vehicle ( Table 129.2 ). The role of the stratum corneum in skin barrier function, including percutaneous absorption of medications, is discussed in Chapter 124 .
| FACTORS THAT AFFECT PERCUTANEOUS ABSORPTION |
| Characteristics of the patient/skin |
|
| Properties of the medication/its application |
|
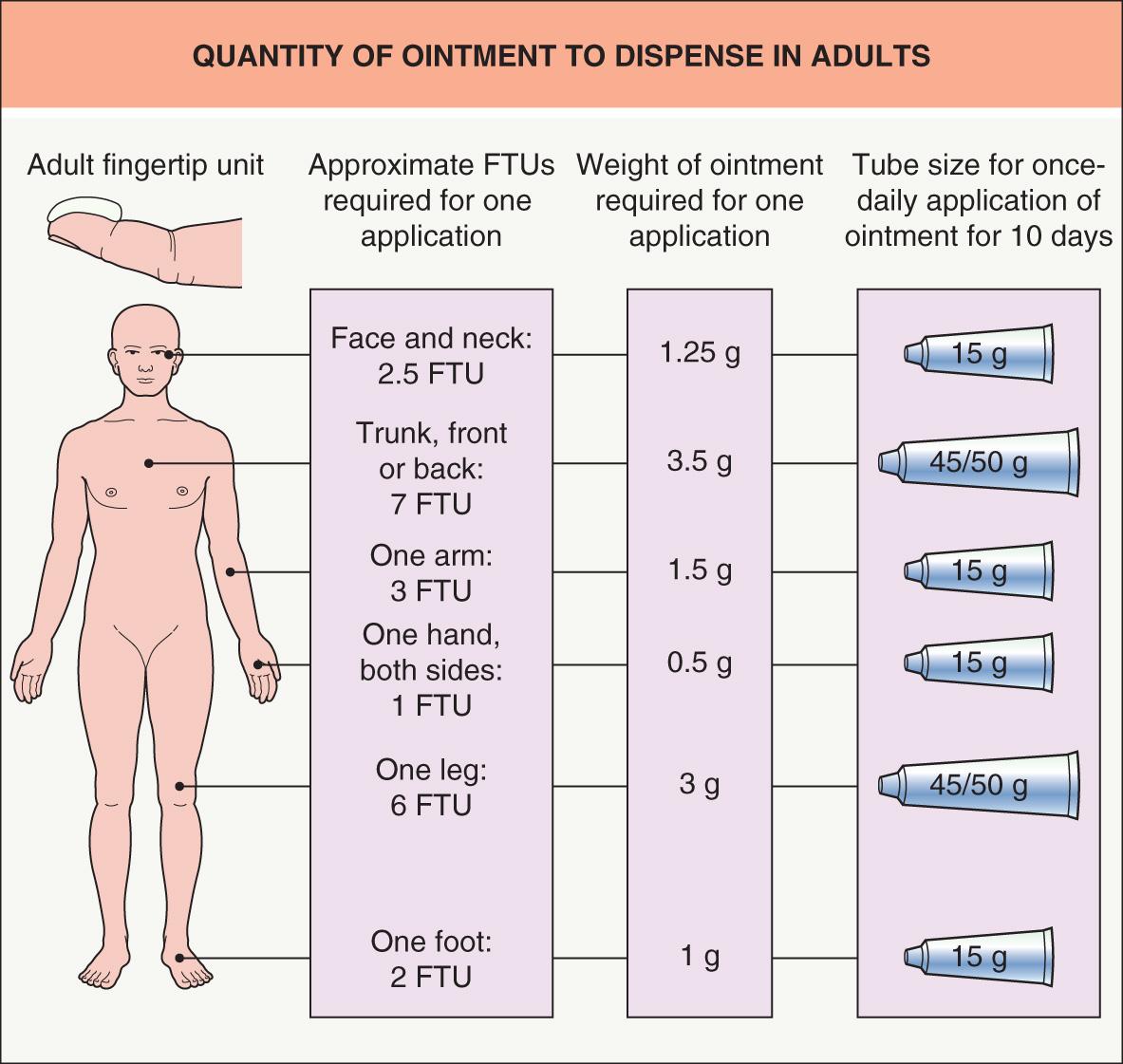
In general, topical medications should be applied to the skin as a thin layer. A thicker layer of medication does not result in enhanced penetration or additional therapeutic benefit. One gram of cream covers a ~10 cm × 10 cm area of skin, and the same amount of ointment spreads nearly 10% further.
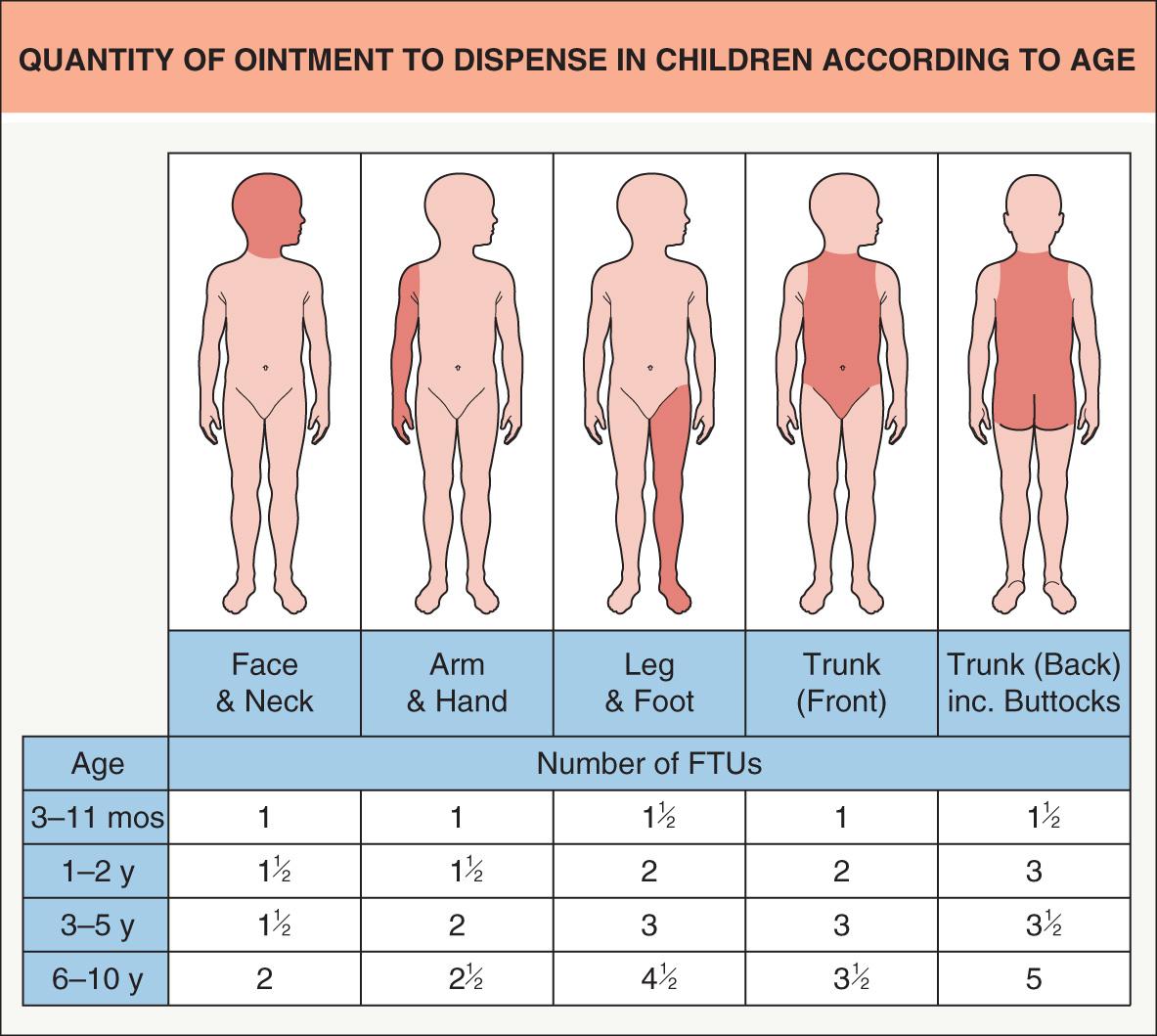
A practical guide to quantifying the amount of ointment necessary to treat different areas of the body is the “fingertip unit” (FTU), which represents the amount of ointment dispensed from a 5 mm-diameter nozzle that extends from the distal crease to the tip of the index finger in an adult . One FTU is equal to ~0.5 g, and the quantities required to treat various areas of the body in adults and children are presented in Figs 129.1 and 129.2 . The appropriate amount to treat the entire body of an adult man is ~20 g, therefore requiring ~250 g per week if applied twice daily. Because ~0.5 FTU (0.25 g) can treat an area equivalent to one side of an extended (“flat”) hand, estimating the number of “flat hand areas” of affected skin assists in determining the amount of medication needed. For example, four “flat hand areas” would require 1 g per application and ~15 g per week if applied twice daily.
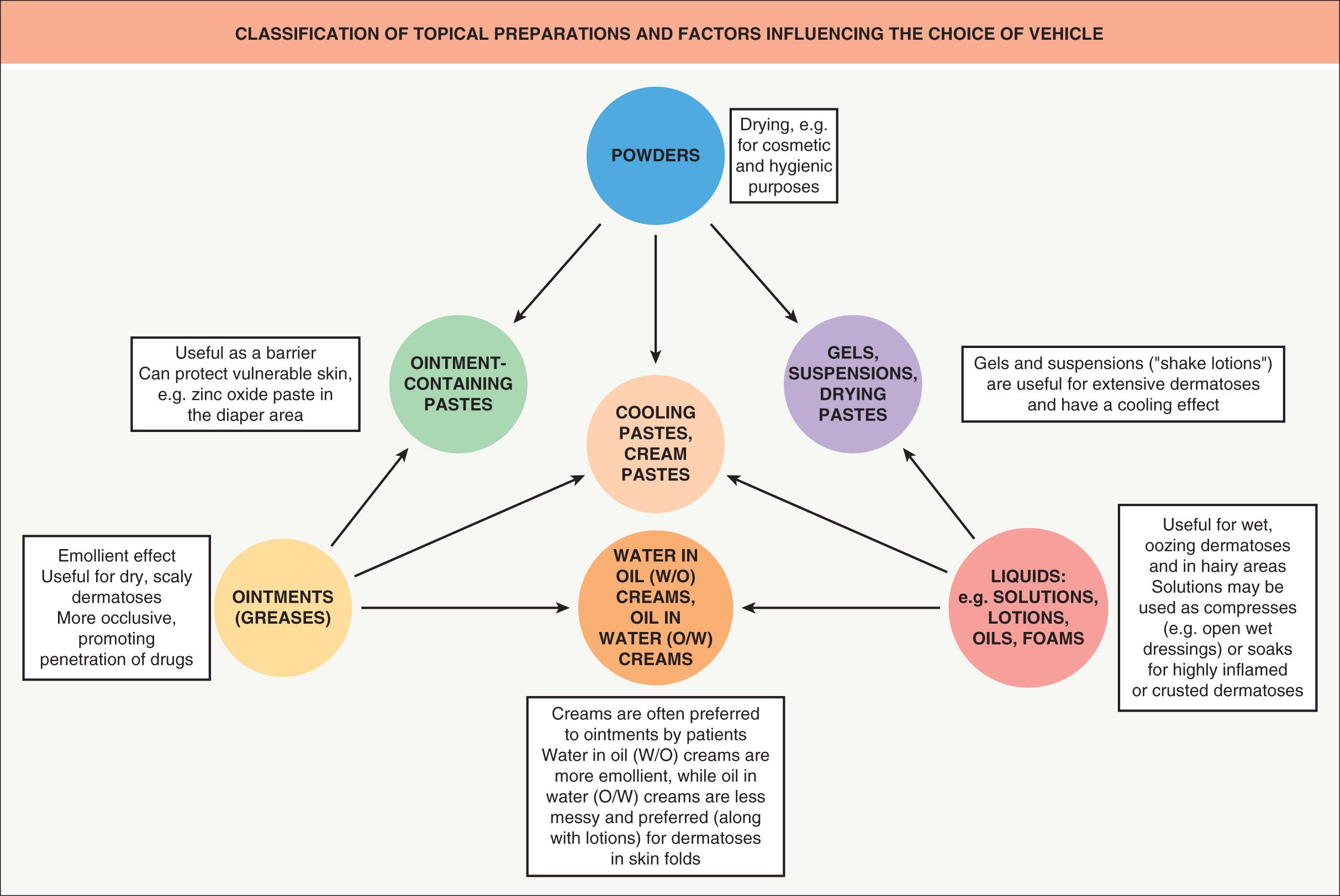
A classification of topical formulations and clinical guidelines for vehicle selection are presented in Fig. 129.3 . A discussion of how vehicles affect drug delivery is found in Chapter 124 .
The decision to use topical medications during pregnancy and lactation should be based on the potential risk of the medication and the extent to which the condition affects the health of the woman. Use of the following topical medications during pregnancy (not a comprehensive list) is generally contraindicated: podophyllin, anthralin, lindane, chemotherapeutics (e.g. carmustine, mechlorethamine hydrochloride [nitrogen mustard], 5-fluorouracil), tazarotene, and peels with phenol or salicylic acid. Table 129.3 presents the traditional US Food and Drug Administration (FDA) pregnancy risk categories and information on the new labeling system that was implemented in 2015. Table 129.4 lists topical medications with minimal risk during pregnancy and lactation.
| TRADITIONAL FDA CLASSIFICATION SYSTEM OF PHARMACEUTICAL PREGNANCY CATEGORIES | |
|---|---|
| Category | Description |
| A | Controlled studies show no risk. Adequate well-controlled studies in pregnant women have failed to demonstrate risk to the fetus. |
| B | No evidence of risk in humans. Either animal studies show risk, but human studies do not; or, if no adequate human studies have been done, animal findings are negative. |
| C | Risk cannot be ruled out. Human studies are lacking, and animal studies are either positive for fetal risk or lacking as well. However, potential benefits may justify the potential risk. |
| D | Positive evidence for risk. Human studies, or investigational or post-marketing data, show risk to fetus. Nevertheless, potential benefits may outweigh potential risk. |
| X | Contraindicated in pregnancy. Studies in animals or humans, or investigational or post-marketing reports, have shown fetal risk, which clearly outweighs any possible benefit to the patient. |
| TOPICAL MEDICATIONS WITH MINIMAL RISK DURING PREGNANCY AND LACTATION | |
|---|---|
| Pregnancy | Lactation |
| Azelaic acid | Acyclovir |
| Ciclopirox | Bacitracin |
| Clindamycin | Benzoyl peroxide |
| Clotrimazole | Butoconazole |
| Erythromycin | Calcipotriene |
| Metronidazole * | Ciclopirox |
| Mupirocin | Clotrimazole |
| Naftifine | Erythromycin |
| Nystatin † | Hydroquinone |
| Oxiconazole | Ketoconazole |
| Permethrin | Metronidazole |
| Retapamulin | Mupirocin |
| Terbinafine | Nystatin |
| Oxiconazole | |
| Terbinafine | |
| Tretinoin | |
* The CDC no longer recommends avoidance of oral metronidazole during the first trimester.
† Intravaginal topical application not advised close to term because of risk of contamination if membranes have ruptured; pregnancy category A for pastilles.
Although the stratum corneum provides competent skin barrier function in full-term newborns under basal conditions (see Ch. 2 ), it undergoes structural and functional maturation during the first few weeks to months of life. Several factors result in an increased risk of systemic toxicity from topically applied medications during the neonatal period (the first 30 days of life) ( Table 129.5 ). Systemic toxicity has been reported in neonates exposed to topical corticosteroids, salicylic acid, lindane, hexachlorophene, chlorhexidine, and propylene glycol ( Table 129.6 ).
| FACTORS THAT INCREASE THE RISK OF SYSTEMIC TOXICITY FROM TOPICAL MEDICATIONS IN NEONATES |
|
| POTENTIAL SYSTEMIC SIDE EFFECTS OF TOPICAL MEDICATIONS | |
|---|---|
| Medication | Systemic side effect |
| Androgens | Virilization in women, children * , and fetuses |
| Boric acid | Generalized erythema, fever, vomiting, mental status change |
| Calcipotriene (calcipotriol) | Hypercalcemia, hypercalciuria |
| Carmustine (BCNU) | Bone marrow suppression |
| Chlorhexidine | Nausea, signs of ethanol intoxication |
| Clindamycin | Diarrhea, pseudomembranous colitis (controversial) |
| Corticosteroids | Iatrogenic Cushing syndrome, inhibition of hypothalamic–pituitary axis |
| Dimethylsulfoxide | Nausea, abdominal pain |
| Epinephrine (adrenaline) | Tachycardia |
| Estrogens | Pseudoprecocious puberty, gynecomastia, hypogonadism in men |
| Gentamicin | Ototoxicity |
| Hexachlorophene | Neurotoxicity, coma, death |
| Iodine | Hypothyroidism |
| Lidocaine and other topical anesthetics | With overdose (>5 mg/kg of lidocaine absorbed): early/lower levels – paresthesias (e.g. perioral tingling), tinnitus, dysgeusia (e.g. metallic taste), lightheadedness, tremors; late/higher levels – seizures, hypotension, arrhythmias, cardiopulmonary arrest (see Ch. 143 ) |
| Lindane | CNS toxicity |
| Malathion | CNS toxicity, hyperglycemia |
| Mechlorethamine (nitrogen mustard) | Myelosuppression |
| Mercury | CNS and renal toxicity, acrodynia |
| Minoxidil | Cardiac toxicity |
| Neomycin | Ototoxicity, nephrotoxicity |
| Phenol | Cardiac arrhythmia, death |
| Podophyllin | Gastrointestinal (nausea, vomiting), neurologic (mental status changes, peripheral polyneuropathy) and hematologic (thrombocytopenia, leukopenia) effects |
| Prilocaine–lidocaine (EMLA®) | Methemoglobinemia (perioral/acral cyanosis, vascular “mottling”) related to prilocaine; see lidocaine above |
| Propylene glycol | Hyperosmolality, with or without lactic acidosis |
| Salicylic acid | Tinnitus (early sign), gastrointestinal symptoms (e.g. nausea, vomiting), CNS toxicity (e.g. confusion, delirium, seizures), metabolic acidosis with respiratory compensation (i.e. tachypnea), hypoglycemia, coma, death |
| Silver (silver nitrate, silver sulfadiazine) | Leukopenia, argyria |
* May occur from passive transfer of paternal topical testosterone.
The advantages of using a single topical agent include improved compliance and often lower cost. However, combination or rotational therapy is sometimes employed to provide additive/synergistic effects via different mechanisms of action or to decrease potential side effects by reducing exposure to one or both agents, especially if they have different adverse-effect profiles. Examples of this strategy for topical therapy include various combinations of benzoyl peroxide, retinoids, and antibiotics to treat acne; use of a corticosteroid together with a vitamin D analogue or tazarotene to treat psoriasis; and rotating use of a corticosteroid and calcineurin inhibitor to treat atopic dermatitis.
Pruritus involves multiple components of the nervous system, including skin surface receptors, peripheral (especially unmyelinated C fibers) and central nerves, and specific brain regions (see Ch. 5 ). Treatment of the associated dermatologic condition, e.g. with application of topical corticosteroids to inflamed skin and lubrication of dry skin, or underlying systemic cause remains the most effective method of alleviating itch. Topical antipruritic agents may help reduce the urge to scratch, potentially improving the efficacy of skin disease-specific therapies. Mechanisms of action of topical antipruritics include substituting a different sensation for itching, anesthetizing cutaneous nerve endings, and blocking molecular mediators of pruritus . Unfortunately, a relative lack of comparative studies has made antipruritics difficult to evaluate. Commonly used agents are outlined in Table 129.7 (also see Table 5.5 ).
| TOPICAL AGENTS USED TO ALLEVIATE PRURITUS | |||
|---|---|---|---|
| Agent | Classification/derivation | Mechanism of action | Uses and side effects |
| Pramoxine 1% (gel, lotion); in combination with 0.5–2.5% hydrocortisone in lotion, cream, ointment, or foam | Ester anesthetic | Blocks transmission of sensory nerve impulses; hypoalgesic effect on cold pain, but not heat pain; duration of effect is 2–4 hours |
|
| Menthol (up to 16% in a variety of lotions, creams, ointments, and gels) | Cyclic terpene alcohol derived from plants in the Mentha genus | Activates TRPM8 cation channels, which also respond to cold thermal stimuli; possible central itch modulation via Aδ fiber and/or κ-opioid receptor activation |
|
| Phenol | Originally a distillation product of coal tar | Thought to act directly on cold receptors |
|
| Camphor (0.25–0.5%; various preparations) | Ketone originally derived from the camphor laurel tree ( Cinnamomum camphora ) | Local anesthetic effect |
|
| Capsaicin (0.025–0.075% cream, lotion, gel or stick; 8% patch) | Natural alkaloid; derived from Solanaceae family members, including hot chili peppers of the Capsicum genus | Activates the TRPV1 vanilloid receptor, which also responds to temperatures >43°C (109°F); repeated release of substance P from C neurons eventually leads to depletion of this neuropeptide (and reduced transmission of heat, pain and itch) |
|
| Doxepin 5% cream | Tricyclic compound | Potent histamine antagonist (H 1 and H 2 ); sedation via anticholinergic properties |
|
| Diphenhydramine (2% cream, lotion, gel or spray) | Antihistamine | H 1 histamine antagonist; localized anesthetic effect via blockage of sodium channels |
|
Keratolytic agents reduce the thickness of the stratum corneum via elimination of squames. This can be beneficial in diseases characterized by reduced desquamation or accelerated epidermal proliferation. Keratolytics and humectants are reviewed in Table 129.8 , and their use in cosmeceutical products and chemical peels is discussed in Chapters 153 and 154 .
| TOPICAL KERATOLYTICS AND HUMECTANTS | ||||
|---|---|---|---|---|
| Agent | Dosage | Mechanism of action | Indications | Side effects (pregnancy category) |
| Keratolytics | ||||
| Salicylic acid (2-hydroxybenzoic acid) | 0.5%–40% lotion, ointment, gel, foam, solution, shampoo, cleanser, pad, plaster; OTC or prescription | Alters corneocyte adhesion, likely via disruption of desmosomal proteins; possible mild anti-inflammatory effects | 0.5–2%: comedolytic for acne 2–10%: hyperkeratotic dermatoses 10–40%: corns, calluses, verrucae, focal hyperkeratosis; increases penetration of other topical agents 20–30%: chemical peels |
Irritation, burning, peeling, erosions (depending on the site and concentration); allergic contact dermatitis (uncommon); systemic absorption from extensive application, especially in neonates/infants, can lead to salicylism (see Table 129.6 ) (C) |
| α-hydroxy acids: glycolic, lactic > mandelic, tartaric, malic, and citric acids | Various concentrations and pH levels; cleanser, shampoo, lotion, cream, gel, solution, mask | Diminish strength of intercellular bonding, thereby weakening corneocyte cohesion and leading to exfoliation; act at lower, newly forming levels of the stratum corneum; higher concentrations may have dermal effects (e.g. thickening) | Xerosis, ichthyoses, other hyperkeratotic dermatoses, acne, rosacea, photoaging; chemical peels | Irritation and burning, especially when applied to inflamed or eroded/fissured skin |
| Humectants | ||||
| Propylene glycol | 10–70% * solution or gel | Humectant, occlusive, and keratolytic agent * | Ichthyoses, keratodermas, other hyperkeratotic dermatoses | Irritation, burning |
| Urea | 10–50% cream, lotion, solution, gel, or foam; OTC or prescription (higher concentrations) | Due to its hygroscopic properties; absorption of water into the stratum corneum results in increased hydration, desquamation of corneocytes, enhanced barrier function, and decreased sensitizing effects of topical irritants | Xerosis, hyperkeratotic dermatoses (e.g. keratoderma climactericum, ichthyosis, psoriasis), nail avulsion; increases penetration of other topical medications | Irritation and burning, especially when applied to inflamed or eroded/fissured skin (B) |
* Often employed at lower concentrations as a preservative and penetration enhancer in vehicles.
Hydroquinone (1,4-dihydroxybenzene) is used to treat melasma and other disorders of hyperpigmentation (see Ch. 67 ) . In the US, 2% formulations are available over the counter, while 3% solution and 4% cream or gel require a prescription. Although twice-daily application is commonly recommended, irritant contact dermatitis can limit frequency of application. Some products contain hydroquinone combined with a sunscreen or with tretinoin (0.05–0.1%) and a class 5–7 corticosteroid .
Hydroquinone reduces skin pigmentation by competing with tyrosine as a substrate for tyrosinase (the initial enzyme in melanin biosynthesis; see Ch. 65 ) and via selective damage to melanosomes and melanocytes via production of reactive oxygen radicals .
Irritant or (less often) allergic contact dermatitis can develop. Exogenous ochronosis occasionally occurs with prolonged use of higher concentrations of hydroquinone. A variety of neoplasms have been noted to develop in rodents that received large systemic doses of the medication, but the relevance to topical therapy in humans has not been determined . Concern regarding potential adverse effects related to misuse of hydroquinone led to its removal from Japanese and European markets.
Hydroquinone is pregnancy category C.
Monobenzyl ether of hydroquinone (MBEH) 20% is infrequently used to depigment remaining normal skin in patients with extensive vitiligo in order to achieve a uniform appearance (see Ch. 66 ). It is thought to act via competitive inhibition of tyrosinase and free radical-mediated damage of melanocytes. Depigmentation is typically long-lasting, but repigmentation (especially in a perifollicular distribution) can occur following sun exposure. Both irritant and allergic contact dermatitis are possible side effects .
Mequinol (4-hydroxyanisole) is a skin-lightening agent. A solution composed of mequinol 2% and tretinoin 0.01% is FDA-approved for treatment of solar lentigines (pregnancy category X). However, the latter product is no longer commercially available in the US. Mequinol is a substrate of tyrosinase and may serve as a competitive inhibitor of melanin biosynthesis .
Both unwanted excessive hair and hair loss are common dermatologic complaints. Minoxidil, bimatoprost, and eflornithine are reviewed here, and a protocol for topical immunotherapy with diphencyprone (DPCP) or squaric acid dibutyl ester (SADBE) for alopecia areata is presented in Table 69.7 . The use of anthralin for alopecia areata is discussed below.
Originally developed as an antihypertensive agent, minoxidil has been known for decades to promote hair growth. Available in 2% and 5% solutions and a 5% foam, topical minoxidil is FDA-approved for the treatment of androgenetic alopecia in both men and women (see Ch. 69 ). It is also used for other forms of hair loss, including alopecia areata. Minoxidil is typically applied twice daily to the scalp .
Minoxidil causes premature termination of the telogen phase, lengthens the anagen phase, and can increase follicle size, particularly of miniaturized follicles . Stimulation of vascular endothelial growth factor and prostaglandin synthesis may also play a role . Although oral minoxidil relaxes vascular smooth muscle by opening ATP-dependent potassium channels, this mechanism has not been definitively linked to stimulation of hair growth .
While generally well-tolerated, topical minoxidil can cause dryness, irritation, and (uncommonly) allergic contact dermatitis; components of the solution formulation, in particular propylene glycol, may be responsible for these side effects. Topical minoxidil can also lead to unwanted hair growth at adjacent sites inadvertently exposed to medication (e.g. the face or ears). Systemic side effects such as headache and peripheral edema are occasionally observed.
Minoxidil is pregnancy category C.
Bimatoprost is a synthetic prostaglandin F 2α analogue that was initially utilized for the treatment of glaucoma. Following observations of thickening and elongation of the eyelashes in glaucoma patients treated with bimatoprost 0.03% ophthalmic solution ( Fig. 129.4 ), this agent was explored as a treatment for eyelash hypotrichosis and, in 2008, FDA-approved for this indication. When bimatoprost is applied nightly to the skin of the upper eyelid margin, increased eyelash length, fullness, and darkness are noted within 16 weeks in ~75% of patients ; upon discontinuation of treatment, return toward baseline typically begins within 4 weeks.

Bimatoprost was also found to improve eyebrow hypotrichosis in a randomized, vehicle controlled trial . There is ongoing study of its potential utility for various forms of scalp alopecia (e.g. androgenetic).
In animal studies, bimatoprost and other prostaglandin F 2α analogues (e.g. latanoprost) prolonged the anagen phase, increased the proportion of anagen follicles, and enlarged the dermal papilla and hair bulb during early anagen .
Bimatoprost ophthalmic solution can cause pruritus and irritation of the eye, conjunctival hyperemia, and hyperpigmentation of the eyelid skin and iris, with the latter likely to be permanent . Decreased intraocular pressure may occur but is generally not of clinical significance.
Bimatoprost ophthalmic solution is pregnancy category C.
Eflornithine 13.9% cream is indicated for the treatment of excessive and unwanted facial hair in women. It irreversibly inhibits ornithine decarboxylase in the skin, leading to decreased polyamine synthesis and arrest of follicular matrix cell proliferation . Twice-daily application for 24 weeks has been shown to significantly decrease facial hair , and use of eflornithine together with laser hair removal may result in more rapid and complete reduction in facial hair than laser treatment alone . Eflornithine is usually well tolerated, with occasional burning or acneiform eruptions at sites of application . Available by prescription in the US, it is pregnancy category C.
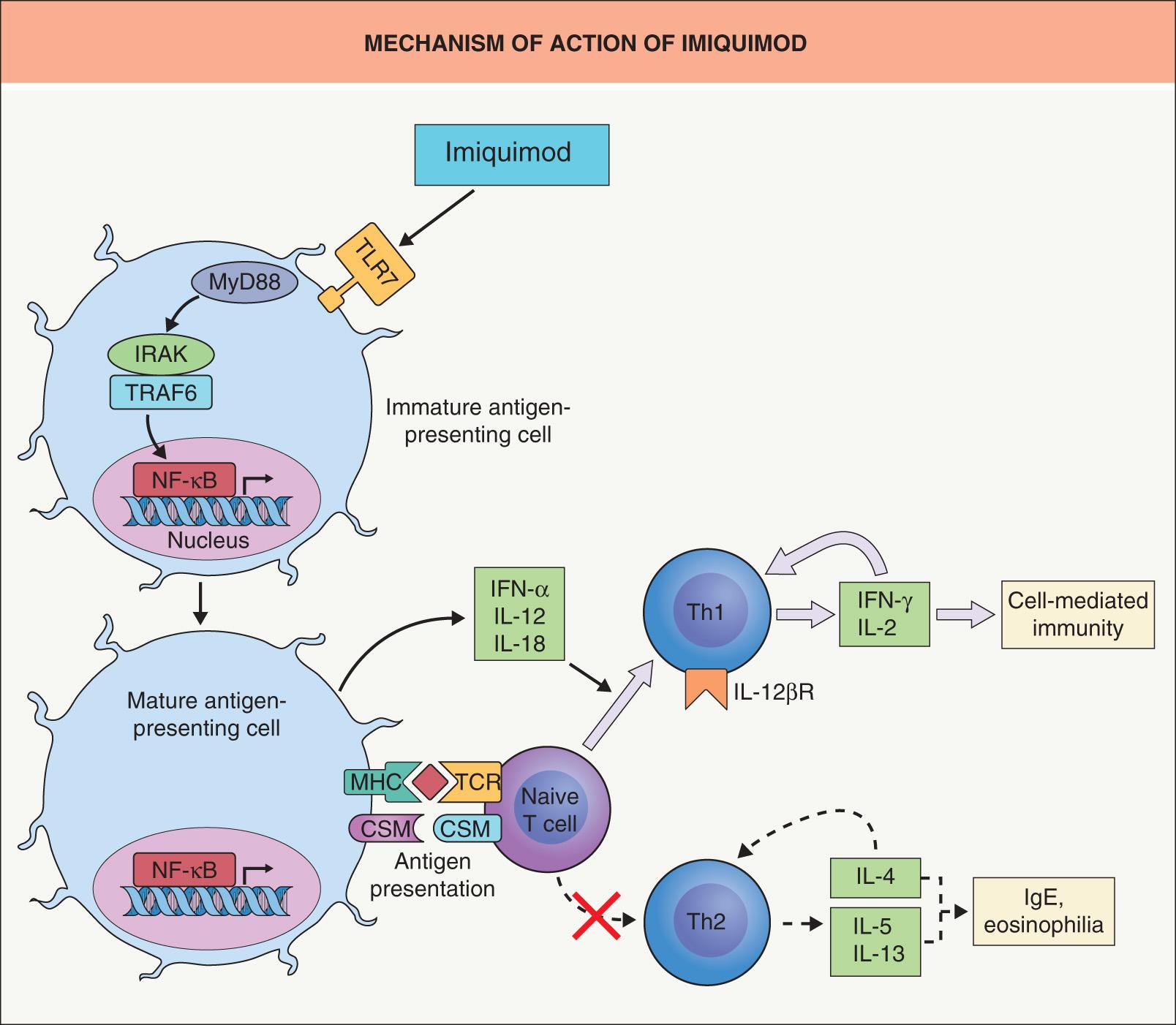
Imiquimod stimulates innate and adaptive immune response pathways, resulting in antiviral, antitumor, and immunoregulatory properties. Commercially available as 2.5%, 3.75%, and 5% creams, it is FDA-approved for the treatment of: (1) anogenital warts ; (2) actinic keratoses (AKs) on the face or scalp ; and (3) superficial basal cell carcinoma (BCC) measuring up to 2 cm in diameter on the trunk, neck, or extremities (excluding the hands and feet) . Off-label cutaneous uses with variable efficacy include treatment of common warts , Bowen disease (squamous cell carcinoma in situ ) , nodular BCC, lentigo maligna, melanoma metastases, T-cell lymphoma, Paget disease, and leishmaniasis as well as prevention of keloid recurrence following surgical excision . Although imiquimod has been utilized to treat molluscum contagiosum, unpublished randomized controlled trials showed no difference in its efficacy compared to that of placebo .
FDA-approved regimens for imiquimod application are as follows: (1) for anogenital warts – 5% cream three times weekly for up to 16 weeks, or 3.75% cream daily for up to 8 weeks (~50% and ~30% clearance, respectively); (2) for AKs – 5% cream twice weekly for 16 weeks, or 2.5–3.75% cream daily for two 2-week cycles separated by 2 weeks without treatment (~50% and ~35% clearance, respectively); and (3) for superficial BCC – 5% cream five times weekly for 6 weeks (~75% clearance). The frequency of application and duration of therapy for off-label uses vary.
The mechanism of action is depicted in Fig. 129.5 . In animal models, imiquimod's antiviral and antitumor activity is explained at least in part by the effects of IFN-α .
The most common adverse reactions to imiquimod cream are erythema, edema, scaling, erosion, and ulceration at the site of application ( Figs 129.6 & 129.7 ). These reactions tend to be more intense and frequent in patients with actinic damage. Development of erosive pustular dermatosis of the scalp has been associated with the use of imiquimod for AKs of the scalp , and reactions with histologic findings mimicking those of lupus erythematosus have been described. Flu-like symptoms such as fatigue, fever, headache, diarrhea, and myalgias occur in ~1–2% of patients, but systemic immune alterations have not been described.


Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here