Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Disc space narrowing and osteophyte formation are features of the general spine condition known as intervertebral disc (IVD) degeneration
IVD degeneration is an age-related condition
IVD degeneration is highly heritable
The burden of IVD degeneration predicts the likelihood of low back pain episodes
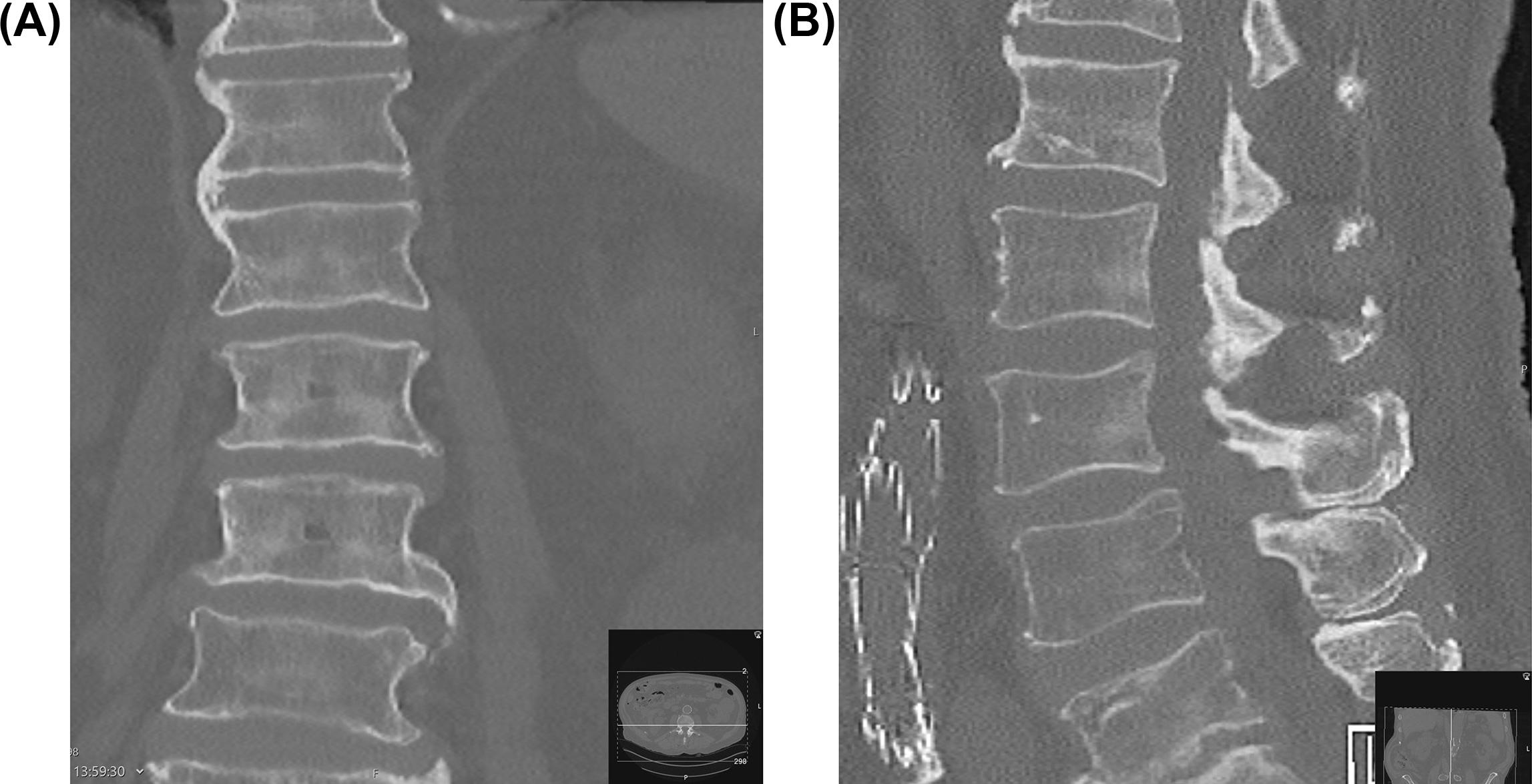
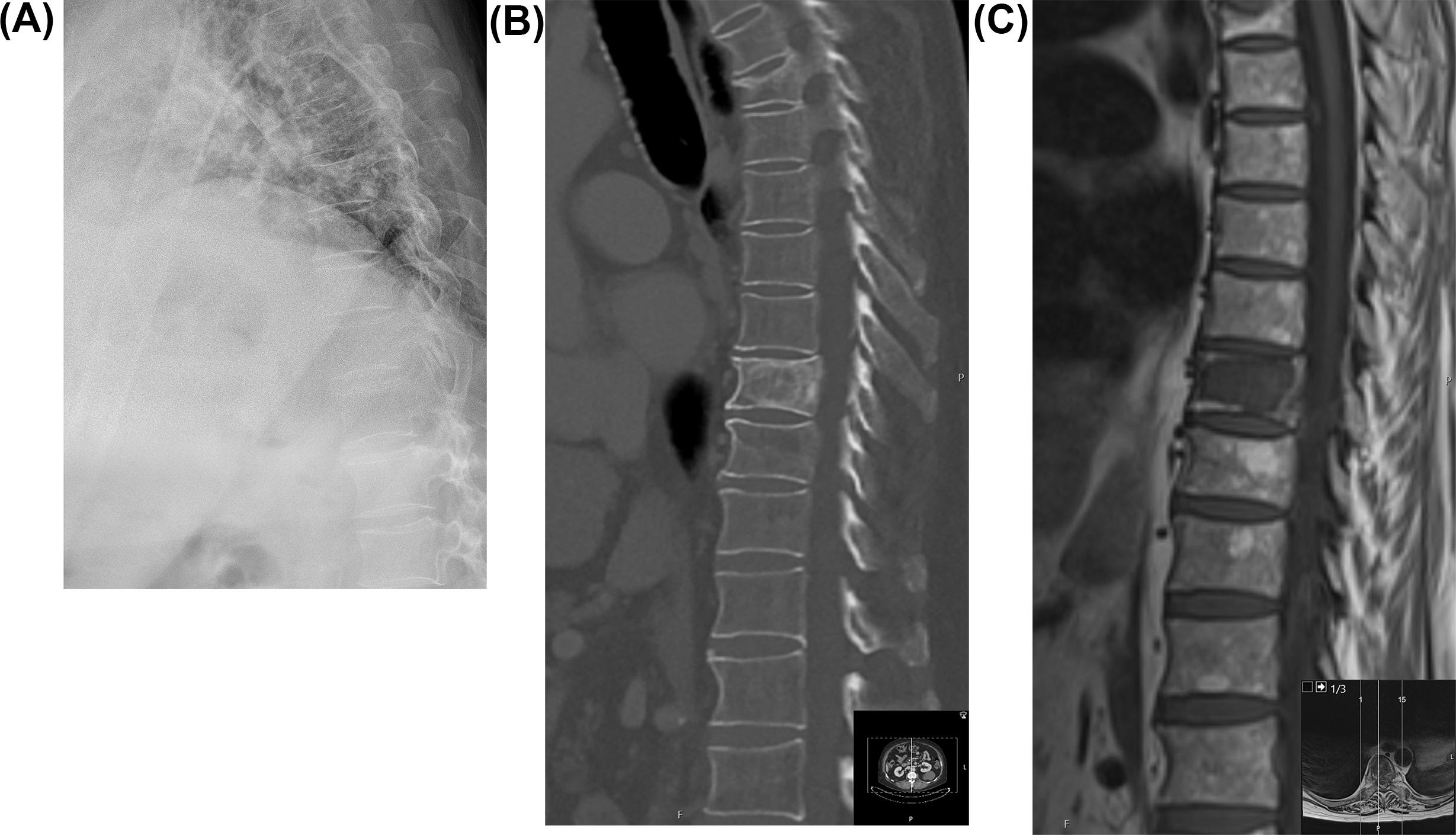
The outgrowth of small spicules of bone—osteophytes—from the endplate of the vertebral body is one of the hallmarks of the bony response intervertebral disc (IVD) degeneration ( Fig. 7.1 ) (see Chapter 6 ). Such degeneration is characterized by activation of matrix metalloproteinases, reduction in the length of proteoglycans attached to types I and II collagen, and consequently a loss of hydrophilicity of the matrix molecules [ ]. The loss of water from the IVD is evident on T2 weighted magnetic resonance (MR) scans as a change from bright white IVD to light gray, then dark gray ( Fig. 7.2 ). In addition, IVD height is lost and this feature is known interchangeably as loss of IVD height and IVD space narrowing, the latter because early imaging using plain radiology film showed a space between vertebrae rather than an image of the IVD itself ( Fig. 7.3 ).

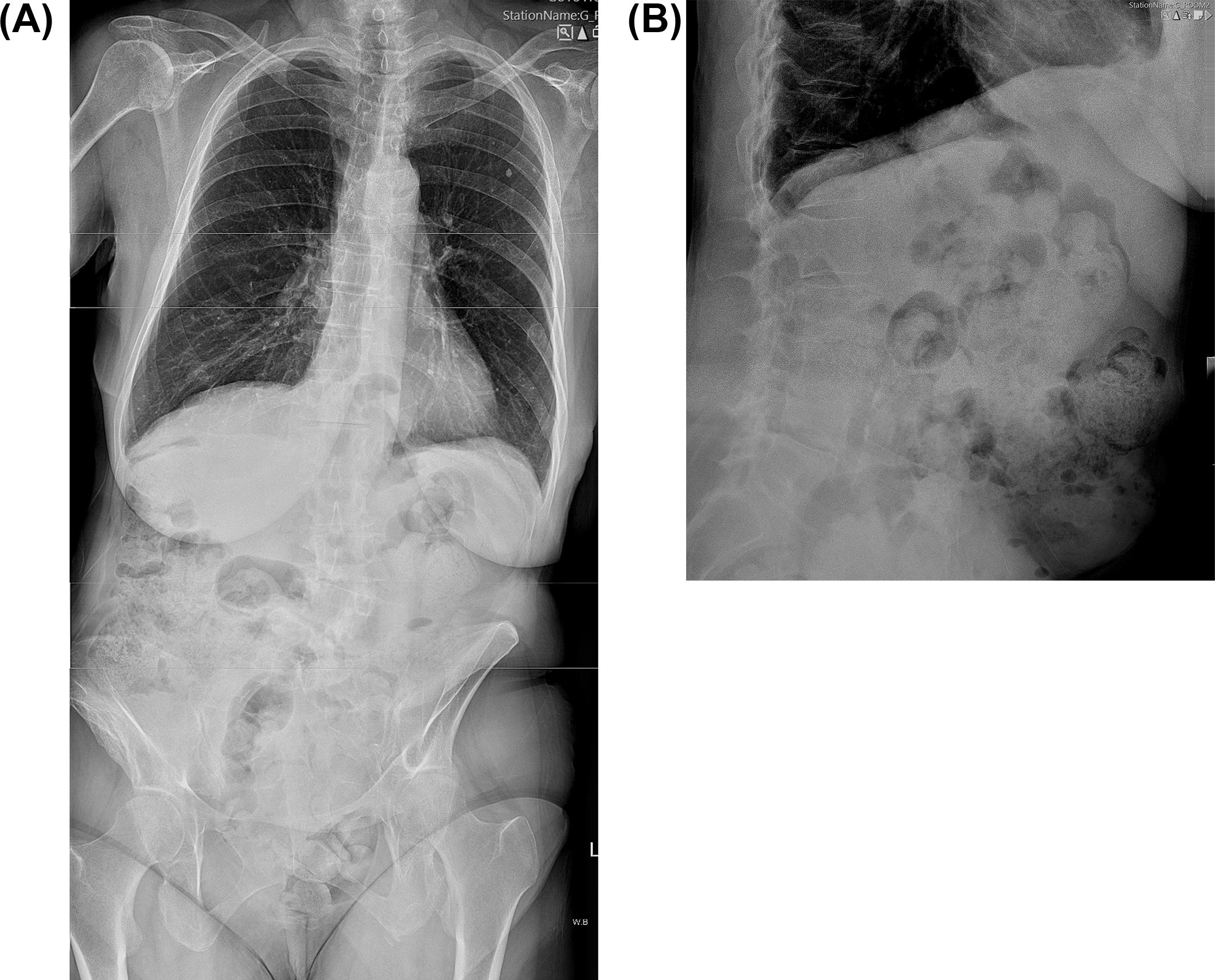
The features of lumbar IVD (osteophyte formation and loss of IVD height on MR scan) are correlated [ ], and both are known to be heritable [ ]; that is, a significant proportion of phenotypic variation is accounted for by genetic factors. In fact, twin studies have shown a surprisingly high level of heritability (60%–80%)—which varies by spine level—for a condition that was long considered to be largely occupational [ ]. In this chapter, we discuss the changes that take place at the cellular level and describe the histology of osteophytes and the IVD as it loses height and degenerates. We describe how the two features are related to one another and their epidemiology. The most important question, however, is their contribution to low back pain, a highly prevalent condition worldwide, with considerable social and economic costs. Low back pain now causes more disability on a global level than any other condition [ ]. Finally, we discuss the rare complications that may arise from osteophyte formation.
The primary cause of osteophyte formation at any joint is thought to be joint instability, detected perhaps by proprioceptive receptors. Osteophyte growth is an attempt to stabilize the joint [ ]; they grow out laterally and appear to try and increase the surface area of the joint. In the spine, osteophytes grow horizontally from the margin of the vertebral body. The most likely causes of perceived instability are IVD degeneration or facet joint osteoarthritis (see Chapter 14 ), which is closely related (see later) ( Fig. 7.3 ). It is difficult to perform well-designed studies in humans to work out the sequence of events but longitudinal cohorts are beginning to address this important issue [ ]. The main cause of joint instability is believed to be changes in the IVD triggered by endplate damage (see Chapter 10 ); loss of IVD height occurs with subsequent peripheral annular bulging. IVD cells are lost, and matrix metalloproteinases degrade the proteoglycans are degraded and water escapes, some through fissures formed with degeneration of the annulus fibrosus (AF), resulting in further thinning of the IVD; vertebral endplate sclerosis and osteophyte formation ultimately follow. One study found anterior and lateral traction osteophytes in greater numbers than posterior and posterolateral traction osteophytes [ ]. Rarely, the osteophytes can lead to local pressure effects and, rarely, serious complications (see later).
One large American cohort study, the Johnson County Osteoarthritis Project, has found different radiographic biomarkers associated with facet joint osteoarthritis and IVD space narrowing relate to osteoarthritis at other sites [ ]. For example, there was a close relationship between lumbar spine IVD and hand and knee osteoarthritis, which was not seen at the hip. This highlights the close relationship between IVD, facet joint osteoarthritis and osteoarthritis of the cervical and lumbar spines and peripheral joints, which has been reported in many epidemiological studies [ ]. The relationship between IVD degeneration facet joint osteoarthritis is discussed further in the following.
Visual assessment and subjective evaluation remain the commonest method for classifying osteophytosis and IVD space narrowing into mild, moderate, and severe, using standard imaging techniques. A number of coding methods have been devised for epidemiological study but standardization of the scales used to code these features has been slow despite numerous calls for international agreement [ ]. Different specialties tend to use different scales: for example, surgeons use the Pfirrmann or Schneiderman classifications to characterize the overall degree of degeneration, while epidemiologists are working with more granular scales that code each radiological feature separately [ ]. An international working party was set up (Hong Kong, 2013) to try and address this and set international standards through professional groups, such as the International Society for the Study of the Lumbar Spine. In addition, machine learning methods are used to try and improve image interpretation, particularly the correlation between imaging features and symptoms, by reducing the noise introduced by human error in coding [ ].
Measuring the osteophyte extension beyond the vertebral body margin and commenting on the temporal orientation of the osteophytes are only performed by a few people. Clearly, the imaging tool used has an important influence—plain films only demonstrate osteophytes in a single plane while they may occur throughout the margin of the vertebral endplates, to a variable degree. MR is also not the optimal imaging method for bone but is the best for IVD. Some classify according to location of osteophytes on the vertebral body as anterior, lateral, and posterior osteophytosis ( Fig. 7.4 ).
Both loss of IVD height and osteophyte formation are clearly age-related traits, and this has been recognized for centuries but the first formal epidemiology studies date from the 1960s [ ]. Both features are observed occasionally in children, have a low prevalence in adolescents and young adults [ ], and become highly prevalent—almost universal—in those over 60 years old [ , ]. Degenerative change in the vertebral column is seen in all ethnic groups but there are some differences, particularly in osteophyte floridity, which may reflect different genetic background. Although there is a correlation between different forms of imaging, differences in prevalence may also reflect the coding methods used to determine the presence or absence of osteophytes and IVD narrowing. The most widely reported method is plain radiography for reasons of cost and availability, and large cohorts have been assembled for clinical studies [ ] and drug trials in osteoporosis. Although the imaging in these studies has been selected for the incidence and prevalence of vertebral fracture, the plain radiographs have lent themselves well to studies of IVD. The superior method of MR imaging is increasingly used because the costs are falling, and collections now exist in the United States, United Kingdom, Hong Kong, and Japan that are vital to performing well-powered studies. Finally, there are reports of a few studies that have examined postmortem specimens of the spine.
In the study of Karasik et al. [ ], a significant association between increased anterior lumbar osteophytes and prevalent abdominal aortic calcification was demonstrated, suggesting a link between IVD and cardiovascular disease. Whether there is truly a pathogenic connection involving calcium metabolism or whether both simply represent diseases of aging remains to be determined but there does seem to be a link [ ] ( Fig. 7.1 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here