Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Spinal infection is a multicausal disease. The three most common are hematogenous spread, direct spread, and direct inoculation, which is usually iatrogenic.
Arterial hematogenous spread can be due to an infectious focus anywhere in the body. This can be responsible for pyogenic and nonpyogenic infections and is the most common source of infection. It was previously believed that hematogenous spread can occur through venous or arterial spread, but there is now evidence to suggest that venous spread is unusual.
The second main cause of spinal infection is direct spread from an infectious focus adjacent to the spine. This can be located virtually anywhere in the trunk of a patient. Spread from infection in the pelvis, perirenal, pleural, and pharyngeal area is particularly common.
The third main group of spinal infections results from direct inoculation, and these are virtually always due to iatrogenic infections, that is, infection of the spine after a medical intervention. This can be due to spinal surgery but is also seen after discography, myelography, facet joint injections, and epidural blocks/anesthesia but increasingly also after minor interventions, such as paraspinal injections of trigger points or acupuncture and also after vertebroplasty.
The commonest infectious organism is Staphylococcus aureus, which is encountered in about 60% of cases. This holds true for all three groups discussed previously. Apart from S. aureus, virtually any infectious agent may be found in spinal infection. Bacterial infections are much more common than fungal or parasitic infections. Apart from Staphylococcus and Mycobacterium tuberculosis , commonly found infectious agents are Escherichia coli and gram-negative bacteria in immunocompromised patients. Intravenous drug users often suffer Pseudomonas infections.
Spontaneous spinal infections most commonly occur in the elderly and the immune compromised. Recognized risk factors are advanced age, male gender, immunosuppression, intravenous drug abuse, human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), diabetes mellitus, use of corticosteroids, chemotherapy, rheumatologic or immunologic disease, hepatic or renal failure, malnutrition, myelodysplastic disease, and so on. Increased frequency of tuberculosis in developed as well as underdeveloped countries and more chronically debilitated patients lead to an increased incidence of spinal infection. The peak incidence is in the sixth and seventh decades of life, and more than 50% of patients with spinal infection are older than 50 years. Large studies found incidences of about 2.2 cases per 100,000 of vertebral osteomyelitis and epidural abscess. Spinal infection represents about 2% to 8% of all cases of osteomyelitis.
Spinal involvement in tuberculosis is seen in about 50% of all patients with musculoskeletal involvement. However, musculoskeletal involvement in tuberculosis overall is uncommon and occurs in only 1.5% to 3% of cases. Around one third of the world's population harbors tuberculosis and remains a substantial problem.
Spinal infections due to other organisms, such as Brucella or fungal infections, are comparatively rare in the Western world.
Iatrogenic spinal infections can occur after a large number of procedures. They occur in up to 4% of all spinal surgery patients and represent up to 30% of all cases of spinal infection. The use of preoperative antibiotic prophylaxis dramatically decreases the risk of postoperative infection by about a factor 10.
The incidence and pathway of spinal infection can also be differentiated according to age. The first age group includes babies usually up to the age of 6 months. At this age, the intervertebral disk has still a vascular supply, and direct hematogenous spread into the disk is the most common mode of infection. The babies affected are usually severely ill and present with septicemia.
The next age group includes slightly older babies and younger children up to 5 to 7 years. These children have lost the direct vascular supply to the intervertebral disk but still have vascular channels in the cartilaginous vertebral body end plate that enables infectious pathogens access to the immediate vicinity of the intervertebral disk. However, the good vascular supply also enables a strong immune response, and affected children often present with only local symptoms and a benign clinical course. This has led to speculation that this disease is actually an aseptic diskitis, but this theory is now largely discounted in favor of an infectious process. Infections in this age group are fairly rare.
The third distinct age group includes people older than 50 years and patients with an underlying systemic disease or drug addicts. More than 50% of patients with spinal infection are older than 50 years. The clinical presentation is often similar to that of the children's group in that onset can be insidious. However, if untreated, the natural history of spinal infection in this age group is grim; in the pre-antibiotic era, mortality was 25% to 70%. Since the advent of antibiotics, this has dropped to about 5% to 20%. Sequelae in survivors can be paraplegia or tetraplegia, and this is seen in about 1% of patients with spinal infection and is more common in patients with cervical spine involvement.
Iatrogenic or postprocedural spinal infections are an increasing problem. They represent up to 30% of all cases of pyogenic spondylodiskitis, although some authors put the incidence as low as 2.5%. A large variety of procedures can give rise to spinal infection, as described in the section on etiology. Patients with an underlying systemic illness are particularly at risk. The use of corticosteroids in paraspinal injections is also a major risk factor. However, even harmless procedures, such as acupuncture, can be the cause of a spinal infection. With the increase in paraspinal and or spinal injections/procedures, especially for pain control, the problem of iatrogenic infection is likely to rise.
Preprocedural antibiotic prophylaxis can dramatically reduce the risk of an infection, but this is not feasible in permanently implanted catheters. The risk of spinal infection after open back surgery is quoted as between 3% and13% without antibiotic prophylaxis and as less than 1% with antibiotic prophylaxis. Less invasive procedures have lower risks, for example, for discography, the infection risk is quoted as about 1%.
The area of the spine most commonly affected by spinal infection is the lumbar spine. This is followed by the thoracic spine; the cervical spine is least commonly affected.
Polymicrobial spondylodiskitis, that is, concurrent infection with more than one infectious agent, is typically seen in a postoperative setting. The incidence here is as high as 50% of all cases. Otherwise, polymicrobial spondylodiskitis is unusual and seen in overall less than 2.5% of cases.
In polymicrobial infection, successful diagnosis and antibiotic treatment of only part of the pathogens will lead to an initial clinical improvement with subsequent renewed clinical deterioration. There is a particular risk of this in patients with concomitant infection with pyogenic and tuberculous pathogens if only the pyogenic infection is initially diagnosed. Although this constellation, overall, is rare, it does occur particularly in fistulating tuberculosis. Here, tuberculosis is the primary infectious agent, with secondary superinfection with pyogenic pathogens after the fistulation. Therefore, for fistula-forming infection, special efforts should be made to rule out tuberculosis.
The clinical presentation of spinal infection is highly varied and ranges from virtually asymptomatic patients to those who are gravely ill. The severity and type of signs and symptoms depend on the spinal level of infection, the offending organism, and the host response. The clinical symptoms are usually nonspecific. Back pain (often localized) coupled with local tenderness, increased temperature, and raised C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are common. However, even back pain is seen in only 92% of spinal infections, and, therefore, about 8% of patients will not describe pain! Increased temperature is seen in only about a third of patients. Leukocytosis can be present but is an unreliable sign. CRP is usually (but not always) elevated in spinal infection.
The back pain caused by spinal infection often worsens with standing and activity and is improved by non–weight bearing. Night pain can occur in varying severity. The varied and often vague symptoms make it difficult to differentiate spinal infection from simple mechanical back pain. *
* References .
If the infection involves the epidural space, and, in particular, when epidural abscess formation occurs, the pain becomes intense and neurologic impairment is seen. The patient is usually clinically quite unwell. The neurologic signs are often vague and affect several levels. This is due to epidural abscess formation, often extensively tracking within the spinal canal spanning several vertebral levels.
The clinical diagnosis of spinal infection poses a particular challenge in patients with underlying preexisting pathologies and problems, such as patients with preexisting chronic back pain, patients after back surgery, patients with paraplegia or tetraplegia, and patients with immune compromise. In these patient groups, the ESR often is also unreliable, and the diagnosis rests on CRP and imaging findings; however, CRP can be normal, despite infection.
In patients with preexisting chronic back pain, a change in the type or quality of pain can be a sign of spinal infection. However, this finding is nonspecific and, more frequently, is due to deterioration of mechanical back pain. In patients with previous back surgery, recurrence of pain can be the only sign of clinical infection. The recurring pain can be similar to the preoperative pain, and the clinical presentation is often nonspecific. Fever is not common in these cases. Leukocytosis is seen in less than 50% of patients. An elevated CRP is the most specific finding. Postoperative diskitis should be suspected if, on postoperative day 6, ESR is greater than 45 mm/hr, CRP is greater than 2.5 mg/dL, or no reduction in these parameters from the immediate postoperative values has taken place. The CRP value usually peaks on day 2 or 3 postoperatively and should be normalized by day 14 postoperatively. Similarly, elevation of ESR to 2 to 4 times its normal value is suspicious for postoperative spinal infection.
Biopsies and blood cultures aid the diagnosis and help identify the infective pathogen but do not exclude spinal infection, if negative. The yield of positive cultures varies greatly in the literature between 50% and 90% for biopsies and 25% and 60% for blood cultures. However, the combination of both tests can result in diagnostic yields of up to 96%. If a spinal biopsy is taken, the infected end plate (not the disk) usually results in the highest yield. More sample results in a higher diagnostic yield. Some authors advise routine biopsy of the infected disk, the paravertebral space, and the intervertebral disk. Open biopsy results in 60% to 86% yield but clearly is not the method of choice, unless there is pressing need for surgical decompression. Antibiotic therapy before biopsy or blood culture results in poorer yields. †
† References .
All of the problems discussed result typically in a delayed diagnosis of spinal infection, often by about 2 to 3 months. However, good clinical outcome depends on early diagnosis.
The understanding of the disease process in spinal infection requires a good understanding of spinal anatomy.
In babies younger than 6 months, there is a direct vascular supply to the intervertebral disk. Direct hematogenous infection, therefore, can occur in this age group. As the babies get older, the direct vascular supply disappears, but there are still focal areas seen of vascular channels in the cartilaginous end plate of the vertebral bodies, typically to the age of 5 to 7 years. These enable hematogenous deposition of pathogens into the immediate vicinity of the intervertebral disk. Finally, in the normal adult, the vertebral body end plate poses a considerable barrier to blood-borne infection. However, in severe degenerative disk disease, blood vessels can secondarily invade the intervertebral disk, and direct hematogenous infection can then occur.
In the adult, the spinal column is surrounded by a dense anastomotic network of arteries formed by segmental vessels and their branches. The segmental arteries enter the spinal canal through the intervertebral foramina. Nutrient arteries enter the vertebral body from inside as well as outside of the vertebral canal, and the main arterial supply is usually by bilateral anterolateral arteries and one central posterior artery. The terminal branches of the nutrient arteries are end arterioles. This predisposes to embolic infarctions in the richly vascularized paradiskal area of the vertebrae.
In children, there is a dense anastomosing network of superficial periosteal and intraosseous arteries. The anastomoses become less prominent from the age of 7 years, and, by 15 years, they usually have disappeared and assumed adult configuration. Septic embolization in children, therefore, is rare.
The metaphyseal anterolateral part of the vertebral body, adjacent to the cartilaginous end plates, has a particularly dense vascular supply. This particular area is often the starting point of infections with the oxygen-loving Mycobacterium tuberculosis infections but also for inflammatory spondyloarthropathies and degenerative osteophyte formation.
The paravertebral venous plexus is valveless. It comprises three main parts: the intravertebral venous network, which communicates with the epidural venous network within the spinal canal, which communicates with the paravertebral venous network outside of the spinal canal. In the past, it had been assumed that metastases and infections can spread freely through this network, but several studies have suggested that this is not the case. Metastatic involvement has been observed by continuous spread from paravertebral veins but not as primary venous seedlings, and, similarly, primary venous spread of infection has been discounted.
The main mechanisms of spinal infection are outlined in the paragraph on etiology. It is worth remembering that overall S. aureus is the most commonly encountered pathogen.
Hematogenous spread through the arterial system is the most common mode of spinal infection. Continuous spread from adjacent paravertebral infectious foci and infection by direct inoculation (usually iatrogenic) are less common.
The primary focus of a spinal infection and its pattern of spread is variable, and one has to bear in mind the primary focus, the type and aggressiveness of the pathogen, the host response, and the duration of infection to interpret and understand the imaging features.
In the most commonly encountered scenario of hematogenous spinal infection, the primary infected area is often the anterolateral paradiskal area of the vertebral body. This is due to the increased vascularity in this area and that the vessels here are end arteries susceptible to septic emboli and infarction, as outlined in a previous paragraph. Initially, an inflammatory, edematous bone marrow reaction takes place. Bone destruction, paravertebral spread, and involvement of the adjacent intervertebral disk are secondary.
Subsequently, in early infection, radiographs and CT are normal because no bone destruction has yet occurred, and lack of intervertebral disk involvement and destruction leaves the disk height intact. Nuclear medicine techniques (including PET-CT) can demonstrate increased activity in the affected area, but the spatial resolution is poor, and the findings are nonspecific. MR imaging is the most sensitive and most specific imaging technique for the diagnosis of early spinal infection. Edema-like signal change in the area affected is seen, that is, decreased T1-weighted signal and increased signal in short tau inversion recovery (STIR) and T2, fat-saturated images. Conventional T2-weighted images can be insensitive for the edematous change. Contrast enhancement with a gadolinium chelate typically results in florid contrast agent uptake and enhancement. The early edema-like change is typically limited to the primary infected area, and, therefore, often the anterior vertebral body edge but edematous change of whole vertebral bodies without involvement of adjacent structures is also well recognized.
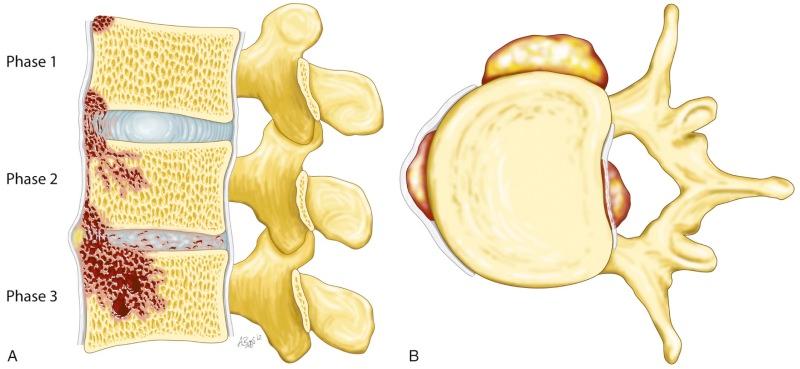
The pattern of spread of a spinal infection is partly dictated by the location of the initial infection and the aggressiveness and type of the infection agent (see Fig. 66-1 ). Pathogens producing proteolytic enzymes (such as S. aureus ) quickly spread into adjacent anatomic structures. The vertebral body end plate and the intervertebral disk are not effective barriers ( eFig. 66-1 ). Disk involvement in infection with pyogenic pathogens is typically seen after 1 to 3 weeks and often leads to the typical picture of involvement of an intervertebral disk and the two adjacent vertebrae. Disk destruction leads to loss of disk height. This can be seen on radiographs and CT, and the concurrent end plate destruction becomes clearer with time and is best appreciated on CT. At 8 to 12 weeks after the onset of spinal infection, reactive bony sclerosis can be seen.

Initial involvement of the intervertebral disk is best appreciated as increased T2-weighted and STIR signal in MR imaging. Often, loss of disk height is seen early in spondylodiskitis, but the disk height can be preserved.
When spread to adjacent tissues occurs, these also show edema-like change. The formation of collections (pus) is best assessed with contrast-enhanced MR imaging, where collections demonstrate lack of contrast enhancement on T1-weighted images.
Pathogens not producing proteolytic enzymes (such as M. tuberculosis ) typically demonstrate a different pattern of spread. Spread of infection is slow and insidious ( eFig. 66-2 ). Complications of the spinal infection, such as fistulating abscesses (either along fascial spaces or even into peritoneum or pleura) or gibbus formation, can be the presenting features. The intervertebral disk can be spared completely or can be involved very late in the disease process. Apparent loss of disk height can be due to disk herniation into vertebral bodies through weakened end plates rather than disk involvement by the infection. Involvement of paravertebral tissue can be in the form of a diffuse inflammatory mass (phlegmon) or abscess formation. Abscess can spread underneath the paraspinous ligaments, elevating them and even leading to compromise of the vertebral vascular supply, ultimately leading to avascular necrosis of vertebrae.

In spinal infection by direct spread, the source of infection is usually best visualized on cross-sectional imaging. In some cases, it can be difficult to differentiate secondary spread to the spine from a primary spinal infection with secondary spread to adjacent structures, but the clinical history and imaging findings are usually unequivocal. Radiographs are relatively insensitive but, in some cases, show paravertebral masses and/or the source of infection.
In spinal infection by direct inoculation, there is usually a relevant clinical history either penetrating trauma or an iatrogenic intervention. Radiographs are usually not helpful, and CT is also of limited use in the early phase before bone destruction occurs. Nuclear medicine techniques are sensitive but nonspecific. MR imaging is the technique of choice. Edema-like changes and possibly abscess formation are seen.
The particular importance of diagnosing spinal infections lies in the life-threatening or disabling nature of this disease. The primary location of the infection and aggressiveness of the infectious agent are important in that they influence the rapidity with which severe complications develop.
Destruction of bone, disk, and ligaments can lead to gibbus formation, instability, and secondary spinal cord compromise. This process usually develops over weeks or even months. The treating clinicians and the radiologist involved should always be mindful and wary of instability. Unexplained deterioration in the clinical condition or even lack of improvement should always be seen as an indication for further imaging, and, if there is concern regarding the mechanical stability of the spine, a spinal surgeon or neurosurgeon should be consulted.
Tracking of abscesses into paravertebral spaces and organs can cause sudden marked deterioration and is one important process leading to morbidity and mortality.
The most serious complications of spinal infection is epidural or meningeal and spinal cord involvement. Epidural phlegmon or abscess formation can lead to rapid deterioration with permanent disability or death if not treated early. Epidural involvement is best demonstrated with contrast-enhanced MR imaging. This allows the differentiation of phlegmon with edema-like signal and marked contrast enhancement from abscess formation with fluid-like signal and absence of contrast enhancement in the abscess collection. Epidural abscesses frequently demonstrate discontiguous spread within the spinal canal, and, if epidural infection is seen, the whole of the spine needs to be imaged. Epidural involvement constitutes a surgical emergency!
Epidural infection can cause spinal cord compromise by direct pressure and by vascular compromise. The vascular compromise is thought to be due to inflammatory mediators and pericapillary edema.
Involvement of the subdural space with meningitis or direct involvement of the spinal cord is relatively rare. *
* References .
Radiography is commonly the first examination performed in a patient with back pain. The first radiographic signs of spondylodiskitis are loss of disk height, vertebral end-plate destruction, and possibly paraspinal soft tissue masses. Depending on the type and virulence of the infection and the immune response, new bone formation or paraspinal calcification may also be seen. With advanced destruction, spinal deformity may occur.
A diagnostic approach solely based on radiographs is problematic because of the poor sensitivity, particularly for early infection and the poor specificity. Destruction of the vertebral end plate is the most specific sign of spinal infection but at the earliest seen several weeks (4 to 6 weeks) into a pyogenic infection, and it can be very much delayed or even not occur at all in infections with low virulence and or tuberculosis. In addition, loss of disk height is nonspecific, and the commonest cause for it is degenerative disk disease. Reactive bone sclerosis takes even longer to develop and is not usually seen before 8 to 12 weeks. Paraspinal masses are not often identified on radiographs and, if seen, are not specific for infection.
Epidural abscess formation, paraspinal soft tissue infection, infection of facet joints, and so on, are at best very poorly, but usually not all, imaged by radiographs.
If children are affected, the radiographic changes develop significantly faster. Loss of disk height may be seen after a few days to 2 weeks, end-plate erosion/destruction may be seen after a few weeks, and reactive bone sclerosis may be seen after 1 month.
CT of the spine is not normally the examination of choice for diagnosis of spinal infection. CT has relatively poor soft tissue contrast and cannot demonstrate the earliest sign of spondylitis: bone marrow edema. It usually can demonstrate paraspinal masses and abscesses but not as well as MR imaging. It can demonstrate loss of disk height, although the differentiation of degeneration and infection can be difficult. Epidural phlegmon and epidural abscess formation are not well imaged.
CT is well suited to demonstrate bone destruction and bony reaction in the form of sclerosis. It also is the best imaging modality to show calcification and gas in soft tissue. CT is the imaging modality that best allows to assess an early healing response (new bone formation) after successful treatment of spondylodiskitis.
CT can demonstrate sclerosis of the remaining bone cortex and marrow at about 6 weeks after the onset of infection, whereas these changes are clearly appreciated on MR imaging at about 12 weeks after the onset of infection. Further application for CT in the diagnosis of spinal infection are in those cases where MR imaging cannot be performed, for example, due to claustrophobia or metal implants. This makes CT valuable for the imaging of postoperative infections.
Ultrasound plays no significant role in the diagnosis of spinal infection, although its use in children has been suggested. It is also sometimes used intraoperatively, especially for localizing epidural abscess collections.
Nuclear medicine techniques were the most sensitive techniques for the diagnosis of spondylodiskitis before the advent of CT and MRI. Isotope bone scintigraphy can demonstrate increased uptake of bone with high sensitivity, but the findings are nonspecific. Single-photon emission computer tomography, also known as SPECT, increases the spatial resolution but not the specificity. With the arrival of infection-specific nuclear medicine techniques came a renewed interest in isotope imaging, particularly for the diagnosis of postoperative infection. Similarly, with the introduction of PET, this has been proposed for the diagnosis of spinal infection.
Postoperative infection is the one area where all imaging techniques suffer from relatively poor sensitivity and specificity. In the postoperative patient, an isotope bone scan will show increased activity whether or not infection is present. Similarly, labeled leukocyte scanning will result in increased activity because hematopoietic bone marrow normally shows increased activity. Combination with gallium-labeled scintigraphy improves the diagnostic accuracy, but overall results are not good. Ciprofloxacin-labeled technetium-99m and fluorine-18 fluorodeoxyglucose (FDG) PET have both been used for the diagnosis of spinal infection and postoperative spinal infection. 99m Tc-labeled ciprofloxacin (Infecton) was supposed to bind only to living bacteria (even if these were immune to ciprofloxacin), although it was found that increased activity is seen in many diseases with increased cell turnover. The 18 FDG-PET imaging similarly is sensitive but nonspecific and positive in many disease processes. FDG-PET imaging can be used for the differentiation of hot and cold abscesses. A hot abscess shows increased activity of the entire abscess cavity, whereas a cold abscess (e.g., in tuberculosis) shows increased activity only in the capsule but not in the cavity of the abscess. *
* References .
PET imaging has also been found helpful in the differentiation of early infection from Modic type I end-plate changes.
MR imaging is the examination of choice in cases of suspected or established spinal infection. Sensitivity, specificity, and accuracy have been reported as 96%, 92%, and 94%, and these are the best values for any imaging method. Other imaging techniques are superior only in postoperative imaging (nuclear medicine) or in the assessment of an early healing response (CT).
The commonest location for the development of a spinal infection is the anterior vertebral body edge near the end plate. Bone marrow edema (high short tau inversion recovery [STIR], high T2-weighted fat-saturated, low T1-weighted signal) is the hallmark of spinal infection ( Figs. 66-1 to 66-3 ). In the early stages of infection, MR imaging sometimes only demonstrates an area of contrast enhancement with otherwise normal appearances, but this is rare. The area of edematous change increases in size and can involve the whole of the vertebral body. In pyogenic infection, there is often early involvement of the adjacent intervertebral disk, which shows edema-like signal pattern. Through the disk, the adjacent vertebral body is often also involved early in these cases. The infected intervertebral disk loses the low T2-weighted signal intranuclear cleft and displays a very high T2-weighted signal in its entire body. The disk height is usually reduced early but can sometimes appear widened due to erosion of the adjacent vertebral end plate. In pyogenic infection with proteolytic enzyme releasing pathogens, focal disk protrusion into the end plate is almost always seen. Contrast enhancement helps differentiate nonenhancing disk fragments from inflammatory tissue. It is important to realize that, as far as intervertebral disk is concerned, absence of contrast enhancement does not automatically equal fluid collection or abscess, because normal disk does not enhance. Diffuse contrast enhancement of the intervertebral disk was seen in only 20% of patients in one series. *


* References .
MR imaging is not particularly sensitive for demonstrating bony end-plate destruction. CT is better suited for this. Bone sclerosis, either preexisting or secondary to infection, with general reduction in signal intensity in all sequences can mask typical edema-like changes, and contrast agent administration can be of help in these cases.
In some cases, the edema-like bone marrow change remains contained within the vertebral body, which can cause diagnostic difficulties. The vertebral body can show four different MR patterns—diffuse bone marrow edema, a mixture of bone sclerosis and bone marrow edema, focal intravertebral abscess formation with bone marrow edema, and, finally, a pathologic fracture may be all that is seen. The commonest pathogen to cause only vertebral body involvement without disk involvement is tuberculosis, but this phenomenon can also occur in pyogenic infections. It is essential to image the whole of the vertebral column, in these cases, because multilevel involvement can be encountered. Similarly, it is important to always bear in mind, particularly in osteoporotic patients, that there is a risk that a fracture due to infection is misinterpreted as aseptic osteoporotic collapse.
If spinal infection is imaged very early when it is still restricted to part of the end plate, the diagnosis can be very difficult because the findings are virtually identical to Modic type I signal change. Diffusion-weighted imaging can assist due to differing apparent diffusion coefficients (ADCs) for infection and degeneration (see also discussion on diffusion-weighted MRI). In a research setting, iron oxide particles have helped discriminate between degenerative change and infection.
In other cases with adjacent end-plate changes, the intervertebral disk might demonstrate relatively high fluid signal (the so-called “white disk”). This sign should always raise suspicion.
If degenerative end-plate changes are present, the intervertebral disk virtually always demonstrates degenerative change and, therefore, low fluid signal. High fluid signal can be due to infection, and, in some instances, there are very minor end-plate changes at the time of disk involvement with infection.
In any case of unusual imaging findings or mismatch of imaging with clinical findings, the principal options are watch and wait, reimaging, or biopsy. Clearly, the clinical context is important. In the authors' practice, an unexplained incidental imaging finding is discussed in a clinical radiologic case conference. In the absence of clinical concern, the finding is either dismissed or, more frequently, further diagnostic imaging, such as CT or nuclear medicine or follow-up MRI, at a later date is arranged. If there is clinical concern, there is a very low threshold to biopsy.
Biopsies are usually taken under CT guidance. Even if there may be no correlating CT abnormality, careful correlation of anatomic features should enable to target any area of abnormality as demonstrated on MRI.
Infection of the spinal canal and the posterior elements is imaged most accurately by MRI. Epidural involvement in spinal infection is indicated by a decrease in T1-weighted signal intensity of epidural fat; increase in T2-weighted signal can be difficult to appreciate without fat suppression. STIR or fluid-attenuated inversion recovery imaging is more sensitive. Abnormal fluid collections usually demonstrate higher T1-weighted and lower T2-weighted signals than cerebrospinal fluid (CSF), but phlegmon as well as collections can show mixed signals in T1-weighted and T2-weighted imaging. The use of contrast agents allows reliable differentiation of phlegmon and collections. Collections show rim enhancement only, whereas phlegmon shows uniform contrast enhancement. Diffusion-weighted imaging also has been demonstrated to help in the diagnosis of collections. Collections exhibit markedly hyperintense signal against adjacent tissue and appear dark on ADC maps. When interpreting contrast enhancement within the spinal canal, it should always be remembered that the epidural vascular plexus normally shows contrast enhancement. This is particularly prominent in the cervical spine. In the differentiation of normal to abnormal contrast enhancement, assessment of symmetry (normally symmetric) and extension into intervertebral foramina (not seen normally) is of help. Epidural infection can occur on its own without involvement of other areas in the spine. The reported frequency of this ranges between rare and up to 40%. Meningitis can be diagnosed by observing abnormal contrast enhancement. If this is nodular or “shaggy,” it suggests granulomatous disease (including tuberculosis). Involvement of the spinal cord is indicated by increase in T2-weighted signal, by abnormal contrast enhancement, and, if severe, by vacuolization.
In cases of proven epidural involvement, the whole spine has to be imaged because there is often very extensive involvement of the spinal canal with areas of relative sparing. Epidural infection is associated with a poor prognosis if there is spinal canal stenosis by 50% or more, a craniocaudal extent of 3 cm or more, and if abscess formation is seen.
Infection of the posterior spine can occur as primary or secondary to infection of other parts of the spine. Primary infection is uncommon and more commonly seen with tuberculosis than with other infections. Overall, the same imaging criteria apply as in other areas of the spine.
Paravertebral involvement can occur as phlegmon, diffuse infection of tissue, or abscess, liquefaction of tissue. Phlegmon is indicated by edema-like signal and diffuse contrast enhancement; an abscess collection is indicated by fluid-like signal (high STIR, T2-weighted, low or intermediate T1-weighted signal, no contrast enhancement) and a thick, sometimes irregular, contrast enhancing rim. Intravertebral abscess formation has the same imaging characteristics as abscesses in other locations. Again, diffusion-weighted imaging can be of help in the diagnosis (see previous discussion).
Care must be taken to image paravertebral infection in its entirety because, otherwise, fistulae and tracking abscesses can be overlooked. In particular, involvement of the pelvis, peritoneum, perirenal space, pleura, pericardial, and retropharynx should be assessed.
As soon as a spinal infection has been diagnosed and treatment begun, there is no formed body of opinion as to the role of subsequent imaging in clinically uncomplicated cases. At the authors' institution, there is no routine follow-up in clinically uncomplicated cases. If imaging follow-up is performed, it is important to be aware of imaging pitfalls.
Even in patients responding well to treatment who go on to healing of their lesions, there is often an initial worsening of imaging appearances, the infection seems to spread, and there is often some progression of bony destruction. Persistence of abnormal imaging features was seen in a study of Kowalski and colleagues more than a month after the beginning of treatment, and this did not indicate treatment failure. The study concluded that, in uncomplicated cases, follow-up MRI is not indicated.
MR imaging is relatively insensitive for early healing response; early new bone formation, which is best appreciated in CT, is more suited for the assessment of early healing response. Regression of inflammatory change and reparative sclerosis of bone cortex and marrow with increasing bony consolidation can be seen on CT from 6 weeks after onset of infection (when successfully treated), whereas using MR imaging, these findings take about 12 weeks to diagnose with confidence.
MRI findings suggestive of healing are the decrease in contrast enhancement, reduction of edema and abscess size, and beginning normalization of the signal pattern, which is seen a few weeks to months after the initiation of treatment.
The absence of contrast enhancement and return of the spine to a normal signal pattern are both sure signs of complete healing of a spinal infection. However, the reverse is not true—persistence of contrast enhancement is not a sign of persisting infection but might be seen in healed spinal infection for a long time. Persistence of contrast enhancement in the intervertebral disk, as opposed to the vertebral body, is more common. The signal pattern of the bone marrow can revert to normal, but sclerosis and fibrosis can lead to low T1-weighted and T2-weighted signal patterns. If fatty marrow replacement occurs, high T1-weighted signal will be observed.
Bony fusion of vertebral bodies can occur after spinal infection and is identified by the continuity of bone marrow signal in the previous disk space.
Postoperative infections can be difficult to diagnose. An MRI that does not show inflammatory change can exclude infection; however, after surgery, contrast medium enhancement is very common and usually normal. There is edema-like signal and contrast enhancement seen in the area of previous surgery whether an infection is present or not. For a simple diskectomy, this normally is seen only in the surgical access route and not within the vertebral body. Postoperative Modic type I end-plate changes can occur and cause diagnostic difficulties. Intradiskal contrast medium enhancement after disk surgery is frequent and normal, and contrast enhancement due to infection is usually more amorphous. In postsurgery, there are frequently fluid collections seen. The majority of these will be due to harmless seromas, but CSF leaks and abscesses are in the differential diagnosis. Seromas usually have a thin, well-defined rim and show only minor, if any, contrast enhancement. CSF leaks show imaging features very similar to seromas. If hemosiderin deposition is seen (very low signal in gradient echo T2-weighted sequences), then a seroma is favored. Both collections often have T2-weighted signal intensities higher than those of CSF because there is no flow in these collections, and, therefore, no dephasing and signal loss occurs.
Surgical implants can cause artifact and make image interpretation more difficult or impossible. Implants can also generate signal change by their very function. For example, the implantation of epidural catheters for continuous epidural analgesia leads to signal changes very similar to those of infection. The epidural space shows decrease in T1-weighted signal, increase in T2-weighted signal, and avid contrast enhancement. The area of signal change frequently spreads along multiple vertebral bodies but can also be localized around the catheter tip. These findings are similar to those in catheter-related epidural infection with abscess formation, and, from imaging alone, the differential diagnosis is difficult.
Technical considerations for MR imaging of spinal infection are reasonably straightforward. Sagittal imaging should include edema-sensitive sequences, such as STIR or T2 fat-saturated images. If a reliable fat-saturation technique is not available (e.g., in low-field MR scanners), T2-weighted spin-echo imaging with repetition time greater than 2000 msec and echo time of 100 to 200 msec is advised. Fast spin-echo should not be used, in these cases, because edema may not be reliably diagnosed. Contrast enhancement is more clearly seen on T1 fat-saturated images. Abnormal areas should be assessed in sagittal and axial planes and, in particular, for axial imaging, an enlarged field of view may be necessary to demonstrate paraspinal involvement. Coronal imaging planes are not routinely necessary. There should be a low threshold for imaging the entire spine, if there are any indicators that a spinal infection is not strictly localized. Early synchronous or secondary involvement may be asymptomatic. If epidural infection is seen, then whole spine imaging with contrast enhancement is mandatory. Chemical shift artifact with pseudosparing of vertebral end plates of infected disks has been reported in the early years of MR imaging. This can be overcome by fat suppression or by changing the frequency encoding gradient to an anterior-posterior direction but is rarely a problem.
Diffusion-weighted imaging of spinal abnormalities can be used as an adjunctive technique in select cases. It has been pointed out that sometimes the imaging features of spinal infection and malignancy are very similar, and confident diagnosis is not possible. The imaging features of paraspinal abscesses are very similar to those in cerebral and hepatic abscesses, that is, hyperintense compared with adjacent tissue in diffusion-weighted imaging and low signal in the ADC map. Usually, the ADC of neoplastic lesions is significantly lower than that of infection. However, the measurements are not reliable to differentiate these two conditions reliably, and diagnosis of the type of infection is also not possible.
More recently, diffusion-weighted MRI has been found useful for the early diagnosis of spinal infection. Because infection often starts near the end plate, in early cases, differentiation from degenerative change, in particular, Modic type I, can be difficult. The ADC values for infection and degeneration-related edema-like signal change were found to be significantly different, allowing differentiation of these disease entities.
MRI is the imaging method of choice for spinal infection. Cost considerations may play a role, and MRI is not possible in all patients.
The only feature in favor of radiography is its almost universal availability. The problem with radiographs is the poor or absent sensitivity for any spinal infection other than destructive spondylodiskitis. Normal radiographs do not exclude a spinal infection. Life-threatening complications, such as epidural abscess formation, cannot be diagnosed with radiographs. Radiographs can play a role in monitoring complications, such as increase in bone destruction and instability, but cross-sectional imaging is much more specific and sensitive.
CT is well suited to assess bone response to spinal infection and can be performed under virtually any circumstances. Disadvantages, compared with MRI, are poor depiction of soft tissues and also the use of ionizing radiation.
Nuclear medicine techniques (including PET) offer reasonable sensitivity but poor specificity and poor anatomic detail. It can be of help in postoperative patients as MR imaging and CT are a struggle in these patients but still suffers from its limited specificity.
Ultrasonography does not play any significant role in the imaging of spinal infection.
There are no real controversies in the imaging of spinal infection. Some authors suggest that the infectious pathogen can be diagnosed with accuracy, but, although this may be the case for some, it certainly does not reflect the experience of the majority of the published literature, and the authors of this chapter cannot advise this approach.
The main caveats in imaging of spinal infection are to image the whole spine when spinal infection has been diagnosed so as to not miss epidural or other multilevel involvement. Postoperative infections can be very difficult to diagnose. Finally, it has to be made clear to any referring physician that normal radiographs do not exclude significant spinal infection.
Infection with M. tuberculosis is the most common granulomatous disease of the spine, and spinal tuberculosis accounts for half of all musculoskeletal tuberculosis cases. In developed countries, musculoskeletal tuberculosis in the indigenous population is uncommon and affects mainly the elderly and is thought to be due to reactivation of an old focus; however, it is not uncommon in immigrants of any age and in otherwise good health from high prevalence countries. In underdeveloped countries, children and young adults are particularly affected, and the disease tends to be more aggressive.
Tuberculous spinal infection usually presents with relatively mild symptoms and progresses slowly, often leading to a long delay before diagnosis. It has been reported that up to a third of patients with active tuberculosis have a normal CRP, making the diagnosis even harder. Spinal tuberculosis usually results from hematogenous spread from a focus in the lung or the genitourinary tract, although the primary focus is not always found.
The thoracolumbar junction or lumbar spine are most commonly affected. The frequency of involvement decreases from here to the thoracic, the cervical, and the sacral portions of the spine. More cranial parts of the spine are more frequently infected than in pyogenic infection, but this does not allow reliable differentiation.
Spinal tuberculosis typically starts in the well-vascularized anterolateral edge of a vertebral body. It can spread underneath the longitudinal ligaments to adjacent vertebral bodies. The stripping of periosteum and longitudinal ligaments can cause vascular compromise with avascular necrosis and subsequent vertebral body collapse. Central abscess formation within the vertebral body is relatively common in tuberculosis. Bone sclerosis is less common and florid than in pyogenic infection, but, in chronic cases, reactive new bone formation can be considerable.
Erosion of the vertebral body end plate can cause disk herniation into the vertebral body and loss of disk height without actual infection of the disk. The disks are often spared for a long time presumably because M. tuberculosis lacks proteolytic enzymes, but, eventually, the disk is involved in 75% of cases.
Large paravertebral abscesses are commonly seen in tuberculosis of the spine. They are often symmetric and tend to be larger than in pyogenic infections. Wall thickness and regularity have been suggested as the discriminating feature between pyogenic and tuberculous infection, but this is highly unreliable. Abscesses can track long distances, and sinuses are frequently seen in the groin, buttock, and chest but can occur virtually anywhere in the trunk. If calcified (difficult to appreciate on MR imaging), an abscess is very suggestive of tuberculosis; if an air-fluid level is seen, tuberculosis is virtually excluded (as long as there is no sinus to gas containing structures or the skin surface).
Vertebral body destruction is common in spinal tuberculosis (up to 73%), which makes spinal deformity with gibbus or vertebra plana and neurologic compromise more common than in other infections. Kyphotic deformities tend to be more severe in the thoracic spine compared to the thoracolumbar junction and the lumbar spine.
Neurologic compromise rarely occurs due to bony collapse alone. It is either due to associated subluxation/dislocation or, in the acute disease, to epidural involvement.
Involvement of the posterior elements is common in spinal tuberculosis and seen in greater than 40%. The relevance of this lies in the increased incidence of neurologic complications and the more difficult the differential diagnosis, especially against neoplasia. Isolated infection of the posterior elements is rare (<2%).
Paraspinal (78%) and epidural abscesses (68%) are more common than in other infections. Together with the bone changes, they result in neurologic compromise in 10% to 61%, and paraplegia occurs in about 10%.
After treatment, progression of destructive change is often seen and can last up to 14 months. This is significantly longer than in pyogenic infection. This means that the assessment of treatment success cannot be simply based on MR imaging. Decrease of bone marrow edema and contrast enhancement is usually regarded as evidence of healing. The differentiation of disease recurrence from secondary degenerative change after the primary infection can be similarly difficult. MR imaging will show decreased T1 signal, increased T2 signal, and contrast enhancement. If there is no signal increase in T2-weighted signal, recurrence of infection is unlikely.
The radiographic findings are largely nonspecific. The conventional teaching is that there is less reactive sclerosis of bone and that abscess calcification is more frequent than in pyogenic infections. In a recent review, it was suggested that the combination of radiographic lysis and sclerosis in conjunction with a suggestive clinical history is diagnostic of spinal tuberculosis and that further tests are not necessary in these circumstances. However, the authors of this chapter strongly advise against this approach and emphasize that any diagnosis should be based on clinical, laboratory, imaging, and histologic and microbiologic data.
The signal pattern of vertebral osteomyelitis due to tuberculosis is the same as in other infections or inflammation with edema-like signal, that is, signal decrease in T1-weighted and increase in T2-weighted images, although in the vertebral body, a mixed pattern can be seen in T1-weighted and T2-weighted images.
Attempts at pattern identification of spinal tuberculosis have been made. One classification proposes a pattern of initial osteitis with subsequent osteitis + abscess and subsequent osteitis + abscess + diskitis, whereas another describes a paradiskal pattern (metaphyseal involvement with erosion of end-plate and disk herniation into the end plate), an anterior pattern (stripping of periosteum, avascular necrosis, and vertebral body collapse), and a central pattern (involvement of whole vertebral body). The paradiskal pattern is seen in greater than 50% of adults and has significant loss of disk height, the anterior pattern, and more so the central pattern, leading to vertebral body collapse with deformity. Arachnoiditis, meningitis, and infection of the spinal cord occur more frequently in tuberculosis of the spine than other spinal infections. Often, there is no associated spondylitis. On MR imaging, the meninges show contrast enhancement, and the CSF shows increase in T1-weighted signal when involved. Other findings are CSF loculations, subarachnoid nodular contrast enhancing lesions, clumping of caudal nerve roots, and contrast enhancement of the nerve roots or cord. In cases of suspected tuberculous meningitis, the entire spine should be imaged, and, if suspected ,the brain should also be imaged.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here