Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Evaluation of fetal anatomy, including a detailed fetal cardiac examination, is possible in the late first trimester.
Many anatomic abnormalities can be detected in the first trimester, giving families time to make important decisions regarding pregnancy management and the opportunity for early termination of pregnancy to reduce maternal morbidity risks.
Doppler techniques and four-dimensional spatiotemporal image correlation (4D STIC) are modalities used to help examine the fetal heart in detail during the first trimester, although detection rates using STIC technology are reported to be slightly lower than with two-dimensional (2D) sonography.
In experienced centers, or when educational programs are instituted, the reliability and detection rates of first trimester anatomic evaluation have been demonstrated to parallel those of second trimester anatomic evaluation.
The cost effectiveness of first trimester anatomic screening in the general population remains unknown at this time.
It is important to keep the ALARA (as low as reasonably achievable) principle in mind when performing detailed anatomic evaluation in the first trimester. This point becomes particularly important when using modalities that employ higher frequencies, such as power Doppler sonography.
The thermal index for soft tissue (TIS) and thermal index for bone (TIB) should be kept below 1.0.
First trimester fetal anatomy evaluation has developed over the past several decades. As a result of advances in technology, the resolution of sonography has improved, and subsequently, our ability to image the fetus with increasing detail. Initially, first trimester sonography was limited to use as a means of measuring crown-rump length for pregnancy dating. As the utilization of high-frequency transvaginal sonography evolved through the 1980s, sonographic investigation of the anatomic development of the embryo and early fetus became possible. With the boom in first trimester aneuploidy screening in the 1990s came the discovery of increased nuchal translucency as a marker of aneuploidy, propelling further investigation into the potential for first trimester anatomy evaluation. As reports of normal and abnormal first trimester fetal anatomy continued to surface in the literature and detection rates and technical aspects began to be published, our ability to image the fetus in the first trimester became more refined. Today, the possibility of performing a detailed anatomic assessment, including fetal echocardiography, between 12 and 14 weeks is a reality.
The first trimester marks a period of rapid fetal growth and development ( Fig. 5-1 , Table 5-1 ). Prior to embarking on a detailed description of the use of sonography to assess fetal anatomy in the first trimester, it is important to understand the structure and development of the embryo and fetus, as this directly impacts the potential of ultrasound to detect abnormal structures. Note that embryonic development is typically described by weeks post conception, whereas sonographic findings are described using clinical menstrual age dating. Menstrual age dating is typically 2 weeks greater than conceptional age (see Chapter 6 ).

Week 4: The 4th week marks significant development of the embryonic body, with formation of the primordium of the brain from the previously formed neural tube, the oropharyngeal membrane, and the foregut (primordium of the pharynx, esophagus, and lower respiratory tract). Primitive erythroblasts enter the embryo proper at 4 weeks' gestation, and the primordial heart begins to develop and contract. During the 4th week, hematopoietic cells begin to colonize the newly forming liver, which serves as the major site of hematopoiesis. As the embryo folds in both the cephalocaudal and lateral directions, the intraembryonic coelom is divided by the septum transversum (future diaphragm), located just caudal to the heart. The septum transversum divides the primordial body cavities into the cranial pericardial cavity and the caudal peritoneal cavity. The maxilla and mandible begin to take form. The prominence of the forebrain results in the classic C-shaped curve of the embryo. Caudal folding results in the caudal eminence, a tail-like structure, with lower limb buds visible by the end of the 4th week.
Week 5: The 5th week is marked by accelerated growth, with head growth outpacing the other embryonic structures. The face begins to take form, and the mesonephric ridges develop to mark the site of the future kidneys. The embryonic heart develops into a four-chambered structure.
Week 6: By the 6th week, the limb buds begin to differentiate into upper and lower limbs with large hand plates, which develop primordial digits. The lower extremities lag behind the upper limbs by approximately 4 to 5 days. The primordial ear develops and the eyes become obvious as the retina becomes pigmented. The fetal liver occupies the majority of the abdominal cavity at the 6th week. As the rapid growth of the intestines exceeds the growth of the abdominal cavity the physiologic herniation of the intestines into the umbilical cord occurs. Spontaneous twitching movements and reflex responses to touch begin to take place.
Week 7: The most notable change in structure at 7 weeks is limb development as the digits become distinct and ossification begins. The plantar surfaces of the feet face each other. The developing central nervous system (CNS) is divided into the prosencephalon (forebrain), mesencephalon (midbrain), and rhombencephalon (hindbrain); however, the midline falx cerebri has not formed, and what will become the lateral ventricles is a single ventricle at this point.
Week 8: The 8th week marks the final week of the embryonic period. By then, the heart has developed all of its adult components, pulmonary veins, tricuspid and mitral valves, coronary arteries, inferior and superior vena cava, interventricular septum, and aortic and pulmonary valves. Near the end of the 8th week, the choroid plexus begins to fold inward and the falx cerebri develops, thus dividing the single ventricle into two lateral ventricles. The face takes form over the course of weeks 5 through 8. By the end of the 8th week, the mandibular, maxillary, and nasal processes have merged in the midline, and the primary and secondary palates have fully fused to produce the two palatal shelves of the definitive palate.
Weeks 9 to 12: At 9 weeks, 50% of the fetus is composed of the head, and the 9th through 12th weeks are marked by acceleration in body growth. At 10 weeks, the knees begin to rotate ventrally and the soles of the feet become reoriented with the plantar surface on the ventral aspect. In the 10th week, the hindbrain develops and the cerebellum takes form. It is not until 12 weeks that the corpus callosum begins the first stages of development that will continue through the second trimester. From 10 to 12 weeks, the male and female genitalia differentiate. The intestines begin to return to the abdominal cavity in the 10th week with full return by the end of the 11th week. Between weeks 10 through 12, the two shelves of the definitive palate fuse in the midline. Primary ossification centers appear by 12 weeks; the lower limbs have reached their final relative length, and the upper limbs are nearly at their relative length. Between 9 and 12 weeks the fetal kidneys begin urine production and excretion into the amniotic fluid.
Weeks 13 to 14: Weeks 13 through 14 are marked by more fetal growth. Limb movements become coordinated by 14 weeks. The eyes begin to rotate from anterolateral to anterior.
In the embryonic period, the brain is hypoechoic and characterized in the sagittal plane by the presence of three echogenic structures: prosencephalon (forebrain), mesencephalon (midbrain), and rhombencephalon (hindbrain). The rhombencephalon can be visualized as early as 7 weeks and is the most prominent cavity owing to its relatively larger size compared to the other two cavities. These fluid-filled cavities are positioned in a triangular fashion, laid out as to predict their future site of structure and function. The base of the triangle is formed by the forebrain in the anterior position and the hindbrain in the posterior position with the midbrain forming the apex of the triangle in between ( Fig. 5-2 ).

The cerebral hemispheres are only tiny buds at 7 weeks, but by 9 weeks Blaas and associates demonstrated the appearance of measureable hemispheres in 79% of embryos with visualization in all fetuses by 10 weeks. As the hemispheres grow, they conceal the diencephalon and meet in the midline at 11 to 12 weeks. At 12 weeks the mean measurements of the cerebral hemisphere in the sagittal view are length 16.4 mm (12.4-20.9 mm); width 6.1 mm (4.2-8.4 mm); and height 2.0 mm (1.4-2.5 mm). As the first trimester progresses from the 8th week onward, the mesencephalon gradually moves toward a more central location, and the third and fourth ventricles become more organized with a distinct isthmus visible between the cavities of the prosencephalon and mesencephalon by the 9th week.
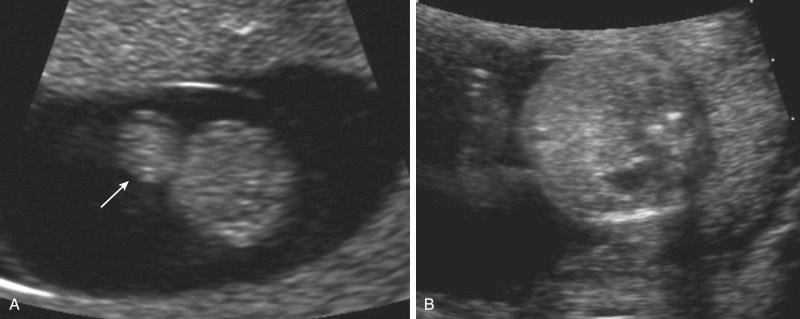
At 7 weeks, a single ventricle is visible, as the midline falx cerebri has not yet developed. Timor-Tritsch and colleagues demonstrated variability in the development of the falx. Although the falx was visible in the majority (75%) of embryos by 9 weeks, in a small proportion the division of the ventricles was not visible until the 10th week, when the falx was clearly visualized dividing the two lateral ventricles in all embryos. The choroid plexus can be visualized routinely within each of the lateral ventricles by the middle of the 9th week, and by the 12th week it fills most of the space of the lateral ventricles ( Fig. 5-3 ).

At 12 weeks, the corpus callosum is not visible, but the trunk from which it will continue to develop may be seen. The cavum septi pellucidi (CSP), an important marker of normal CNS development, can be seen in 40% of pregnancies at 15 weeks and in 82% at 16 to 17 weeks.
The rhombencephalon is the most obvious structure of the early embryonic CNS. As the cerebellar hemispheres grow, they become measurable by the middle of the 10th week and appear to meet in the midline by 11 to 12 weeks. The choroid plexuses of the fourth ventricle are visible by the middle of the 10th week as echogenic areas that traverse the roof of the fourth ventricle.
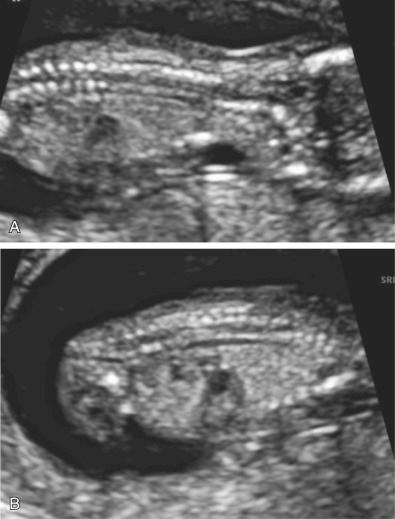
The spine will be detectable as two parallel lines as early as the 8th week in a majority of embryos. The cervical, thoracic, and lumbar spine can be visualized in 80%, 81%, and 72% of fetuses between 11 and 12 weeks and 89%, 87%, and 72% of fetuses between 13 and 14 weeks. The sacral spine is more difficult to visualize in the first trimester, with visualization rates of 35% between 11 and 12 weeks and 48% between 13 and 14 weeks ( Fig. 5-4A and B ).
The bony cranium begins to ossify at 9 weeks and can be precisely measured after 9 weeks using high-frequency transvaginal sonography. Using a combination of transvaginal and transabdominal sonography, Souka and colleagues were able to visualize the fetal head, including the complete cranium and the presence of the falx in all cases between 11 and 14 weeks' gestation ( Fig. 5-5A ).
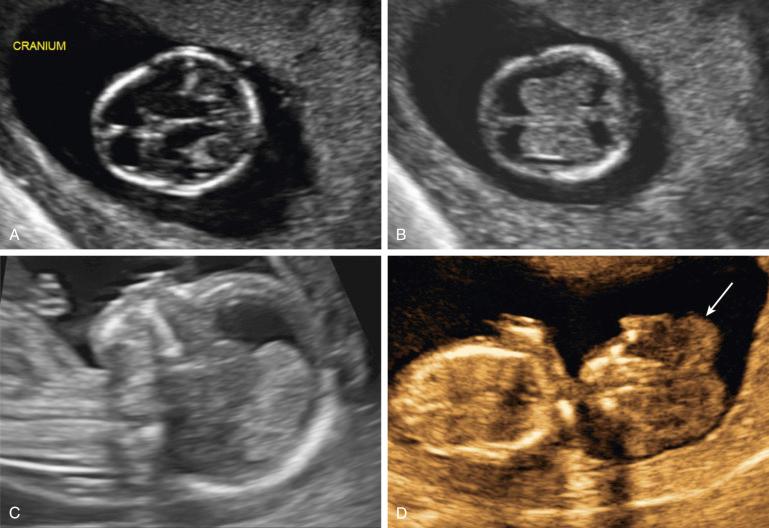
The structure of the face changes dramatically throughout the first trimester and therefore is not reliably imaged until the 11th or 12th week. Souka and colleagues were able to visualize the fetal face, including the orbits, lenses, and profile 99.7% of the time using a combination of transabdominal and transvaginal sonography from 11 to 14 weeks. In addition, there does not seem to be a significant difference in the ability to detect the structures of the face, including the lenses, profile, nose, and lips between 11 and 12 weeks compared to 13 and 14 weeks. In the embryonic and early fetal periods, the forehead is the dominant feature of the developing human face. After 11 weeks, the fetal profile takes on the expected contour with balance between the mandible, the maxilla, and the forehead. At 12 weeks a coronal section of the face can reliably be obtained and allows assessment for symmetry through imaging of the orbits, mandible, and maxilla ( Fig. 5-6 ). In the coronal section of the face, the fetal lenses can be visualized as an echogenic ring with a sonolucent center in 91% of fetuses at 11 to 12 weeks' gestation.

By 11 weeks, imaging of the palate and lips can be reliably performed ( Fig. 5-7 ). The nose also becomes fully formed by 11 weeks, and the presence or absence of the nasal bone can be evaluated at this time. The frontomaxillary facial angle measured using three-dimensional (3D) volumes of the fetal face has been investigated as a screening tool for trisomy 21, which is associated with significant flattening of the face. The frontomaxillary angle decreases with increasing crown-rump length. Nomograms for chromosomally normal fetuses have been reported.

The international 3D focus group has published recommendations regarding imaging of the fetal face in the first trimester. These recommendations include imaging specifications that are unique to the developing first trimester face and are particularly useful for correct visualization of the nasal bone and excluding face malformations.
Evaluation of the nuchal anatomy in the first trimester has been a stepping stone that has led to the development of fetal anatomic assessment in the first trimester. The measurement of the nuchal translucency (NT) is now a widely accepted tool used for first trimester aneuploidy screening. The nuchal translucency is gestational age dependent and can be reliably measured from 11 to 14 weeks' gestation ( Fig. 5-8 ).
The fetal chest, imaged between 11 and 14 weeks' gestation, demonstrates improved visualization of the pulmonary and cardiac structures occurring over the course of time. Using a combination of transvaginal and transabdominal sonography, Timor-Tritsch and colleagues demonstrated a significant difference in the ability to visualize the fetal lungs between 13 and 14 weeks compared with 11 to 12 weeks (77% vs. 64%, P = 0.02). The fetal diaphragm was visualized by the same group in 87% of fetuses from 11 to 12 weeks ( Fig. 5-9 ).

Using high-frequency transvaginal sonography, the fetal heart motion is first visualized from 5 weeks and 4 days to 5 weeks and 6 days, with an average rate at 6 weeks of 104 bpm. In a longitudinal study of cardiac development in the first trimester, Blaas and colleagues demonstrated that the fetal heart rate follows an inverted- U curve from 7 weeks to 12 weeks. The fetal heart rate was noted to be at 138 bpm at 7 weeks, peaks at 175 bpm at 9 weeks, and then decreases to 166 bpm at 12 weeks.
Although it has been demonstrated that the major structures of the heart can be visualized as early as 10 weeks, the success rate of visualizing these structures has been shown by several authors to improve with each advancing week. In addition, Gembruch and colleagues have demonstrated better visualization using transvaginal sonography compared to transabdominal sonography from 10 to 13 weeks, equivalent visualization of the two approaches at 14 weeks, and after 14 weeks superiority of the abdominal approach.
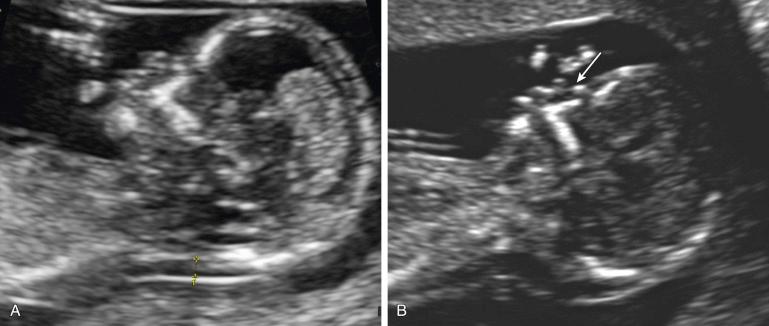
Situs can be confirmed by documenting appropriate orientation with the aorta to the right of the spine, inferior vena cava anterior and right of the spine, and the heart lying on the left side of the chest with the appropriate axis. Compared to the 45 ± 10 degree cardiac axis in the mid-second and third trimesters, the cardiac axis in the first trimester begins much more midline and gradually rotates to the 45-degree position by about the 12th week. From the 8th through the 9th weeks the heart sits at approximately 25 ± 12 degrees, from the 10th through the 11th week the axis rotates to 40 ± 9 degrees, and between the 12th and 15th weeks it reaches the final cardiac axis at 49 ± 7 degrees ( Fig. 5-10 ).

At 12 weeks the four-chamber view can be obtained reliably in 90% of fetuses using transvaginal sonography. Two equally sized ventricles and atria with an intact ventricular septum up to the cardiac crux are seen in the normal four-chamber view ( Fig. 5-11A and C ). The atrial appendages are more pronounced in the first trimester fetal heart compared to later in gestation, and the ventricles are in a spiral arrangement; however, the resolution of 2D sonography limits our ability to appreciate these differences, which have been demonstrated using 4D high-resolution transvaginal sonography (4D HREVS). The right and left ventricles can be difficult to distinguish because of their spiral orientation, but they can be distinguished by identification of the offset of the atrioventricular valves with the tricuspid valve on the right side positioned slightly lower than the mitral valve on the left. The atrioventricular septum grows relatively late in the first trimester, and as such, the offset of the mitral and tricuspid valves may not be apparent until after 12 weeks. Doppler sonography can be used to help identify the morphologic features of the right and left ventricles. Lombardi and colleagues described the “banana-shaped” right ventricle and “ballerina shoe–shaped” left ventricle with its less severe curvature. In addition, a combination of color Doppler and power Doppler is also recommended to help define the septal aortic continuity, evaluate normal valvular flow, and show pulmonary vein flow into the left atrium. The short axis view of the great vessels, which demonstrates the wrapping of the pulmonary artery from the right ventricle continuous with the branching of the ductus arteriosus, also demonstrates the tricuspid and pulmonary valves and is therefore useful for measuring flow across these valves. It should be noted that in the first trimester it is particularly important to apply the ALARA principle and keep the thermal index below 1, which can become an issue when Doppler is used.
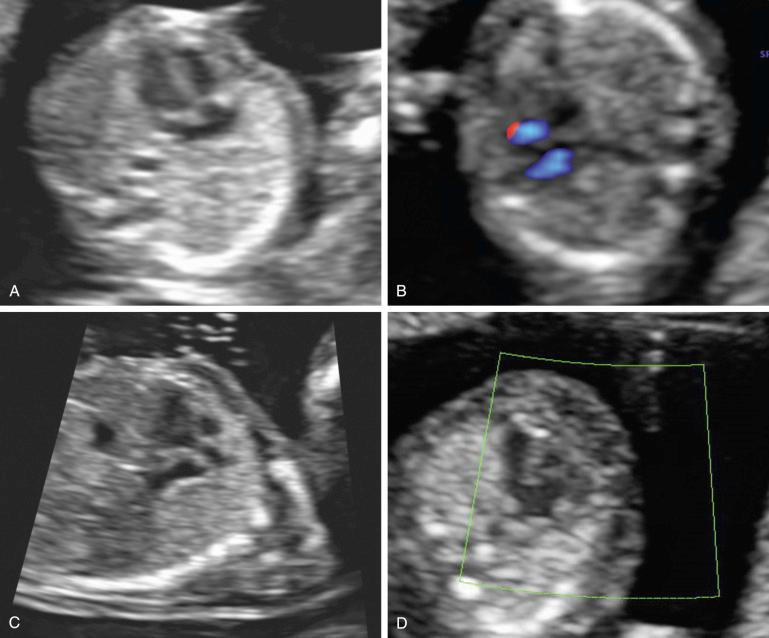
Demonstration of the outflow tracts can be achieved in many fetuses by the 12th week, with improved visualization in the 13th week. The long-axis view of the aorta with the aorta arising from the left ventricle adequately demonstrates the left ventricular outflow tract (LVOT) in 68% of fetuses in the 12th week, increasing to 92% in the 13th week ( Fig. 5-11B ). In the long-axis view of the aorta, the continuity of the ventricular septum with the anterior wall of the aorta and the anterior mitral leaflet with the posterior wall of the aorta can be visualized. By angling the transducer toward the fetal right side, if the aorta and pulmonary artery are oriented in their normal crossover configuration, the long-axis view of the pulmonary artery can be obtained, which demonstrates the right ventricular outflow tract as the pulmonary artery branches off the right ventricle cephalad toward the fetal left side.
The aorta is seen arising centrally from the left ventricle and the pulmonary trunk from the anterior right ventricle with the pulmonary trunk crossing over the ascending aorta to the left side of the fetus ( Fig. 5-12 ). The ductal arch is anterior to the transverse section of the aortic arch and heads almost directly posterior toward the spine where it converges with the descending aorta to the left of the spine ( Fig. 5-13 ). The three-vessel view with the pulmonary trunk originating from the right ventricle, the aorta, and the superior vena cava is useful for identifying and comparing the sizes of the great vessels. The use of color Doppler can confirm forward flow through the outflow tracts. Using power Doppler, the normal orientation of the great vessels can be demonstrated using the X sign, which identifies the normal crossover of the pulmonary trunk over the aorta, and the b sign, which demonstrates a transverse plane at the level of the sweeping arch of the aorta and near linear path of the pulmonary artery.


Nomograms for cardiac biometry between the 10 and 15 weeks have been published by Smrcek and coworkers.
Examination of the abdomen in the first trimester begins with evaluation of the ventral wall ( Fig. 5-14 ). The physiologic herniation of the midgut can be seen as early as 7 weeks and becomes most identifiable from 9 to 10 weeks with retraction back into the abdominal cavity from the middle of the 10th week through the 11th week ( Fig. 5-15 ). By 12 weeks the thickening of the umbilical cord associated with midgut herniation has resolved, and the umbilical cord insertion into the abdominal cavity is able to be evaluated.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here