Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
DNA viruses are frequently associated with vision-threatening complications, while RNA viruses usually cause more benign forms of conjunctivitis.
Adenovirus is the most common etiology of viral conjunctivitis.
Laboratory testing is rarely necessary for diagnosis; however, identification of the pathogen can be obtained by cell culture, polymerase chain reaction (PCR), and rapid diagnostic tests via antigen detection.
Few viral entities respond to topical antiviral therapy.
When inflammation is associated with the clinical findings, judicious use of antiinflammatories is acceptable as long as a herpes simplex virus (HSV) infection has been ruled out.
The key in viral conjunctivitis management is prevention of transmission and of complications.
Viral conjunctivitis is a common form of ocular morbidity. The severity of the disease may range considerably, and several viruses have been identified as causes. The differentiation of these causes is important, since therapy may not only be based on symptomatic relief but also may include antiviral and/or antiinflammatory drugs, the use of which requires a specific diagnosis.
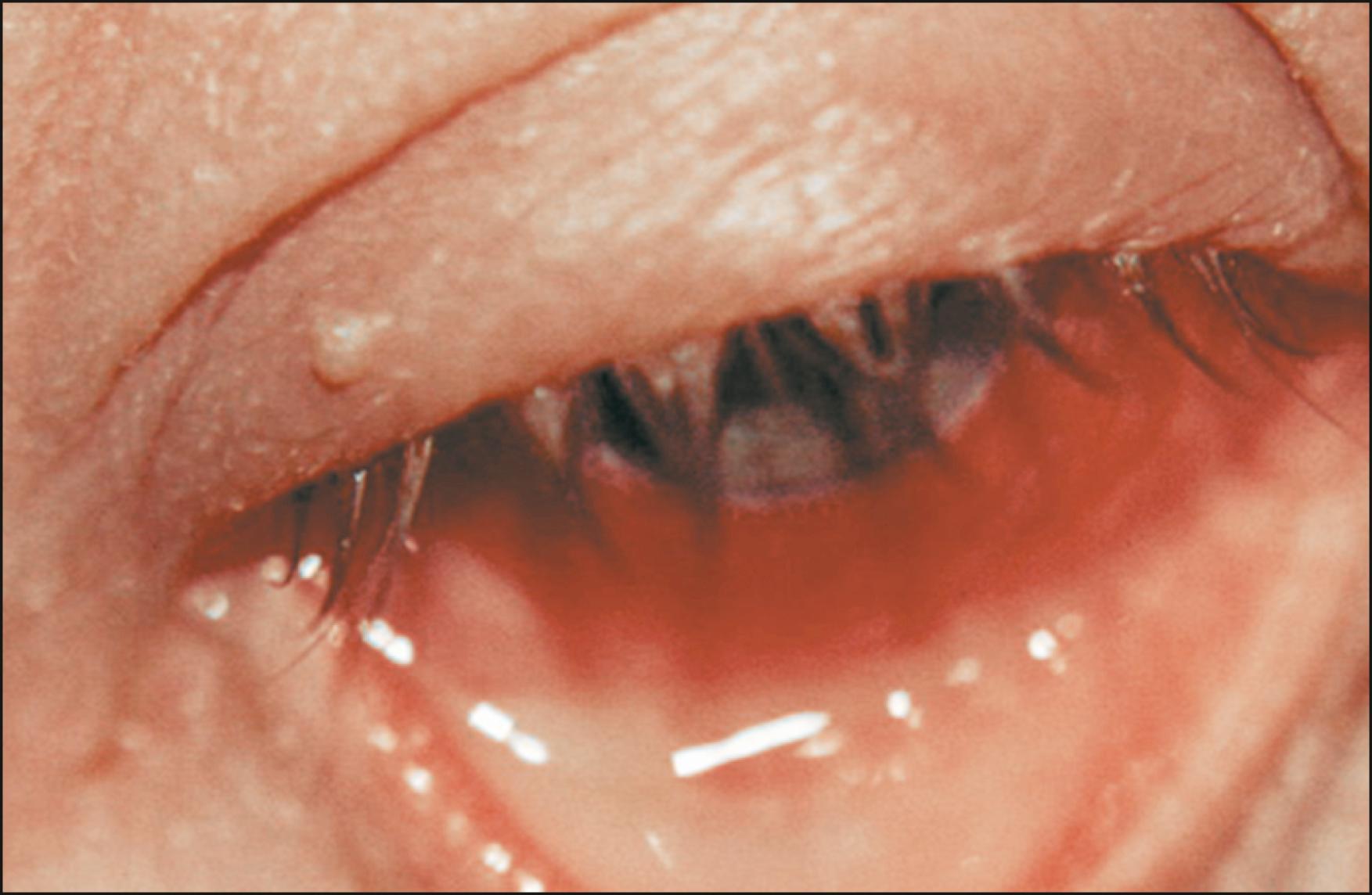
The clinical hallmark of most viral conjunctivitis is the follicular reaction of the conjunctiva, although this feature may also be present in chlamydial infection and toxic conjunctivitis as well. Follicles are the macro appearance of aggregates of lymphocytes surrounded by plasma and mast cells in the superficial conjunctival stroma of the conjunctiva ( Fig. 38.1 ). During the enlargement of the follicle, the cluster of immune cells displaces the blood vessels peripherally. As such, the biomicroscopic finding is a yellowish-white oval mound with dilated blood vessels in the periphery.
Both RNA- and DNA-containing viruses can infect the conjunctiva. The former usually cause more benign forms of conjunctivitis, while the latter are more frequently associated with vision-threatening forms of inflammation.
Adenoviruses (Ad) are the most common cause of viral conjunctivitis. Eighty-eight distinct human adenoviral serotypes have been described; these are classified into seven subgenera (A–G). , More than half of all adenoviral serotypes (57) belong to subgenus D. With few exceptions, most adenoviral conjunctivitis is caused by this subgenus. The application of restriction endonucleases and the analysis of cleavage patterns have led to the identification of different genotypes of a single serotype (e.g., eight different genotypes of adenovirus 8 have been described [Ad8A–Ad8H]).
Classically, ocular Ad infection is grouped into four different clinical presentations: (1) pharyngoconjunctival fever (PCF); (2) epidemic keratoconjunctivitis (EKC); (3) acute nonspecific follicular conjunctivitis; and (4) chronic keratoconjunctivitis.
PCF is characterized by pharyngitis, follicular conjunctivitis, fever, and preauricular and cervical adenopathy. Diarrhea and rhinitis are often associated symptoms. Ad 3, 4, and 7 are the causative agents in most reported cases, although Ad 1, 2, 5, and 14 have also been implicated. This highly infectious disease occurs in small outbreaks. It is transmissible by three routes: personal contact, fomites, or through insufficiently chlorinated swimming pools or ponds and lakes. PCF is one of the most common illnesses seen by physicians at children’s summer camps. The communicability is extremely high during the first several days and might last for 2 weeks after the onset of the symptoms.
The onset is acute, after 5–14 days of incubation. Most patients present with symptoms 6–9 days after exposure, especially when contaminated water is the source of infection. Pharyngitis varies from a mild sore throat to severe and painful inflammation causing difficult and painful swallowing. Examination of the posterior oropharynx reveals reddened mucosa without exudates. The pharyngitis as well as the fever may last up to 10 days. Lower respiratory tract infection, hepato- or splenomegaly, and rash are uncommon and may suggest a nonadenoviral etiology.
The ocular findings are often present at the onset of the disease. Initial symptoms vary in severity even within the same outbreak. PCF is most commonly bilateral, and the eyes may be affected simultaneously or in sequence up to 3 days apart. Normally, the second eye is clinically less severe. Initially, the patient complains of the abrupt onset of itching and irritation. The serous discharge may be abundant and often leads to crusting of the superior and inferior lashes, causing difficulty with opening the eyes on awakening. The hyperemia involves the entire conjunctiva but is more prominent in the inferior fornix. Mild punctate keratitis may be detectable by 2 days to 1 week after onset of symptoms. Minute punctate dots that stain poorly with rose Bengal and fluorescein are the initial finding. These dots may become diffuse and persist for up to a week. The subepithelial infiltrates (SEIs) typically seen in EKC are not frequent in patients with PCF. Most cases of PCF are self-limited, and complications are rare.
EKC is the severest ocular disease caused by adenoviruses. Ad 8, 19, 37, 53, 54, and 56 are the serotypes most commonly associated with EKC, but many other types have been documented. Mixed infection can occur. Ad 8 is the classic cause of EKC, and its clinical picture is the prototype of ocular changes induced by adenoviral disease. Transmissibility is high during the first days of symptoms, and hospital outbreaks are not uncommon. In communities with epidemics, the transmission occurs by contaminated fingers or objects, sexual contact, and swimming pool water. Instruments (such as tonometer tips) can also spread the disease, along with hand contact in the doctor’s office.
Ocular signs and symptoms are often more severe than those found in patients with PCF, but the two conditions may be indistinguishable on biomicroscopy. The absence of extraocular manifestations and severe stromal infiltrates in EKC are the differentiating features. EKC has a higher prevalence (up to half of patients) of unilateral disease when compared to PCF. Conjunctival involvement ranges from mild inflammation with diffuse hyperemia and a mixed follicular and papillary reaction (both more intense in the lower fornix) to a severe response with subconjunctival hemorrhages and intense inflammation. Pseudomembranes (inflammatory debris and fibrin) or true membranes ( Fig. 38.2 ) are a marker of severe conjunctival involvement. True membranes bleed when removed, and their presence makes the patient uncomfortable. Membranes can also rub against the cornea, causing mechanical, geographic ulcers that can mimic herpetic keratitis.
The initial corneal alteration in EKC can be detected as early as two days after the onset of the disease, as epithelial vesicle-like elevations of about 25–30 μm in diameter, hardly perceptible at the slit lamp, develop. By day 5, these elevations are easily visible both with and without fluorescein (the epithelial protrusions causing dark “holes” in the stained tear film). These findings are classified as stage 0 and stage I adenoviral keratitis, respectively. Histologic preparations of these focal lesions obtained at this stage have demonstrated scattered swollen cells and round or globular cells with various shapes and sizes, some fused to syncytia. These fused cells may exhibit necrosis and alterations in the cell surface. The next stage (II) persists for 2–5 days and is characterized by a coalescence of the lesions and involvement of the deep epithelium.
The incidence of stage 0–II keratitis ranges from as low as 13% to as high as 70% of patients with EKC. , This broad range is apparently related to the serotype as well as the genotype of the virus (e.g., Ad8H has a higher incidence of keratitis when compared to Ad8C and Ad8E). Marked worsening of photophobia, tearing, and discomfort heralds the presence of keratitis. The duration of the superficial keratitis is usually less than 2 weeks, but in Ad8 infections is typically longer (over 3 weeks) and with a higher incidence of both coarse lesions and progression to SEIs. The superficial keratitis may resolve or progress to SEIs in 43% of patients with EKC. In stage III, besides the deep epithelial punctate keratitis, faint SEIs just beneath the compromised areas of the epithelium are present ( Fig. 38.3 ). Stage III is typically detected during the second week. These infiltrates must be differentiated from immune-mediated SEIs as a manifestation of graft rejection. In the latter case, there is no conjunctivitis, and SEIs are limited to the donor.
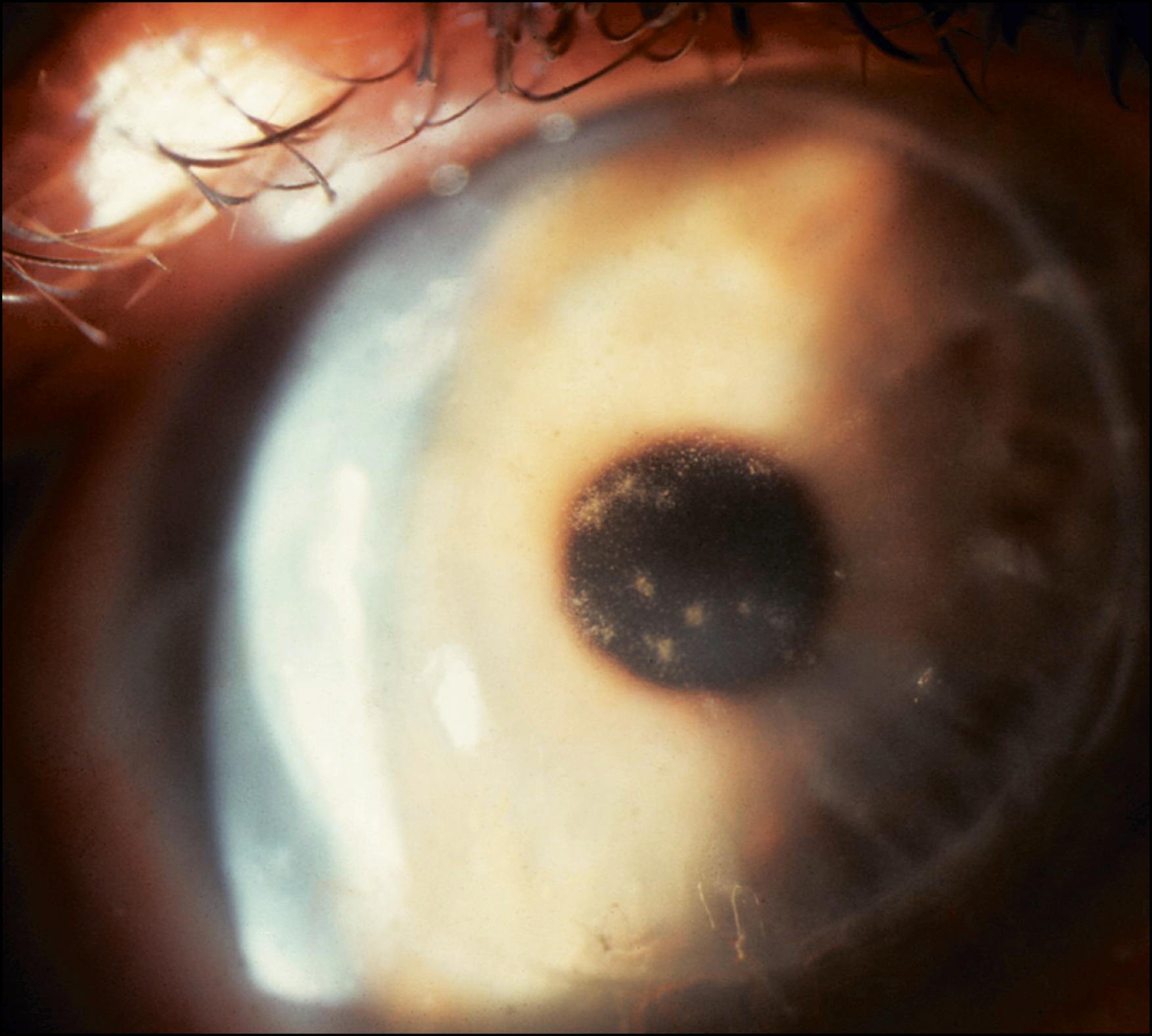
Stages IV and V are detected in or after the third week. No staining is seen. Stage IV is characterized by the classic SEIs that may be present for weeks or months after the infection ( Fig. 38.4 ). Stage V is characterized by punctate epithelial granularity, often overlying subepithelial opacities. The highest incidence of SEIs is associated with Ad 5 and 8. SEIs most commonly diminish with time; however, even with treatment, SEIs may cause photophobia and blurred vision for many months and, in some cases, may lead to visually significant scarring. SEIs are lymphocytic infiltrates in the superficial corneal stroma and the overlying (deep) epithelium and represent an immune reaction against Ad antigens.
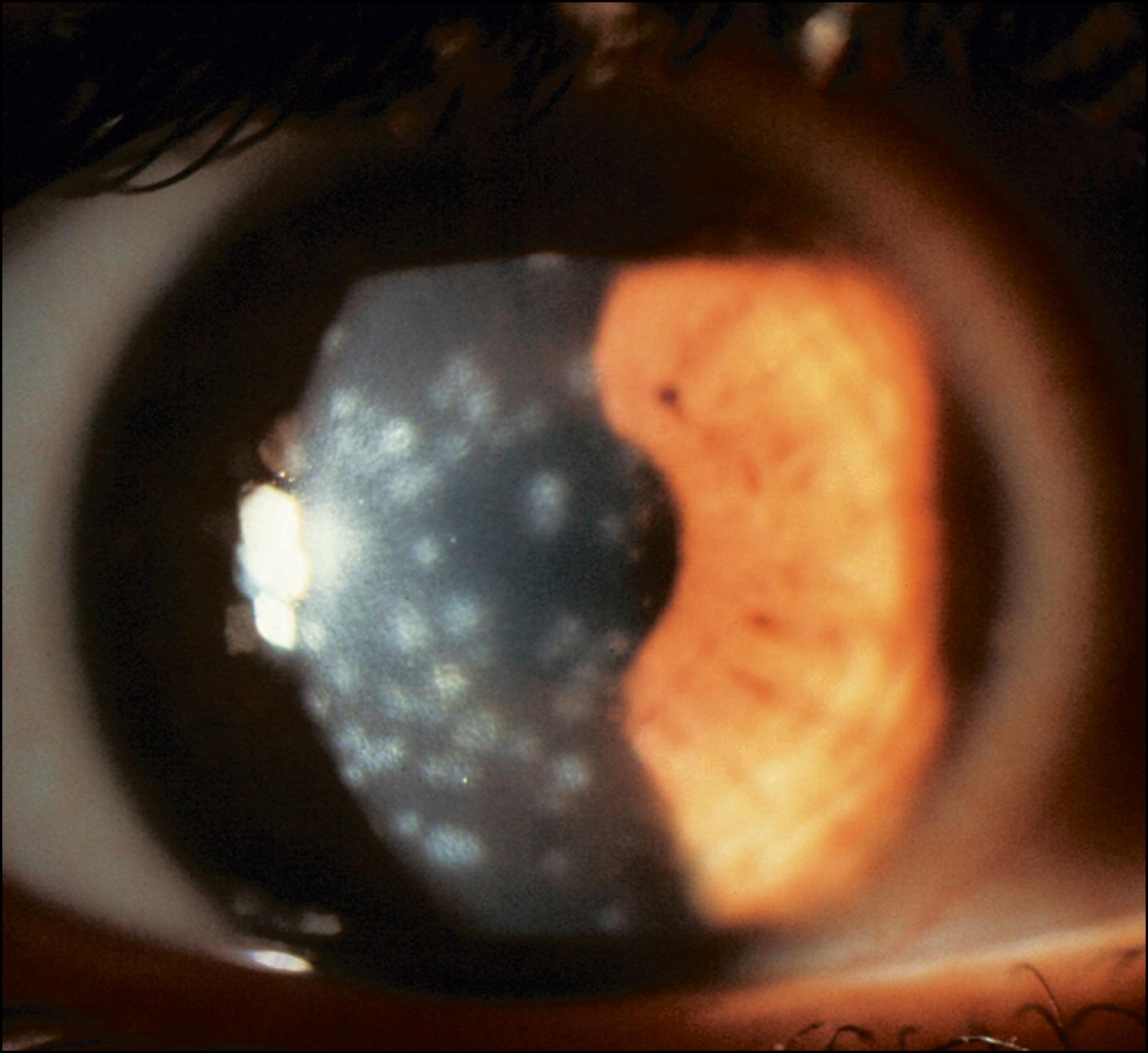
The keratitis is usually central, but the periphery can also be affected. Visual acuity is often diminished, especially when there is coalescence of the SEIs in the visual axis. These opacities may cause a decrease in contrast sensitivity and the presence of haloes and/or glare. Paracentral opacities may cause visual disturbances (haloes and/or glare) only in low-lit rooms and during the night, especially when driving. Quantifying the visual discomfort (interview, contrast sensitivity charts, visual acuity) is important when deciding whether or not treat the patient. Nevertheless, there is no standardization of any of these indices regarding eligibility for treatment.
Subconjunctival hemorrhage can be seen in the bulbar and palpebral conjunctiva. It has been described in 33.3% of patients with Ad8 infection, but the incidence is probably lower in infection from other serotypes.
Uveitis is a rare finding in adenovirus conjunctivitis and has been described only in patients with EKC and severe keratitis due to Ad8 infection. It is characterized by a mild flare and small numbers of cells in the aqueous humor of the anterior chamber. Resolution without complication within a few days is the rule.
Acute nonspecific follicular conjunctivitis may be caused by many serotypes of adenovirus, including those classically associated with PCF and EKC. The conjunctival involvement is milder, and keratitis is limited to the epithelium or, most commonly, is not present. Ocular signs are limited to a mild follicular reaction, mild conjunctival hyperemia, and discrete lid edema. Preauricular adenopathy may be present. The resolution of the signs and symptoms is usually more rapid than in PCF and EKC, and patients are often cured by the beginning of the third week. Some patients infected during an outbreak of EKC will present a mild disease compatible with nonspecific follicular conjunctivitis. The identification of these patients is important, because they might not seek medical assistance, and despite the benign presentation they can serve as a virus reservoir, spreading a not always benign disease in the community.
Chronic conjunctivitis is the least common form of adenovirus conjunctivitis. It was described in 1965 and has been reported infrequently. , Ad 2, 3, 4, and 5 have been isolated. The symptoms persist longer than expected for typical cases of adenoviral disease, and the virus can be recovered many months or years after the onset of symptoms. The conjunctivitis presents with intermittent bouts of ocular irritation with a waxing and waning superficial punctate epithelial keratitis and with SEIs. Both eyes can be affected, and the conjunctiva may present a follicular or a papillary reaction. Spontaneous resolution is the rule.
Adenovirus infection cases considered to be typical, on clinical grounds, are commonly treated without laboratory confirmation. The clinical diagnosis of viral conjunctivitis can be based on the presence of acute conjunctivitis and one of the following features: follicles on the inferior tarsal conjunctiva, preauricular lymphadenopathy, an associated upper respiratory infection, and a recent contact with a person with a red eye.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here