Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Yeasts such as Malassezia and Candida albicans exist as commensals and form a normal part of the skin microbiome, where they cause minimal inflammation in the skin. Other fungi such as dermatophytes actively digest keratin and induce significant inflammation ( Chapter 32 ). Yeast infections are most commonly seen in situations where the host immune system is compromised (e.g. immunosuppressive treatment, HIV).
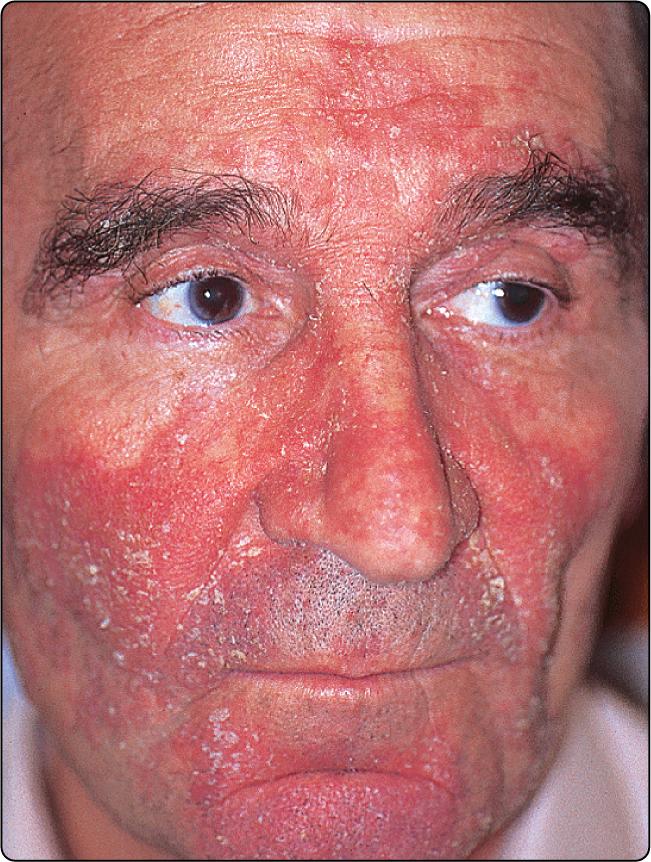
Seborrhoeic dermatitis is a chronic, red, scaly, inflammatory eruption usually affecting the scalp and face ( Table 33.1 ).
| Site of seborrhoeic dermatitis | Differential diagnosis |
|---|---|
| Face | Psoriasis, contact dermatitis, rosacea |
| Scalp | Psoriasis, fungal infection |
| Trunk | Psoriasis, pityriasis versicolor, fungal infection |
Sebum production is normal, but the eruption often occurs in the sebaceous gland areas of the scalp, face and chest. Endogenous and genetic factors and an overgrowth of the commensal yeast Malassezia (previously Pityrosporum ovale ) are involved. The condition is severe in some patients with HIV infection.
There are four common patterns:
Scalp and facial involvement. Excessive dandruff, with an itchy scaly erythematous eruption affecting the sides of the nose, scalp margin, eyebrows and ears ( Fig. 33.1 ). Blepharitis may occur. Most common in young adult males.
Petaloid. A dry, scaly patch of eczema over the presternal area.
P. folliculitis. An erythematous follicular eruption with papules or pustules over the back ( Fig. 33.2 ).

Flexural. Involvement of the axillae, groin and submammary areas by a moist intertrigo, often secondarily colonized by C. albicans. Seen in the elderly (do not confuse with the similarly named infantile eruption, p. 144).
The scalp lesions require the use of a medicated shampoo (e.g. containing coal tar, selenium sulphide or ketoconazole), either alone or following the application of 2% sulphur and 2% salicylic acid cream left on for several hours. Facial, truncal and flexural involvement responds to an imidazole or antimicrobial, often combined with 1% hydrocortisone, in a cream or ointment base. Oral itraconazole is also effective. Recurrence is common and repeated treatment often necessary.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here