Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vestibular schwannomas (acoustic neuromas) are tumors arising from the Schwann cells of the eighth cranial nerve. They are typically slow-growing, benign tumors and malignant degeneration is rare. They are most commonly unilateral, resulting from a somatic mutation in a gene that encodes for the merlin protein on Chromosome 22, which is responsible for Schwann cell replication. In cases of bilateral vestibular schwannomas, the cause is almost invariably from neurofibromatosis type 2 (NF2). The causative gene mutation is the same as in unilateral tumors; however, NF2 results from a germline mutation that is present in all cells in the body. The true incidence of vestibular schwannoma is unknown although large epidemiologic studies have suggested an annual rate of 10.3 to 17.4 new cases per 1 million people. ,
The clinical presentation is varied and depends on the size and location of the tumor; however, progressive unilateral hearing loss is the most common presenting symptom leading to diagnosis. In a large retrospective study, 94% of patients presented with sensorineural high-frequency hearing loss. Tinnitus is the second most common symptom, seen in upwards of 80% of patients. Approximately 50% of patients will also present with disequilibrium or vertigo. Interestingly, headache is an uncommon complaint and is typically only seen when the tumor has grown to such a large size that it results in posterior fossa mass effect or obstructive hydrocephalus. Similarly, ataxia and cerebellar dysmetria are uncommon complaints and result from extracanalicular tumor compressing the brachium pontis or cerebellar hemisphere.
Prior to stereotactic radiosurgery, microsurgical excision was the only viable treatment. Depending on the location and size of the tumor, three operative approaches exist to the cerebellopontine angle. The middle fossa and retrosigmoid approaches can be hearing-sparing with the former used primarily for intracanalicular tumors while the latter is used for predominantly cisternal tumors. The translabyrinthine approach is typically reserved for patients with significantly reduced serviceable hearing. Radiosurgery provided patients with a wider range of therapeutic options with fewer risks and similarly durable results. These options include stereotactic radiosurgery or image-guided fractionated external beam radiation using linear accelerator generated photons, or protons.
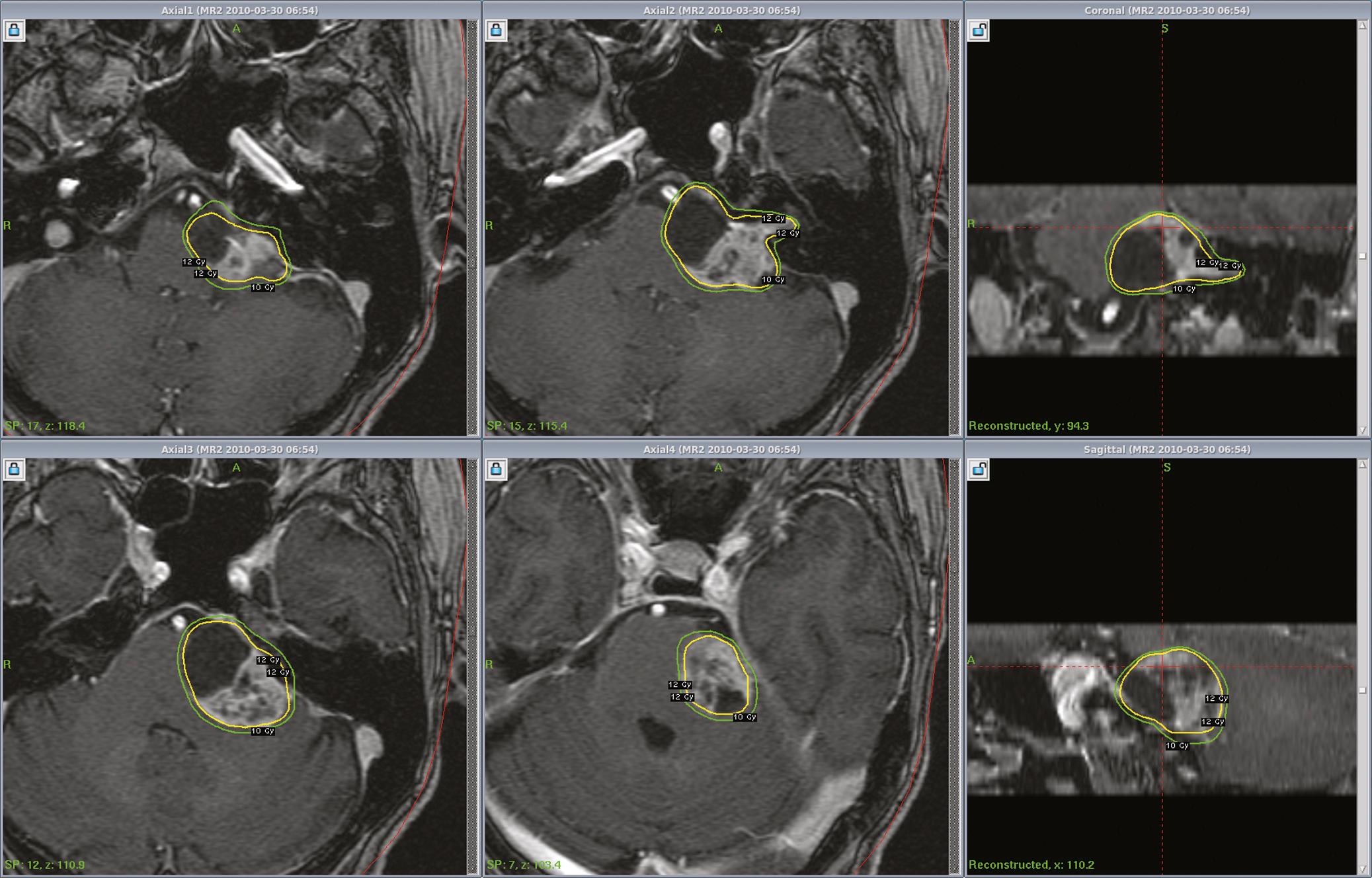
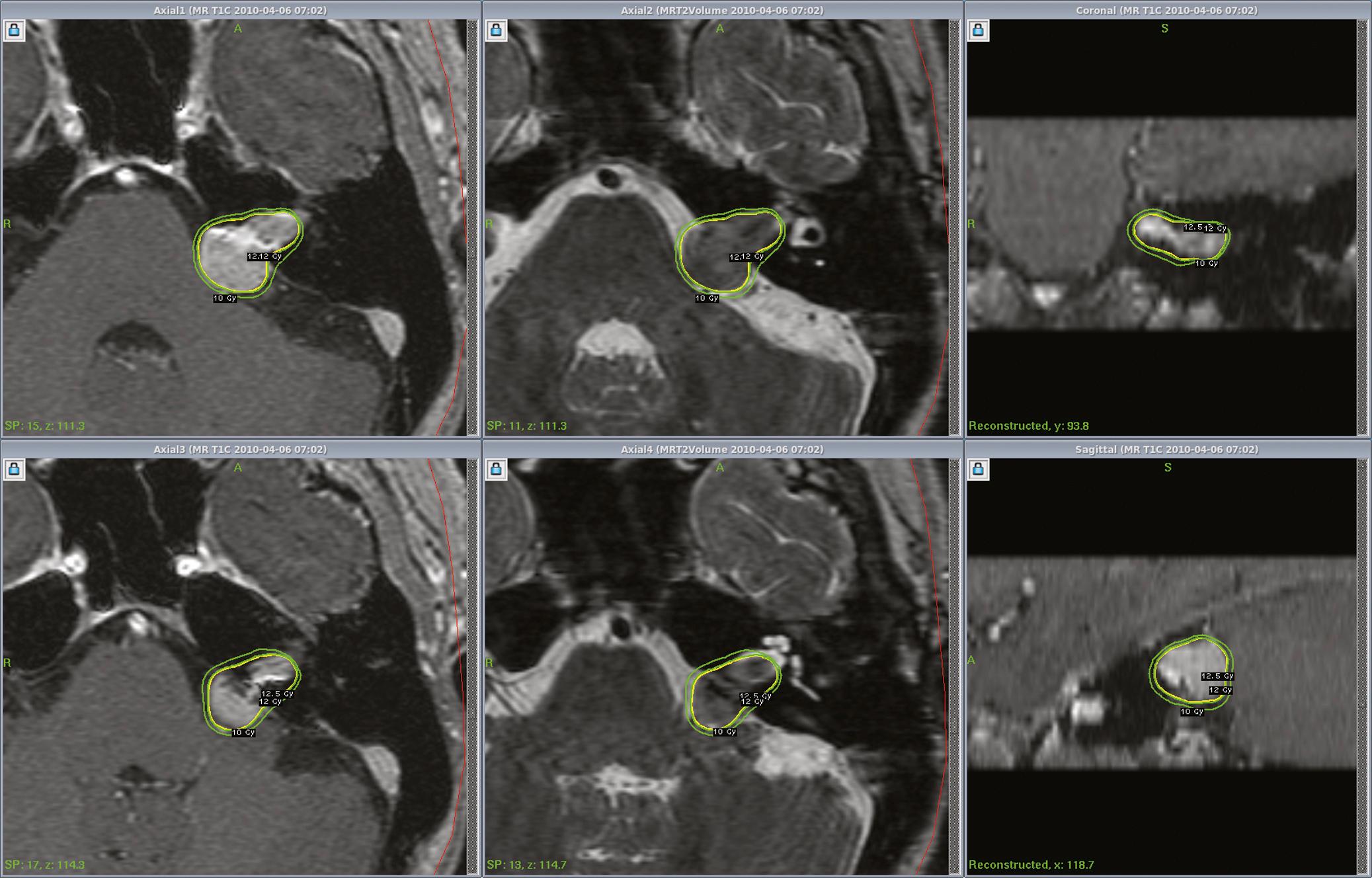
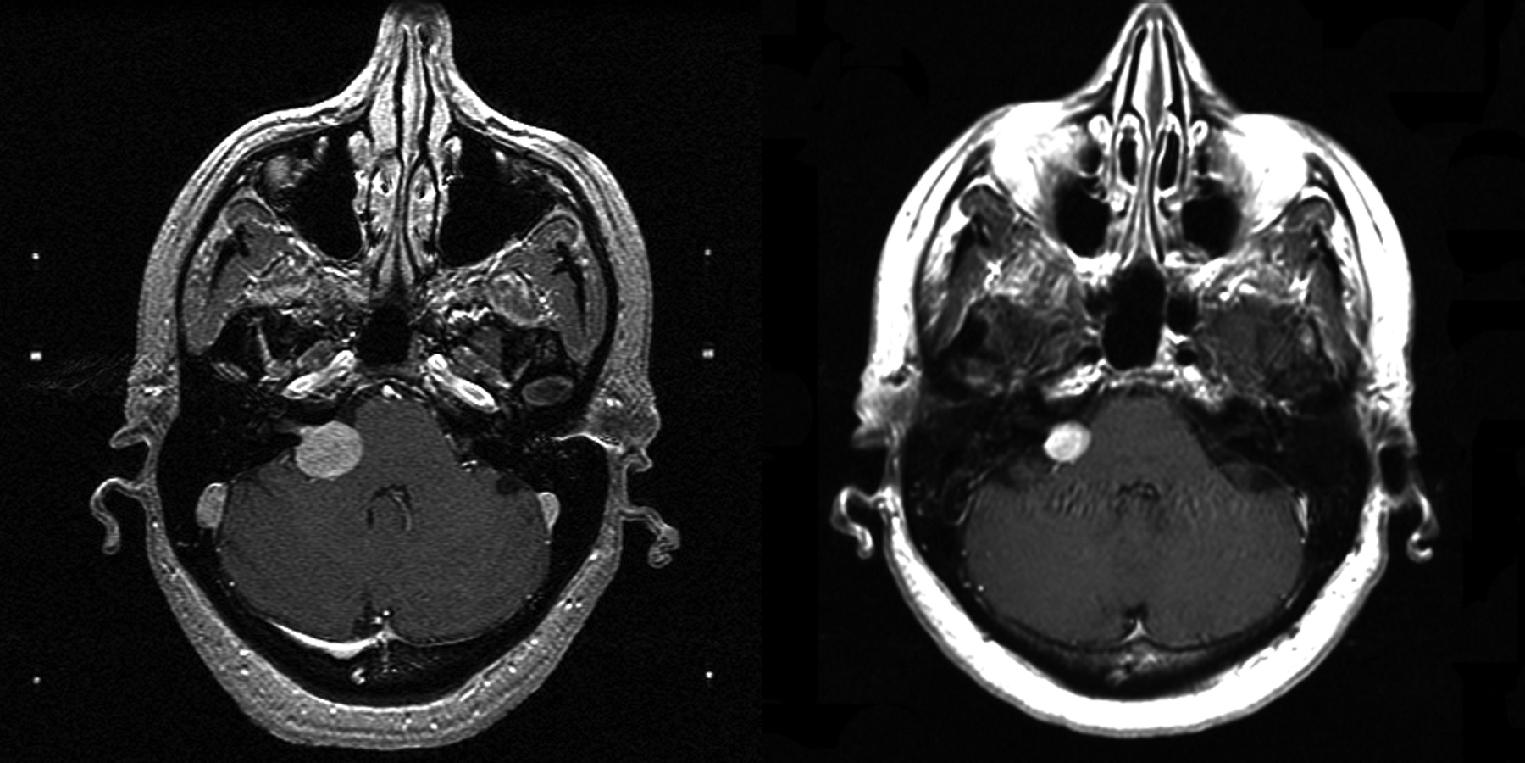
Vestibular schwannoma stereotactic radiosurgery using the Gamma Knife was first performed by Leksell in 1969. During the past decades radiosurgery has emerged as an effective alternative that is preferred by many patients and physicians for surgical removal of small to moderate-sized vestibular schwannomas ( Figs. 94.1 and 94.2 ). Long-term results have established radiosurgery as an important minimal access alternative to resection. Advanced multi-isocenter dose planning software, high-resolution MRI for targeting, dose optimization, and robotic delivery reflect the evolution of this technology. Other image-guided linear accelerator devices (Trilogy, Synergy S, Axesse, Novalis, X-Knife, TomoTherapy, Primatom, and CyberKnife) generally can be used to fractionate radiation delivery in 5 to 30 sessions. Proton beam technology is also used to deliver fractionated radiation therapy. The goals of vestibular schwannoma radiosurgery are to prevent further tumor growth, preserve neurologic function where possible, to avoid the risks associated with open resection, and improve preexisting symptoms.
Patients with vestibular schwannomas are evaluated with high-resolution MRI (CT may be substituted in patients who cannot undergo MRI scans) and audiological tests that include pure tone average (PTA) and speech discrimination score (SDS) measurements. Hearing is graded using the Gardner-Robertson modification of the Silverstein and Norell classification and/or the American Academy of Otolaryngology-Head and Neck Surgery guidelines, and facial nerve function is assessed according to the House-Brackmann grading system. “Serviceable” hearing (class I and II) is defined as a PTA or speech reception threshold lower than 50 dB and speech discrimination score better than 50%. The Committee on Hearing and Equilibrium of the American Academy of Otolaryngology-Head and Neck Surgery has established guidelines for reporting vestibular schwannoma results. In this classification hearing loss at a higher frequency (3000 Hz) is also included in calculating the PTA. “Serviceable” hearing (class A and B) is similar to class I and II of Gardner-Robertson hearing classes. Every patient is counseled about the options and risks and benefit of microsurgical and radiosurgical management strategies. Modern reports on vestibular schwannoma outcomes should include these data.
Radiosurgery can be performed using the Gamma Knife, modified LINACs, or the proton beam. Techniques of head frame fixation, stereotactic imaging, dose planning, and dose delivery are different for these three modalities. In Gamma Knife radiosurgery the procedure begins with rigid fixation of an MRI compatible Leksell stereotactic frame (model G, Elekta Instruments, Atlanta, GA) to the patient’s head. Local anesthetic scalp infiltration (5% Marcaine and 1% Xylocaine) is used, supplemented by mild intravenous sedation as needed. High-resolution images are acquired with a fiducial system attached to the stereotactic frame. For vestibular schwannoma radiosurgery, a three-dimensional (3-D) volume acquisition MRI using a gradient pulse sequence (divided into 1-mm slice intervals) is performed in order to cover the entire lesion and surrounding critical structures. A T2-weighted 3-D volume sequence (CISS or Fiesta) is performed to visualize cranial nerves and delineate inner ear structures (the cochlea and semicircular canals) ( Figs. 94.3 and 94.4 ). Planning is performed on narrow slice thickness axial MR images with coronal and sagittal reconstructions. Centers using LINAC or proton beam systems may use mask immobilization of the patient’s head along with image guidance and typically deliver the radiation dose in five or more fractions over many days. CT can be used for planning and should be coregistered accurately with MRI.
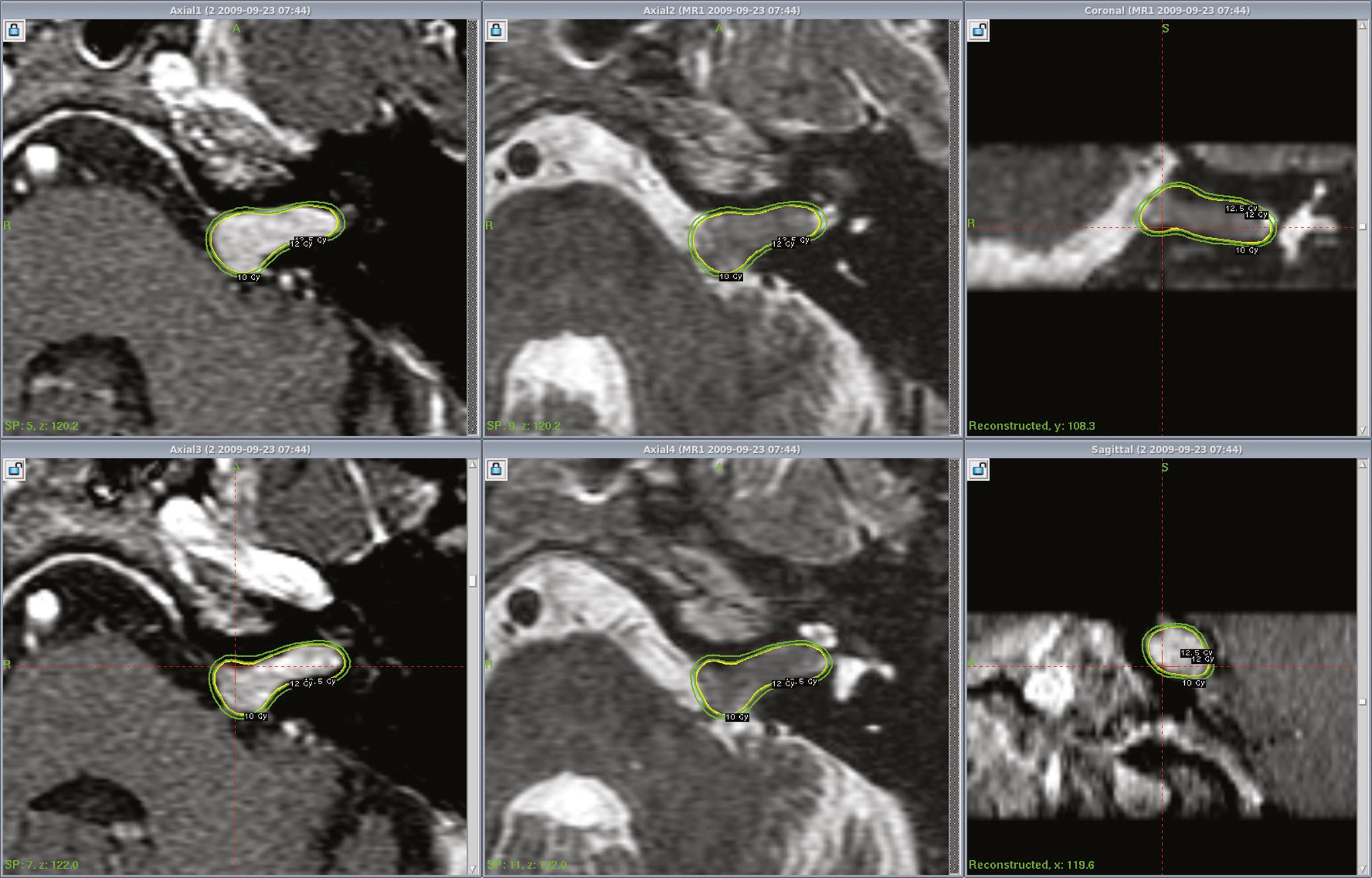
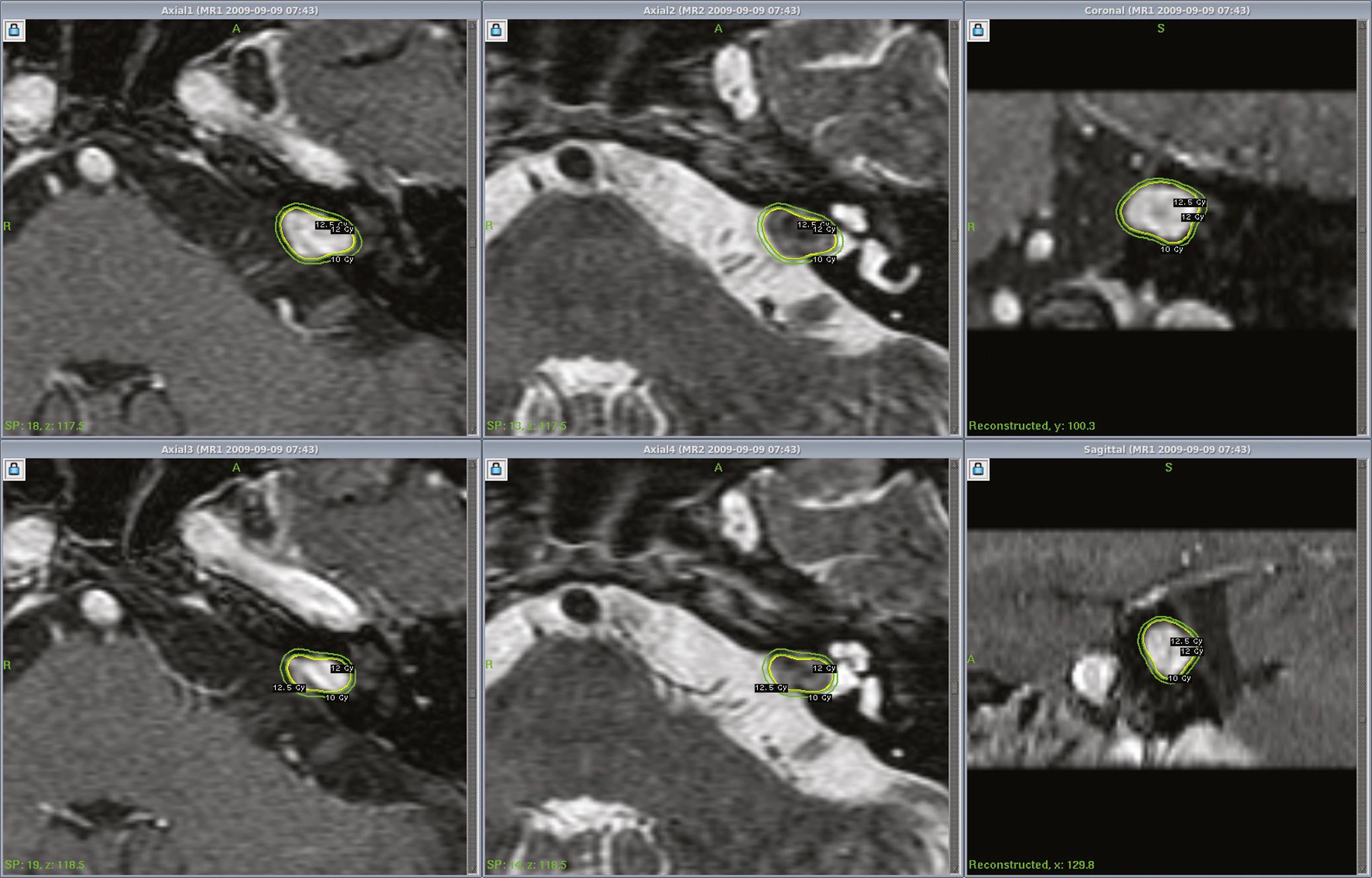
Dose planning is a critical aspect of radiosurgery. Optimal coverage of the tumor and preservation of facial, cochlear, and trigeminal nerve function is given priority during dose planning. For large tumors, preservation of brainstem function is also a consideration. Conformality and selectivity is necessary for hearing and facial nerve preservation. Specific Gamma Knife radiosurgery techniques include accurate definition of the tumor volume, use of multiple isocenters, beam weighting, and selective use of beam blocking to reduce dose to critical structures. Vestibular schwannoma planning is usually performed using a combination of small beam diameter (4- and 8-mm) collimators. For larger tumors, the 16mm collimator can be used. A series of 4-mm isocenters are used to create a tapered isodose plan to conform to the intracanalicular portion of the tumor.
After optimizing the plan, a maximum dose inside the target is determined as well as the dose to the tumor margin. The treatment isodose, maximum dose, and dose to the margin (edge) are jointly decided by a neurosurgeon, radiation oncologist, and medical physicist and, in some centers, a neurotologist. In Gamma Knife radiosurgery a dose of 12 to 13 Gy is typically prescribed to the 50% (or other) isodose line that conforms to the tumor margin. The most common dose is 12.5 Gy, used for hearing preservation in smaller tumors. Larger tumors may receive 12 Gy, and in those with hearing loss or prior resection, 13 Gy. Dose prescription for vestibular schwannomas changed significantly during the early 1990s. This current margin dose range is long established and is associated with a low complication rate and yet maintains a high rate of tumor control. We suspect that further dose reduction is unwarranted. However certain centers in Europe use a margin dose range of 11 to 12 Gy. Similar doses are also used for patients with bilateral (NF2-related) vestibular schwannomas and for patients with contralateral deafness from other causes, for whom hearing preservation is highly desirable.
After prescribing the margin dose, the mean dose to the cochlea, semicircular canals, and brainstem are assessed. A mean cochlear dose less than 4.2 Gy may be important for hearing preservation ( Fig. 94.5 ). The majority of the tumor volume is receiving a radiobiologic dose in excess of a biologically equivalent dose delivered by fractionated image-guided radiation therapy. The maximum precisely delivered radiosurgical dose of 25 Gy may be radiobiologically equivalent to 100 Gy of fractionated radiation. While many radiosurgical centers have evolved toward similar dose selection parameters, the doses and regimens chosen for fractionated radiotherapy continue to vary widely.
After radiosurgery, all patients are followed up with serial contrast enhanced gadolinium-enhanced MRI scans, which are generally requested at 6 months, 12 months, and 2, 4, 8, 12, 16, and 20 years. All patients who have detectable hearing before radiosurgery are requested to obtain audiological tests (PTA and SDS) near the time of their follow-up MRI.
Long-term results of Gamma Knife radiosurgery for vestibular schwannomas have been documented. Recent reports suggest a tumor control rate of 93% to 100% after radiosurgery. Kondziolka et al. studied 5- to 10-year outcomes in 162 vestibular schwannoma patients who had radiosurgery at the University of Pittsburgh. In this study a long-term 98% tumor control rate was reported. Sixty-two percent of tumors became smaller, 33% remained unchanged, and 6% became slightly larger. Some tumors initially enlarged 1 to 2 mm during the first 6 to 12 months after radiosurgery as they lost their central contrast enhancement. Such tumors generally regressed in volume compared to their pre-radiosurgery size. Only 2% of patients required tumor resection after radiosurgery. Norén, in his 28-year experience with vestibular schwannoma radiosurgery, reported a 95% long-term tumor control rate. Litvack et al. reported a 98% tumor control rate at a mean follow-up of 31 months after radiosurgery using a 12 Gy margin dose. Niranjan et al. analyzed the outcome of intracanalicular tumor radiosurgery performed at the University of Pittsburgh. All patients (100%) had imaging-documented tumor growth control. Lunsford et al. reviewed radiosurgery of 829 vestibular schwannomas and reported 97% tumor control rates at 10 years.
Flickinger et al. performed an outcome analysis of acoustic neuroma patients treated between August 1992 and August 1997 at the University of Pittsburgh. The actuarial 5-year clinical tumor control rate (no requirement for surgical intervention) was 99.4 + 0.6%. , The long-term (10- to 15-year) outcome of benign tumor radiosurgery also has been evaluated. In a study which included 157 patients with vestibular schwannomas , the median follow-up for the patients still living at the time of the study ( n = 136) was 10.2 years. Serial imaging studies after radiosurgery ( n = 157) showed a decrease in tumor size in 114 patients (73%), no change in 40 patients (25.5%), and an increase in three patients who later had resection (1.9%). No patient developed a radiation-associated malignant or benign tumor (defined as a histologically confirmed and distinct neoplasm arising in the initial radiation field after at least 2 years have passed). In patients under 40 years of age, with minimum 4-year follow-up, all remained employed and active.
Stereotactic radiosurgery can be a viable option for selected patients with larger vestibular schwannomas. Yang et al. retrospectively reviewed 65 patients with tumors between 3 and 4 cm in one extracanalicular maximum diameter treated with Gamma Knife surgery. At 6-month follow-up, 8% of tumors expanded, 82% were stable, and 11% were smaller. Two years later, 25% of tumors had more than 50% volume reduction, 35% had 10% to 50% volume reduction, 29% were stable, and 11% had volume increase. Eighteen of 22 patients (82%) with serviceable hearing before stereotactic radiosurgery (SRS) continued to have serviceable hearing after SRS more than 2 years later, and 5% of patients required VPS for hydrocephalus. A more recent study by Huang et al. found that ≥15 cm 3 was a significant factor predictive of Gamma Knife radiosurgery (GKRS) failure in a cohort of 35 patients but concluded that satisfactory management of tumors with a single dimension greater than 3 cm and a volume greater than 10 cm 3 can be achieved with GKRS.
A recent study surveyed quality of life (QOL) for patients who underwent GKRS for VS, assessing hearing status, tinnitus, imbalance, vertigo, as well as the Short-Form 36-item Health Questionaire. A total of 353 participants who underwent GKRS between 1997 and 2007 and found that vertigo and balance problems had the largest effect on scores, followed by nonuseful hearing. Overall satisfaction rates were 91% with their current overall level of functioning, and 975 noted they would recommend GKRS for their VS.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here