Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vasculitis refers to a group of inflammatory disorders that result in inflammation and necrosis of blood vessels with subsequent impairment of flow resulting in ischemia and infarction of distal tissues. , Often, vascular surgeons are the first physicians consulted in cases of vasculitis, and vasculitis should be considered in patients with ischemic occlusive disease or aneurysmal disease in the absence of traditional risk factors and in association with features of a systemic inflammatory process. Prompt involvement of a rheumatologist can expedite diagnostic testing and treatment. Vessels of any location may be affected by vasculitis, and the classification nomenclature has been defined by the International Chapel Hill Consensus Conference, as outlined in Table 138.1 .
| Nomenclature | Vasculitis | |
|---|---|---|
| Large-vessel vasculitis | Giant cell arteritis (also known as temporal arteritis) | |
| Takayasu arteritis | ||
| Medium-vessel vasculitis | Polyarteritis nodosa | |
| Kawasaki disease | ||
| Small-vessel vasculitis | Immune complex-mediated | Antiglomerular basement membrane (anti-GBM) disease |
| Cryoglobulinemic vasculitis | ||
| IgA vasculitis (Henoch–Schönlein purpura) | ||
| Hypocomplementemic urticarial vasculitis (anti-C1q vasculitis) | ||
| Antineutrophil cytoplasmic antibody-mediated (ANCA-associated pauci-immune) | Granulomatosis with polyangiitis (previously known as Wegener granulomatosis) | |
| Microscopic polyangiitis | ||
| Eosinophilic granulomatosis with polyangiitis (previously known as Churg–Strauss syndrome) | ||
| Variable-vessel vasculitis | Behçet disease | |
| Cogan syndrome | ||
| Thromboangiitis obliterans (Buerger disease) | ||
| Single-organ vasculitis | Cutaneous leukocytoclastic vasculitis | |
| Cutaneous arteritis | ||
| Primary central nervous system (CNS) vasculitis (isolated angiitis of the CNS) | ||
| Isolated aortitis | ||
| Others | ||
| Vasculitis associated with systemic disease | Lupus vasculitis | |
| Rheumatoid vasculitis | ||
| Sarcoid vasculitis | ||
| Others | ||
| Vasculitis secondary to other etiology | Hepatitis C-associated cryoglobulinemic vasculitis | |
| Hepatitis B-associated vasculitis | ||
| Syphilis-associated vasculitis | ||
| Drug-associated immune complex vasculitis (hypersensitivity vasculitis) | ||
| Cancer-associated vasculitis | ||
| Others | ||
There is no single presentation of vasculitis, but clinical manifestations often suggest the size of vessel affected and thus can help guide the likely diagnosis and necessary work-up. For example, patients with large-vessel vasculitis often present with limb claudication, vascular bruits, asymmetric blood pressures, or absence of pulses. Medium-vessel vasculitis often presents with cutaneous nodules and ulcers, livedo reticularis, digital gangrene, mononeuritis multiplex, and renovascular hypertension. In contrast, patients with small-vessel vasculitis tend to present with palpable purpura, pulmonary–renal syndromes (glomerulonephritis and alveolar hemorrhage), urticarial skin rashes, and scleritis.
The vasculitides typically cause characteristic histologic features, including infiltration of the vessel wall by neutrophils, mononuclear cells, and/or giant cells. Fibrinoid necrosis is seen with pan-mural destruction of the vessel wall and evidence of leukocytoclasis (disruption of leukocytes resulting in the histologic finding of “nuclear dust”). It should be noted that perivascular infiltration alone is a nonspecific histologic finding, which is not diagnostic of vasculitis.
Histologic findings in the specific diseases are dependent on the vessel size affected and the underlying disease physiology. Giant cell arteritis (GCA), Takayasu arteritis, and primary central nervous system (CNS) vasculitis are cell mediated, whereas polyarteritis nodosa (PAN), Henoch–Schönlein purpura, cryoglobulinemic vasculitis, and cutaneous leukocytoclastic angiitis are immune complex mediated. ANCA-associated vasculitis (AAV) involves both cellular and humoral immune responses and often involves granulomatous tissue injury without immune complex formation.
When tissue biopsy is not feasible, angiography imaging can be helpful for assessing specific types of arteritis. For example, angiography of the celiac trunk, superior mesenteric, and renal arteries can be diagnostic of PAN; imaging of the aortic arch is essential for the diagnosis of Takayasu arteritis and GCA with large-vessel involvement; angiography of the extremities can be helpful in the diagnosis of thromboangiitis obliterans (TO); and angiography of the cerebral circulation is essential for the diagnosis of primary CNS vasculitis. Angiographic findings that are characteristic of vasculitis include irregular asymmetrical tapering and narrowing as well as “beading” with segmental stenosis and aneurysm formation.
Noninvasive vascular imaging is used to evaluate some vascular beds, although it is somewhat controversial. In GCA, Doppler ultrasound of the temporal arteries has been shown to demonstrate inflammatory changes and can be used to assist with biopsy site selection; however, utility as a diagnostic tool is highly dependent on the experience of the sonographer; thus it should not replace temporal artery biopsy as a diagnostic tool. Magnetic resonance angiography of the aorta has utility in larger vascular beds and can be used to image the aorta in Takayasu arteritis and GCA. Aortic wall enhancement with gadolinium indicates active inflammation. Positron emission tomography (PET) has also been used to demonstrate enhancement in the aortic and subclavian vascular beds in Takayasu and GCA but has not gained widespread use as a diagnostic tool.
Takayasu arteritis is a cause of large-vessel vasculitis affecting the aorta and its branches that presents in younger individuals. It is discussed in Chapter 140 (Takayasu Arteritis).
GCA primarily affects patients over 50 years of age and is more common in Caucasian patients of Northern European descent. While relatively rare in African Americans, GCA has been reported in all racial groups; thus, patients of other races presenting with a consistent history should be fully evaluated. The incidence of GCA increases dramatically with age and is approximately 10 times more common in patients in their 80s than in patients aged 50 to 60. GCA is more common in women than men with a lifetime risk of 1% in women and 0.5% in men.
The exact cause of GCA is unknown. Genetic polymorphisms of the human leukocyte antigen class II region, specifically HLA-DRB1∗04 and DRB1∗01, are associated with susceptibility to GCA. Notably, the T-cell cytokine IFN-gamma is abundantly expressed in GCA but absent from arteries of polymyalgia rheumatica (PMR) patients without GCA. It is thought that in response to immunologic injury, the artery releases growth and angiogenic factors that induce proliferation of myofibroblasts, new vessel formation, and marked thickening of the arterial intima. This leads to vessel narrowing and occlusion resulting in symptoms of ischemia including jaw claudication, visual loss, and stroke.
GCA should be suspected in individuals over the age of 50 presenting with new-onset headache and evidence of systemic inflammation. Approximately 20% of GCA patients present with cranial symptoms, including headache, scalp tenderness, jaw and tongue claudication, diplopia, and blindness. New onset of diplopia in an elderly patient is highly suggestive of GCA. Jaw claudication is also a very specific symptom. PMR is also a common presentation, with 40% of cases presenting with complaints of symmetric pain and stiffness of the shoulder and thigh girdle muscles. It should be noted that some patients develop PMR without GCA and only 10% to 20% of patients presenting with PMR go on to develop GCA. In 20% of GCA cases, symptoms of both cranial GCA and PMR are present at presentation. GCA may also have a more indolent presentation with 15% of cases exhibiting fever and systemic symptoms with no other localizing symptoms. GCA is the cause in 15% of elderly patients with an FUO. Finally, around 5% of GCA cases present with claudication symptoms, cough, tenosynovitis, and the syndrome of relapsing seronegative symmetric synovitis with pitting edema can also occur.
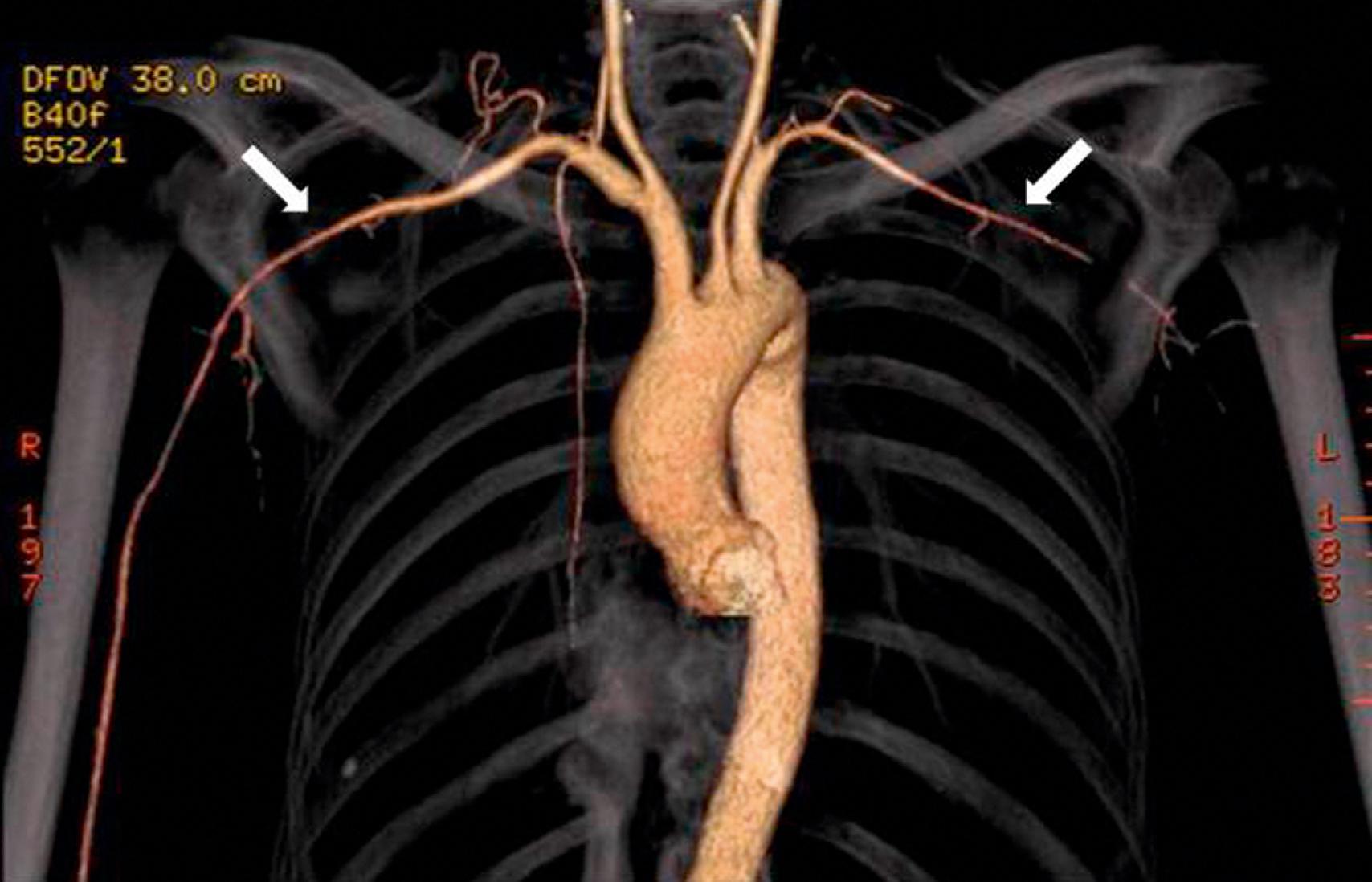
Physical findings in GCA include scalp tenderness and reduced pulse and tenderness of the temporal artery. Of GCA patients presenting with cranial and/or PMR symptoms, approximately 20% have clinical evidence of large-vessel vasculitis impacting subclavian arteries and other vascular territories ( Fig. 138.1 ); thus, it is important to check for discrepancies in blood pressure between the extremities, and the carotid and subclavian arteries should be auscultated for bruits. GCA patients have a 17-fold increased risk of development of thoracic aortic aneurysms and a 2.4-fold increased risk of developing abdominal aortic aneurysm compared to controls. Long-term monitoring with periodic imaging of the aorta is recommended.
Abrupt onset of painless blindness may occur as a result of ischemic optic neuritis in 15% of patients and this is usually related to arteritis of the posterior ciliary branches of the ophthalmic arteries. Amaurosis fugax is the strongest predictor for future blindness with a relative risk of 6.3. Thrombocytosis is also associated with visual loss. Patients may additionally complain of blurring of vision, iritis, conjunctivitis, scintillating scotoma, photophobia, glaucoma, and ophthalmoplegia from ischemia of extraocular muscles. Retinal and ophthalmic artery thromboses and occipital strokes are less common. It should be noted that risk of visual loss also drops significantly once steroids have been commenced, with less than 10% of patients developing blindness after steroids have been initiated.
Involvement of the intracranial vasculature in GCA is relatively rare, because these vessels lack an internal elastic lamina; however, involvement of internal carotids and vertebral arteries can occur and lead to strokes, seizures, acute hearing loss, vertigo, cerebral dysfunction, and depression.
The 1990 American College of Rheumatology criteria for the diagnosis of GCA are listed in Table 138.2 . For diagnosis of GCA, at least three out of five criteria must be present. The presence of three or more criteria yields a sensitivity of 93.5% and specificity of 91.2% for distinguishing GCA from other forms of vasculitis. While the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are often markedly elevated in GCA, only a minority of patients have a normal ESR. Often, patients will have other evidence of systemic immune response, including normocytic anemia and elevated platelet count (see Table 138.2 ).
| Criterion | Definition |
|---|---|
| Age at disease onset >50 years | Development of symptoms or findings beginning at age 50 or older |
| New headache | New onset headache |
| Temporal artery abnormality | Temporal artery tenderness to palpation or decreased pulsation without evidence of arteriosclerosis of cervical arteries |
| Elevated erythrocyte sedimentation rate (ESR) | ESR >50 mm/h by Westergren method |
| Abnormal artery biopsy | Biopsy specimen showing vasculitis characterized by predominance of mononuclear cell infiltration or granulomatous inflammation, usually with multinucleated giant cells |
The gold standard diagnostic test for GCA is temporal artery biopsy. An adequate length of temporal artery (2–3 cm) should be obtained at biopsy, and bilateral biopsies (particularly if the first is negative) are recommended by some groups. Up to 50% of biopsies show diffuse lymphocytic infiltrate without evidence of granulomatous inflammation or giant cells. Fragmentation and fraying of the internal elastic lamina can be seen in normal aging, so in the absence of inflammation, this finding is not diagnostic of GCA. Ideally, biopsy specimens should be obtained prior to or within 7 days of starting corticosteroids. However, corticosteroid therapy does not normalize the affected artery; it simply reduces the inflammatory infiltrate, so “healed temporal arteritis” can still be diagnosed by the presence of intimal fibrosis, medial scarring, and asymmetric destruction of the internal elastic lamina.
Large-vessel involvement may be assessed using conventional angiography, magnetic resonance angiography, or computed tomography (CT) angiography. , , Newer imaging modalities including ultrasound and PET are being evaluated as diagnostic tools in GCA.
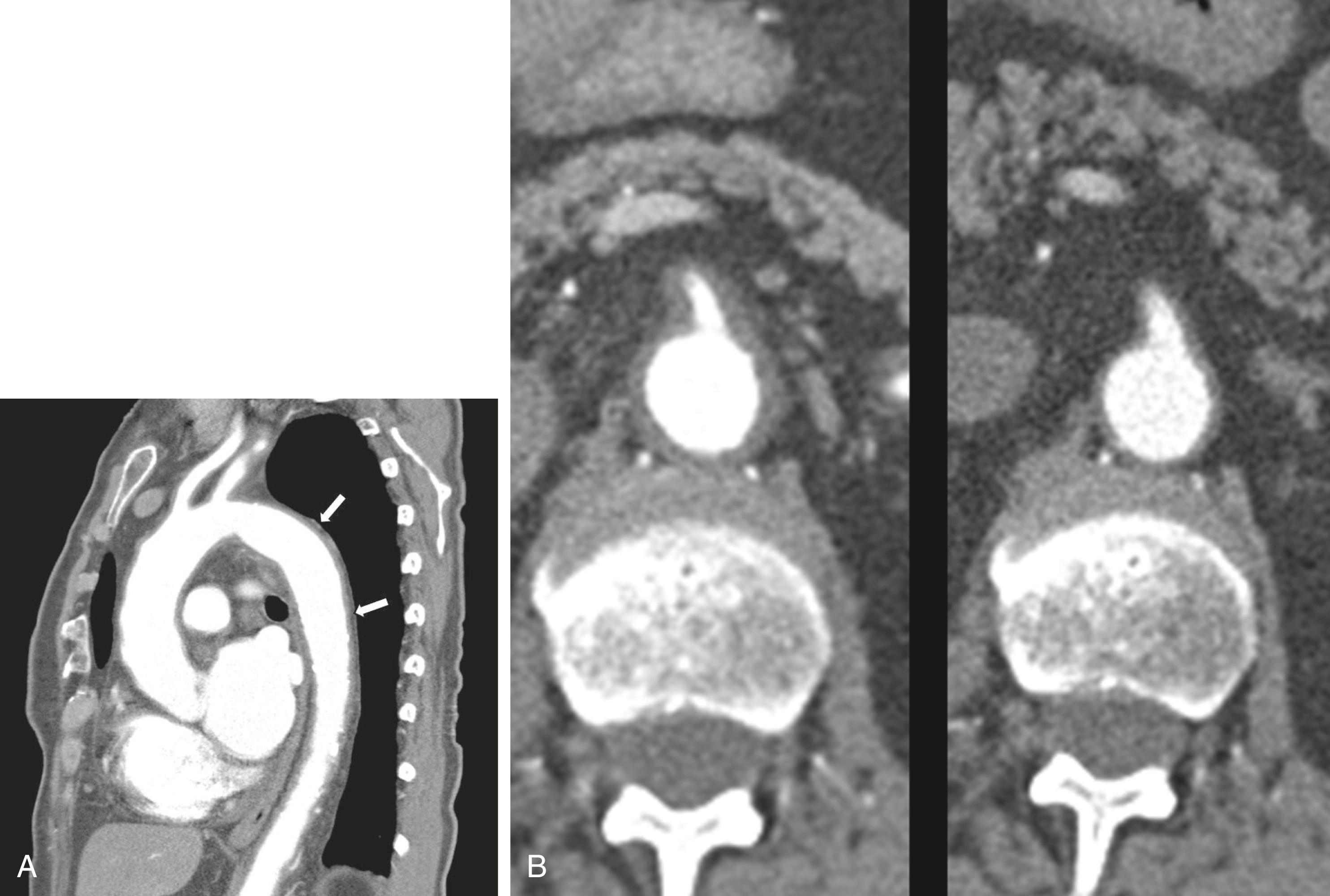
Corticosteroid therapy is standard of care in the management of GCA, and the initial dosing should be 40 to 60 mg daily. In patients with incipient visual loss, intravenous methylprednisolone (1000 mg per day for 3 days) may be considered. The initial prednisone dose should be maintained until inflammatory markers normalize (usually at least 1 month). Various tapering methods are used, but a rule of thumb is to reduce the prednisone by 5 mg every 1 to 2 weeks until 30 mg per day is reached and then to reduce the amount by 2.5 mg every 1 to 2 weeks until 15 mg per day. The subsequent taper should be 2.5 mg every 4 weeks until 10 mg and then 1 mg every 4 weeks until the patient is off prednisone. Alternate-day steroid dosing regimens are not effective. Clinical symptoms, ESR, and CRP should be monitored for every change in dose, and it should be noted that spontaneous recurrence may occur in as many as 50% of cases. Up to 40% of cases (especially women) need long-term corticosteroid therapy for several years. All patients are recommended to also receive low-dose aspirin 81 mg per day to reduce the risk of cardiovascular events and blindness. The anti-IL6 antibody tocilizumab has recently been shown to be effective as a steroid-sparing agent in GCA. Other trials of biologic and nonbiologic disease-modifying antirheumatic drugs (DMARDs) are ongoing. Figure 138.2 shows marked improvement in diffuse arterial wall thickening caused by GCA in response to steroids.
Revascularization procedures are rarely required in GCA due to development of collaterals. Balloon angioplasty in combination with immunosuppressive treatment has been tried in small case series, but unless the inflammatory process is well controlled, the risk of restenosis is high. For patients with aortic aneurysms, surgery is indicated with surgical results similar to those seen in patients with aneurysms from other etiologies.
Inflammation of the aorta discovered incidentally on histology is seen in 3% to 10% of surgical aortic aneurysm repairs. A recorded 45 cases of incidental aortitis in a retrospective review of 514 ascending aortic specimens (frequency 8.8%). In the thoracic aorta, some of these lesions are histologically indistinguishable from GCA, but others demonstrate lymphoplasmacytic infiltrate, and 75% of these are due to IgG4-related disease. In the abdominal aortal, lesions can be grouped into idiopathic retroperitoneal fibrosis (Ormond disease) and inflammatory aortic aneurysms that are often associated with smoking and a family history of aortic aneurysm, of which some of these lesions are due to IgG4-related systemic disease. The syndrome of idiopathic abdominal peri-aortitis has also been described without associated aneurysm or retroperitoneal fibrosis. In these patients, rarer etiologies including Erdheim–Chester disease should be considered.
Idiopathic retroperitoneal fibrosis is rare, affects men more than women (3:1), and presents in patients in middle age (40–60 years old). Typically, patients present with pain in the lower back, abdomen, flank, and scrotum. Some patients also demonstrate systemic symptoms including fever, anorexia, and malaise. Patients have hypertension in 75% of cases and lower extremity edema and phlebitis can be seen. Serologic work-up is usually negative, but inflammatory markers are elevated in 75% of cases. Classic CT findings include presence of a homogeneous mass around the aorta following the iliac bifurcation with associated medial deviation of the mid-part of the ureter and secondary hydronephrosis. Usually, lymphadenopathy is absent. Biopsy may be performed laparoscopically or through open procedure, and histology shows sclerosis with infiltration of mononuclear cells. The pathophysiology of this process is unknown, but an exaggerated local inflammatory response to oxidized low-density lipoprotein in aortic plaque has been postulated. Treatment with high-dose prednisone is recommended (60 mg daily for 1 month followed by tapering off to 10 mg/day by 3–6 months). Maintenance therapy with prednisone is recommended for 1 to 3 years. The disease recurs in 10% to 30%, and use of mycophenolate mofetil, tamoxifen, or methotrexate should be considered for these patients. Monitoring with inflammatory markers and CT scan should be continued every 3 months while on treatment and every 6 months when off treatment.
IgG4-related systemic disease affects older males, with 60% to 80% of cases affecting patients older than 50 years. Often, there is a past medical history of allergic diseases and atopy (eczema and asthma). Patients develop tumor-like lesions in one or more organs and on biopsy dense lymphoplasmacytic infiltrates with storiform fibrosis and obliterative phlebitis are seen. Lesions should be stained to demonstrate IgG4 positive cells (with >30 per high-powered field and IgG4/IgG positive ratio >50% confirming the diagnosis). Elevated serum IgG4 is seen in 60% to 80% of cases but is not always detected. Serologic work-up is usually negative. Several organs may be affected simultaneously, with the most common presentations being type I autoimmune pancreatitis, sclerosing cholangitis, salivary gland involvement (Mikulicz disease), and sclerosing sialadenitis (Kuttner tumor). The disease may be associated with chronic lymphoplasmacytic aortitis and aneurysm formation. This more commonly affects the thoracic than abdominal aorta and can be mistaken for idiopathic retroperitoneal fibrosis. Treatment for IgG4-related disease includes high-dose steroids along with DMARDs; in recent years, rituximab (a monoclonal antibody targeting B cells) has been shown to be effective.
Erdheim–Chester disease is a rare histiocytic disease that is associated with periaortic fibrosis (referred to as “coated aorta”), periarterial infiltration of coronary arteries, and pericardial thickening and effusion. Retroperitoneal involvement may also manifest with mass-like infiltrative lesion or with perinephric changes known as “hairy kidney.” It may be confused with idiopathic retroperitoneal fibrosis and IgG4-related disease, but the distinguishing feature is that most patients also have bone lesions, often in the lower extremities that present with juxta-articular pain. Biopsy of involved tissue reveals tissue infiltration by sheets of foamy histiocytes interspersed with inflammatory and multinucleated giant cells. In recent years, it has become clear that the disease is associated with gain-of-function mutations in the proto-oncogene BRAF (the BRAFV600E mutation), and treatment with BRAF inhibitors has been found to be effective with less toxicity than prior treatment options such as interferon.
PAN is a necrotizing vasculitis of small and medium arteries and is characterized by the absence of glomerulonephritis and absence of antineutrophil cytoplasmic (ANCA) antibodies.
Diagnosis is based on presence of 3 out of the 10 American College of Rheumatology criteria ( Table 138.3 ).
| Criterion | Definition |
|---|---|
| Weight loss >4 kg | Loss of at least 4 kg since illness began without dieting or other confounding factors |
| Livedo reticularis | Mottled reticular pattern over the skin of extremities or torso |
| Testicular pain or tenderness | Pain or tenderness of the testicles not due to infection, trauma, or other causes. |
| Myalgias, weakness or leg tenderness | Diffuse myalgias or weakness of muscles, tenderness of leg muscles. |
| Mononeuropathy or polyneuropathy | Development of mononeuropathy, multiple mononeuropathies, or polyneuropathy |
| Diastolic BP >90 | Development of hypertension with diastolic BP >90 mm Hg |
| Elevated BUN or creatinine | Elevation of BUN >40 mg/dL or creatinine >1.5 mg/dL |
| Hepatitis B infection | Presence of hepatitis B surface antigen or antibody in serum |
| Arteriographic abnormality | Arteriogram showing aneurysms or occlusions of visceral arteries not due to arteriosclerosis, fibromuscular dysplasia, or noninflammatory causes. |
| Biopsy of small or medium-sized artery demonstrating polymorphonuclear neutrophils | Histologic changes showing presence of granulocytes, and/or mononuclear leukocytes in vessel wall. |
PAN may be idiopathic or secondary to hepatitis B infection. In hepatitis B-associated PAN, the mean time between hepatitis diagnosis and PAN is 7 months. PAN may also be associated with other viral infections including HIV and has been seen as a paraneoplastic manifestation of hematology malignancy (particularly hairy-cell leukemia).
The histologic lesion in PAN is a focal, segmental necrotizing vasculitis affecting medium-sized arteries. It commonly affects arterioles with sparing of large vessels and veins. The arterial wall inflammation is characterized by fibrinoid necrosis of the media along with neutrophilic and lymphocytic infiltrate. Active necrotizing lesions are often seen alongside healed and fibrotic lesions. Localized thromboses may occur at the site of inflammatory injury, and arterial aneurysms may form as a result of weakening of the vessel wall by the inflammatory process, ultimately leading to end-organ injury from ischemia, infarct, and hemorrhage.
There are no diagnostic serologic tests for PAN. Elevated systemic inflammatory markers are common, and patients may also exhibit normocytic anemia and thrombocytosis. Usually, complement levels are normal. Hepatitis B serology should be tested, and patients with hepatitis B-associated PAN demonstrate hepatitis B surface antigen positivity, HBeAg, and positive PCR for hepatitis B virus DNA. ANCA testing, rheumatoid factor (RF), cryoglobulins, and antinuclear antibodies (ANA) are typically negative.
Patients with PAN present with constitutional symptoms (fever and weight loss) in the setting of organ dysfunction. Commonly seen manifestations include skin lesions – including palpable purpura, livedo, necrotic lesions, and digital infarcts; peripheral neuropathy and mononeuritis multiplex; abdominal pain due to mesenteric vasculitis; and hypertension with microscopic hematuria or proteinuria. Biopsy of affected tissue is crucial for establishing the diagnosis. If the presenting symptoms are related to mesenteric ischemia or renal involvement, then visceral angiogram can be helpful confirming the diagnosis. Angiographic findings include presence of saccular aneurysms, microaneurysms, occlusions and cutoffs with luminal irregularity, and stenosis of small and medium vessels of abdominal viscera. Severe gastrointestinal (GI) involvement is a major cause of morbidity in PAN. Renal biopsy is usually unhelpful, since the renal injury is not glomerular in nature. Microaneurysms of renal artery branches can occasionally rupture and cause renal hematomas. Myalgias due to skeletal muscle involvement and large joint arthralgias are common. Importantly, PAN does not affect the lungs or upper respiratory tract, which is an important feature in distinguishing this disease from ANCA-associated vasculitis.
In patients with hepatitis B-associated PAN, antiviral therapy should be initiated prior to immunosuppression. Some patients with severe manifestations of hepatitis virus-associated PAN benefit from short-term treatment with glucocorticoids and plasma exchange until the antiviral therapy becomes effective. Plasma exchange has not been shown to be effective in PAN that is not associated with hepatitis B. Prolonged immunosuppression should be avoided to facilitate immunologic clearance of hepatitis B-infected hepatocytes.
In patients with PAN not associated with viral disease, excellent 5-year survival rates of over 80% can be achieved with appropriate immunosuppressive therapy and use of steroids improves survival. For mild and isolated cutaneous disease, initial monotherapy with daily oral prednisone (1 mg/kg ideal body weight up to a maximum of 60 mg per day) is recommended. The initial dose should be continued for 4 weeks, and the taper should be guided by clinical improvement, tapering below 20 mg per day should be done slowly, not faster than by 2.5 mg every 14 days. Most patients remain on prednisone for approximately 6 to 8 months. Many patients with mild disease respond to glucocorticoid monotherapy, but for those patients who do not achieve remission with glucocorticoids alone, addition of a DMARD agent, such as azathioprine (2 mg/kg per day) or methotrexate (20–25 mg weekly) is recommended, with monitoring through rheumatology to allow prednisone to be weaned. Methotrexate should not be used in patients with renal disease or hepatitis.
For patients with moderate to severe disease, data from long-term follow-up studies in several cohorts of patients with PAN shows improved outcomes from induction therapy with steroids and cyclophosphamide , , followed by either azathioprine or methotrexate for remission maintenance. There has been no comparison of oral versus IV cyclophosphamide use in PAN; however, one small randomized controlled trial of 18 patients with PAN and 47 with microscopic polyangiitis (MPA) demonstrated that use of steroids with 12 monthly pulses of IV cyclophosphamide had a lower risk of relapse and higher event-free survival than patients receiving only 6 monthly pulses of IV cyclophosphamide. Mortality did not differ, and this study did not investigate remission maintenance regimens. Some investigators also extrapolate use of the “CYCLOPS” cyclophosphamide dosing regimen that was shown to be comparable to oral cyclophosphamide for induction and remission of ANCA-associated vasculitis, but this has not been studied in PAN. It should be noted that in the management of other forms of vasculitis, the IV dosing of cyclophosphamide often allows effective disease control with lower cumulative dose and potentially reduced bone marrow, bladder, ovarian, and testicular toxicity; but many of the original studies of cyclophosphamide use for vasculitis used the daily oral dosing regimen that is preferred by some due to a higher effective dose and better long-term response rates. In addition, cyclophosphamide should not be dosed without involvement of rheumatology, because this drug carries several adverse effects including cytopenias, gonadal failure, risk for hemorrhagic cystitis, and increased risk of malignancy. Dose reduction is necessary for renal insufficiency and advanced age, and the dose should be adjusted based on the nadir white blood count to minimize bone marrow toxicity. In addition, prophylaxis for Pneumocystis jirovecii (PJP) infection should be employed in patients receiving high-dose steroids in combination with DMARDs.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here