Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Before cross-sectional imaging, the double-contrast enema was the foremost radiologic method for detection of colonic mucosal lesions and precancerous polyps. Diagnostic high-quality double-contrast barium enema examination is an art, requiring skillful maneuvering of the patient and barium pool while optimally using fluoroscopy. With the advent of computed tomography (CT), intramural as well as extraluminal extension of colonic diseases can be detected. This chapter discusses the principles and techniques for safe and accurate barium enema and review technical considerations for the performance of colorectal CT.
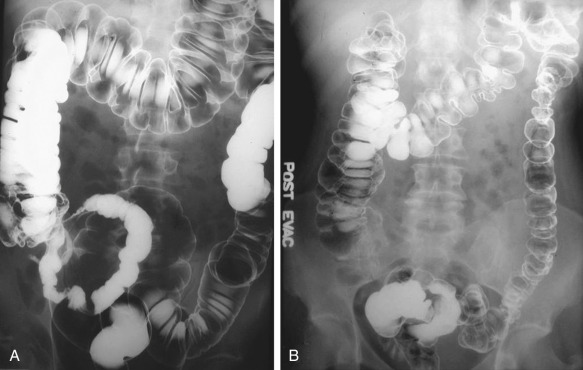
Single-contrast examination is preferred in immobile, elderly, or incontinent patients. The single-contrast examination is less sensitive than the double-contrast examination for detection of small polypoid lesions and evaluation of inflammatory bowel disease ( Figure 29-1 ). Double-contrast barium enema should be performed 1 week after a recent polypectomy, mucosal cautery, or large forceps biopsy to avoid the risk for colonic perforation.

Rigorous colonic cleansing is necessary for an optimal barium enema examination. Several colon cleansing regimens have been described.
A standard bowel preparation is outlined in Box 29-1 . Contraindications for the standard bowel preparation include bedridden patients, postoperative patients, patients with diabetes and hypothyroidism, and patients taking opiates.
On the day before the study:
Twenty-four hours of clear liquids for breakfast, lunch, and dinner
Plenty of liquids or water between meals to maintain hydration
Sixteen ounces of magnesium citrate at 5 pm
Four bisacodyl tablets at 8 pm
On the day of the examination: Nothing by mouth
Before starting the study, compliance with the bowel preparation should be confirmed. A preliminary abdominal radiograph can assess bowel preparation adequacy. The procedure may need to be rescheduled if there is significant colonic residue.
The patient lies in a recumbent, left side down position. Lubricant is applied on the external anal surface and the rectal catheter tip, and the catheter is gently inserted into the anal canal. Balloon insufflation is performed only in patients who are leaking barium or air out of the anal canal.
Rectal balloon inflation should be performed only after outlining the rectum with barium.
Contraindications for inflating rectal balloons include suspected colitis, a history of pelvic radiation or colitis, suspected rectovaginal fistula, and Crohn's disease.
The patient is placed prone and barium is slowly instilled. Once a full column has reached the descending colon, fully open the tube. The radiologist turns the patient 360 degrees to coat the colon. The patient is turned prone to advance the barium into the mid–transverse colon. The distal rectum is then drained by dropping the barium bag to the floor to avoid bubbles when air is insufflated.
Rapid distention of the rectum will cause sphincteric spasm at the rectosigmoid junction and increase the patient's urge to defecate.
Air is used to aid barium across the transverse colon into the ascending colon. The patient is turned right side down to fill the proximal transverse colon and then turned into the supine position to fill the posteriorly located hepatic flexure.
The enema tip can then be removed, providing physical relief to the patient and allowing better evaluation of the distal rectum. The enema tip may need to be left in place in patients expelling gas and who may need additional air to visualize the terminal ileum (e.g., patients with Crohn's disease).
Perform air insufflation only after barium has passed the splenic flexure.
Avoid rapid air insufflations and always turn the patient in different obliquities to redistribute air.
Complementary radiologic projections evaluate the colon. Twelve to 14 spot films and 4 to 5 overhead films are obtained. A routine sequence obtained in a double-contrast barium enema study is suggested in Table 29-1 ( Figure 29-2 ).
Sigmoid colon spot films are obtained before barium reaches the ascending colon. If barium refluxes through the ileocecal valve, the sigmoid colon may be partly obscured.
Obtain views without the enema tip to avoid missing distal rectal lesions.
Anterior cecal masses may need to be evaluated by spot films with the patient prone.
Applying compression in either the erect or recumbent, left posterior oblique position can aid visualization of the appendix and terminal ileum.
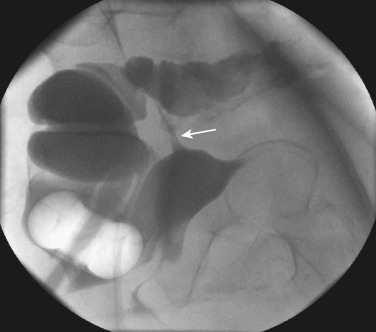
Postevacuation fluoroscopic films may be obtained with suspected fistulas or extraluminal diverticular collections.
| Spot Radiograph | Patient Position |
|---|---|
| Rectum (enema tip in) | Prone, left lateral |
| Rectum with air (enema tip out) | Supine, right lateral view |
| Proximal sigmoid colon | Left posterior oblique, prone |
| Distal sigmoid colon | Right posterior oblique, supine |
| Proximal descending colon | Erect |
| Distal descending colon | Recumbent right posterior oblique |
| Splenic flexure | Erect right posterior oblique |
| Hepatic flexure | Erect left posterior oblique |
| Proximal ascending colon | Prone or Trendelenburg left posterior oblique |
| Lateral wall of cecum | Supine, left posterior oblique |
| Medial wall of cecum | Supine, right posterior oblique |
| Remaining colonic segments | Supine |
| Overhead Radiograph | View |
| Rectosigmoid junction | Prone angled |
| Rectum | Left and right lateral decubitus cross-table view with horizontal beam |
| Rectum | Prone cross-table lateral views |
Some technical challenges during a double-contrast barium enema examination and plausible solutions are summarized in Box 29-2 .
Inexpensive
Very useful in small centers
Adequate mucosal surface information
Replaced in larger centers by colonoscopy and cross-sectional studies
Lacks information of the mucosal, submucosal layers and the mesentery
No extracolonic information
Results depend on technical expertise of operator
Residual barium in colon as a result of previous studies can pose difficulties in performance of future CT and MRI examinations
In patients with suspected colonic perforation or in postoperative patients, a water-soluble contrast agent can be used to look for fistulas or perforations ( Figure 29-3 ).
In cystic fibrosis patients, a hyperosmolar water-soluble molar contrast agent can liquefy the viscous stool by drawing fluid into the bowel.
Double-contrast examinations can be performed through a colostomy.
The pros and cons of a barium enema study are outlined in Table 29-2 .
| Problem | Implication | Solution |
|---|---|---|
| Poor bowel preparation | Simulates inflammatory bowel disease | Horizontal beam upright and lateral decubitus views; repeat study with preparation |
| Fecal residue | Simulates polyps | Found on dependent surface |
| Sigmoid diverticulosis | Difficult to detect polyps | Single-contrast examination of sigmoid |
| Patient incontinence | Leakage of air and barium | Intravenous glucagon prevents spasm; inflation of retention balloon |
| Nonfilling of right colon | Missed lesions | Postevacuation films; single-contrast study of right colon |
The most serious complication is colonic perforation, which can be both intraperitoneal and extraperitoneal and is usually seen in a diseased rectum secondary to inflation of rectal balloon. Air insufflations can cause abdominal discomfort and can be minimized by the use of carbon dioxide. Allergic reactions may be observed to barium, glucagon, or latex in gloves and rectal catheters. Transient bacteremia and septicemia are very rare complications of barium enema. Barium impaction can cause delayed complications with varying degrees of constipation and/or abdominal pain. Venous intravasation may result from barium breaching the colonic mucosa and is a feared complication because of its high mortality rate.
The continued use of the double-contrast barium enema for detecting colorectal polyps is controversial. Although the procedure is reimbursed by Medicare for colon screening, two large prospective clinical trials show the sensitivity of double-contrast barium enema examinations is approximately 50% for polyps measuring at least 10 mm in diameter.
The goal of the double-contrast barium enema is uniform coating of the mucosal surface with barium without formation of barium pools, which can obscure pathologic processes. It is important to be well versed with normal appearances and variations on a double-contrast study.
When the lumen is optimally distended, the normal mucosal folds are just effaced. Inadequate distention may conceal lesions, but overdistention can obscure lesions such as shallow ulcers.
The normal mucosal surface usually has a smooth, featureless appearance. En face, the mucosal surface fades from the white line of the contour to a smooth, gray-white surface. Potential anatomic features include the following:
Innominate grooves or areae colonicae: Seen as a fine network of lines and should not be mistaken for superficial ulceration
Transverse striations: Transient, secondary to contraction of the muscularis mucosa
Lymphoid follicles: May appear as a pattern of fine 1- to 3-mm nodules on the mucosal surface. Enlargement of these follicles may represent Crohn's disease, inflammation, and lymphoma.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here