Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The gastrointestinal (GI) tract performs energy-demanding functions of digestion and absorption of nutrients while maintaining a critical barrier between the internal milieu and the external (luminal) environment. It also contributes to the activities of the immune system. These functions depend on a reliable blood supply. It is not surprising, therefore, that vascular disorders have important clinical manifestations. Vascular disorders usually manifest clinically as bleeding or ischemia, both of which occur in acute and chronic forms. In this chapter, vascular disorders are discussed in the context of these two types of clinical presentation, although there is considerable overlap between them.
The proximal esophagus derives its blood supply from the superior and inferior thyroid arteries, the middle esophagus from the bronchial and right intercostal arteries, and the distal esophagus from the left gastric and left inferior phrenic artery with additional supply from the splenic artery and celiac trunk. The middle and lower esophagus also receives arterial blood directly from the aorta. Venous drainage is also segmental. Blood from the proximal esophagus drains into the superior vena cava, that from the middle esophagus into the azygos or hemiazygos veins, and that from the distal esophagus through the left and short gastric veins into the portal vein. Anastomoses among the vessels that supply each of these regions result in complex arterial and venous networks. For instance, the venous network in the mucosa and submucosa of the middle and distal esophagus is the source of esophageal varices in patients with portal hypertension.
The stomach, proximal duodenum, gallbladder, liver, and pancreas are supplied by branches of the celiac trunk. The distal duodenum is supplied by a branch of the superior mesenteric artery. Numerous anastomoses between esophageal and gastric feeding vessels result in a complex vascular network which results in a protective effect against ischemia in these organs. The gastric and duodenal veins drain into the portal system.
The remainder of the small intestine is supplied by the inferior pancreaticoduodenal, jejunal, and ileal branches of the superior mesenteric artery, which also supplies the cecum and ascending and proximal transverse colon through its ileocolic, middle colic, and right colic branches. The inferior mesenteric artery supplies the distal transverse colon to the proximal rectum, whereas the distal rectum is supplied by the internal iliac and pudendal arteries. The arterial supply of the small and large intestines consists of numerous vascular arcades (vasa recta) with abundant anastomoses that result in a rich collateral circulation that helps protect the bowel against damage from pathological processes within individual blood vessels. Certain areas of the large bowel are predisposed to vascular insult, such as the splenic flexure and rectosigmoid colon. The ileocecal region is also predisposed to ischemic injury, but to a lesser extent. Venous drainage of the colon and rectum follows the arterial supply. The vascular collaterals in the rectum provide another location in which varices may develop in patients with portal hypertension.
The anus is supplied by the superior, middle, and inferior rectal arteries. Branches of these arteries have multiple small arteriovenous anastomoses with submucosal venous plexuses. Interestingly, the blood flow to the anal canal exceeds its metabolic requirements. Venous drainage of the anus is mainly to the superior rectal vein.
Blood flow to the GI tract is normally under tight physiological regulation through the autonomic nervous system. For example, the blood supply increases by as much as 100% immediately after ingestion of a meal. On the other hand, in states of shock, when it is vital to maintain blood flow to critical organs such as the central nervous system, splanchnic blood flow may be drastically reduced, sometimes beyond the critical level needed to maintain viability of the intestinal mucosa.
In general, surgery is performed for failed medical therapy and/or for perforation and other complications. Appropriate macroscopic inspection and sampling are critical to achieve a correct diagnosis. The serosal or adventitial surface, depending on the location within the GI tract, may reveal hemorrhage, necrosis, and serosal fibrin deposition if a perforation is present. Perforations can be microscopic and, as such, not readily evident on gross examination. However, the presence of external fibrinous membranes is often indicative of the perforation site. Serial sectioning should be performed if the perforation is not immediately evident. Serosal adhesions should also be sampled as they can represent the area most indicative of the underlying injury. Tissue sections should target the areas of worse injury to document the severity of disease and to help identify the underlying etiology. Special attention should be paid to sectioning the vasculature in the mesentery and omentum. In cases of thromboembolic disease and vasculitis, the key histological features often reside in the mesentery. Representative sections of the surgical margins should be obtained to predict viability of the anastomosis and any potential complications. If the specimen is received fresh, tissue may be submitted for culture and even immunofluorescence, if clinically indicated.
Bleeding from the upper GI tract is a frequent indication for endoscopy and is common worldwide. In the United States, acute GI bleeding accounts for 250,000 to 300,000 hospitalizations per year. Up to 14% of patients admitted on an emergency basis and as many as 28% of patients hospitalized die of their acute GI bleeding. , Upper GI tract bleeding, defined as bleeding proximal to the ligament of Treitz, is four times more common than lower GI tract bleeding. Upper GI bleeds occur most commonly in elderly patients, although in conditions such as hereditary hemorrhagic telangiectasia (HHT), onset of disease may occur as early as the third decade of life. Risk factors for upper GI tract bleeding include older patient age, alcohol use, and concomitant use of drugs such as nonsteroidal antiinflammatory drugs (NSAIDs) and anticoagulants.
Patients often present with direct evidence of a GI bleed, such as hematemesis, melena, heme-positive stools, and, less commonly, hematochezia. They may also present with signs and symptoms of iron-deficiency anemia, such as syncope, chest pain, dizziness, and shortness of breath. In severe, acute, life-threatening hemorrhage, the clinical presentation is usually a result of shock or cardiovascular collapse.
The most important causes of esophageal bleeding are varices that develop as a result of portal hypertension, Mallory-Weiss lacerations, or esophagitis ( Table 11.1 ).
| Entity | Key Clinical Features | Key Pathological Features | Treatment |
|---|---|---|---|
| Gastroesophageal reflux disease | Most common symptoms are heartburn, regurgitation, and dysphagia More prevalent after 40 years of age |
Typically distal 7 cm of esophagus Background esophagitis: squamous hyperplasia, intraepithelial neutrophils, and increased eosinophils and lymphocytes |
Medical options: PPI and H 2 antagonists Surgical options: fundoplication and gastropexy |
| HSV infection | Main symptom: odynophagia Common in immunocompromised patients, particularly organ and bone marrow transplant recipients Occurs in immunocompetent patients |
Vesicles early feature; coalesce to form ulcer Ground-glass nuclear inclusions in squamous cells at edge of shallow, punched-out ulcers HSV immunostain confirms the diagnosis |
Antivirals (e.g., acyclovir) May resolve spontaneously in immunocompetent patients |
| Candida infection | Main symptom: substernal dysphagia More common in immunocompromised patients Often coexists with other etiologies |
Patchy white mucosal plaques Neutrophils, yeast, and pseudohyphae in superficial squamous epithelium Usually with desquamation: often detached fragments in biopsies Fungal stains (PAS, GMS) often helpful |
Antifungals (e.g., fluconazole, itraconazole) |
| CMV infection | Main symptom: odynophagia Common in immunocompromised patients In HIV-infected patients, more common than HSV |
Ulcers deeper, more linear than in HSV Single large nuclear and multiple amphophilic cytoplasmic inclusions in capillary endothelial or stromal cells in granulation tissue at base Immunostaining may be necessary because inclusions can be rare |
Antivirals (e.g., ganciclovir, foscarnet) |
| NSAIDs | Concomitant illnesses necessitating NSAIDs (e.g., chronic back pain, arthritis) Simultaneous alcohol use common |
Shallow, large ulcers with broad base, usually in middle esophagus Usually devoid of background esophagitis |
Discontinue medication Supportive therapy |
| Pill/medication induced | Sudden onset of symptoms Pills swallowed without fluids Can be caused by many medications (e.g., tetracycline, potassium chloride, bisphosphonate, quinidine) |
Nonspecific superficial desquamation of squamous epithelium, spongiosis, necrotic keratinocytes Exudate seen commonly with quinidine-induced ulcers |
Educate patient to take pills with fluids Discontinue medication, or start liquid therapy if necessary Supportive therapy |
| Radiation | Usually a history of head and neck, mediastinal, pulmonary, or esophageal malignancy | Fibrinoid necrosis and dilation of blood vessels, vascular intimal proliferation, stromal fibrosis, stellate fibroblasts ± cytological atypia and increased apoptosis | Supportive therapy Surgery if perforation or fistula develops |
| Foreign-body injury | Most common in children; also seen in elderly, psychiatric patients, and inmates Sudden onset of symptoms; may lead to esophagovascular fistula |
Nonspecific necrosis, inflammation, and ulceration; may progress to perforation | Endoscopic or surgical removal Resection or repair of perforation or fistula |
| Chemical injury | Similar to foreign body injury Alkaline ingestion damages esophagus more commonly |
Necrosis more common | Supportive therapy May require resection |
| Varices ∗ | Occur in portal hypertension (cirrhotic and noncirrhotic) Schistosomiasis and viral hepatitis are common causes worldwide Typically asymptomatic until rupture; rebleeding is common |
Most common in distal 3 to 4 cm of esophagus Dilated tortuous veins of lamina propria and submucosa bulging into lumen, fresh hemorrhage and adjacent thrombosis Erosions and ulcers uncommon Thrombosis, ulceration, necrosis, and inflammation more likely after therapy |
Sclerosing and banding varices Portosystemic shunting Medical management of portal hypertension |
| Mallory-Weiss tears ∗ | Strong association with chronic alcoholism; ASA use common Typical history (retching or forceful vomiting) in only 30% Related to upward diaphragmatic movement |
Minority involve esophagus; majority in lesser curve of proximal stomach, may be at esophagogastric junction Nonspecific mucosal breach with acute hemorrhage, seldom into submucosa Usually no acute inflammatory response |
Usually self-limited If therapy is required: balloon tamponade, embolization, medical management Surgery rare |
Esophageal varices are dilated, tortuous veins within the lamina propria and submucosa that bulge into the esophageal lumen because of portal hypertension and portosystemic shunting. Esophageal varices may develop in any condition that leads to portal hypertension, but they are most often associated with alcoholic cirrhosis. The demographic features of patients with esophageal varices are similar to those of patients with cirrhosis and portal hypertension. In some parts of the world, hepatic schistosomiasis is a common cause of esophageal varices. Varices are typically asymptomatic until they rupture into the esophageal lumen, which results in hematemesis or melena.
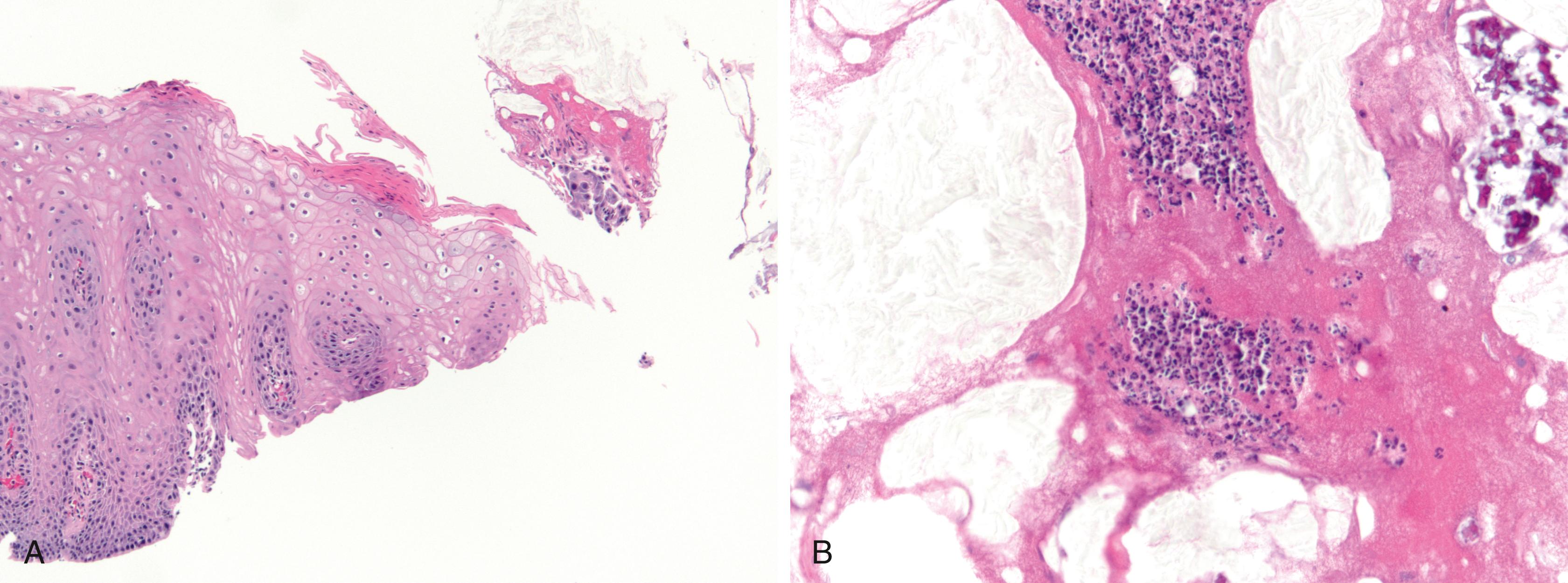
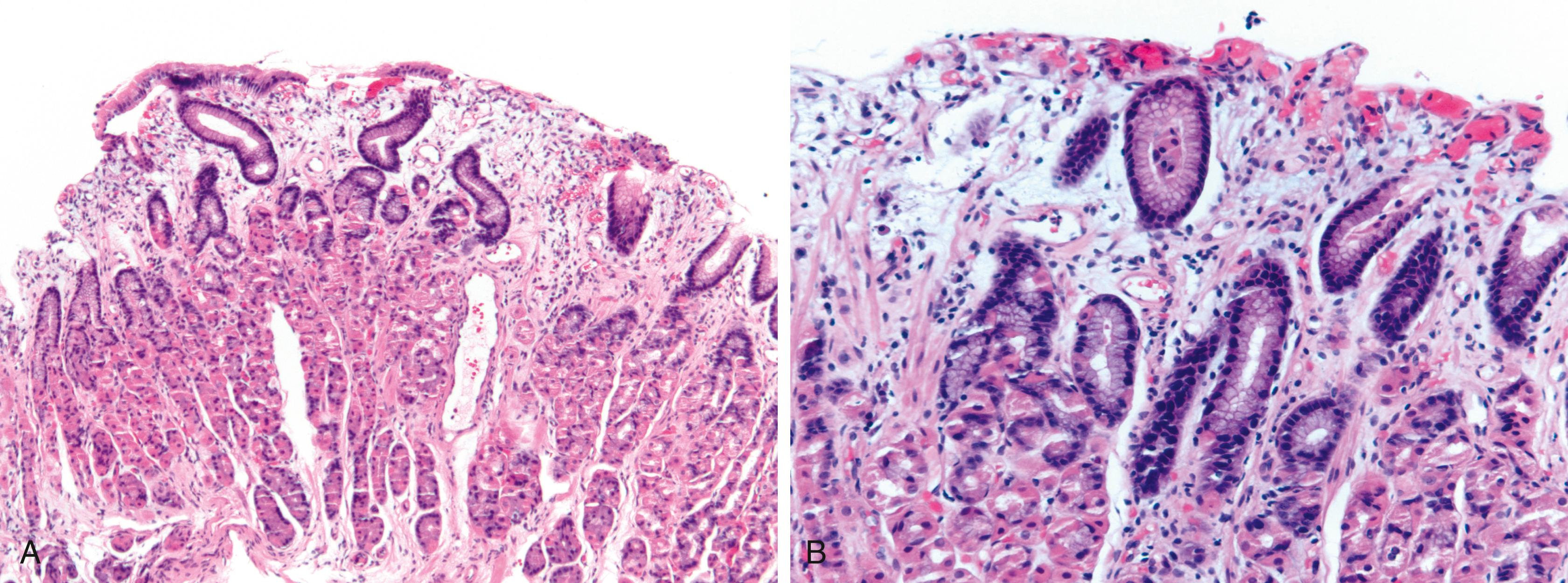
Bleeding varices are most common in the caudal portion of the esophagus. However, a discrete bleeding site is usually difficult to identify pathologically. Varices tend to collapse at the time of autopsy and therefore are best diagnosed endoscopically. In autopsy specimens, eversion and formalin fixation of the esophagus are techniques that can be used to help demonstrate varices. Grossly dilated, tortuous veins may be seen in the distal esophagus, in particular below the aortic arch, protruding into the lumen ( Fig. 11.1A ). There may be superimposed thrombosis and mucosal erosions.
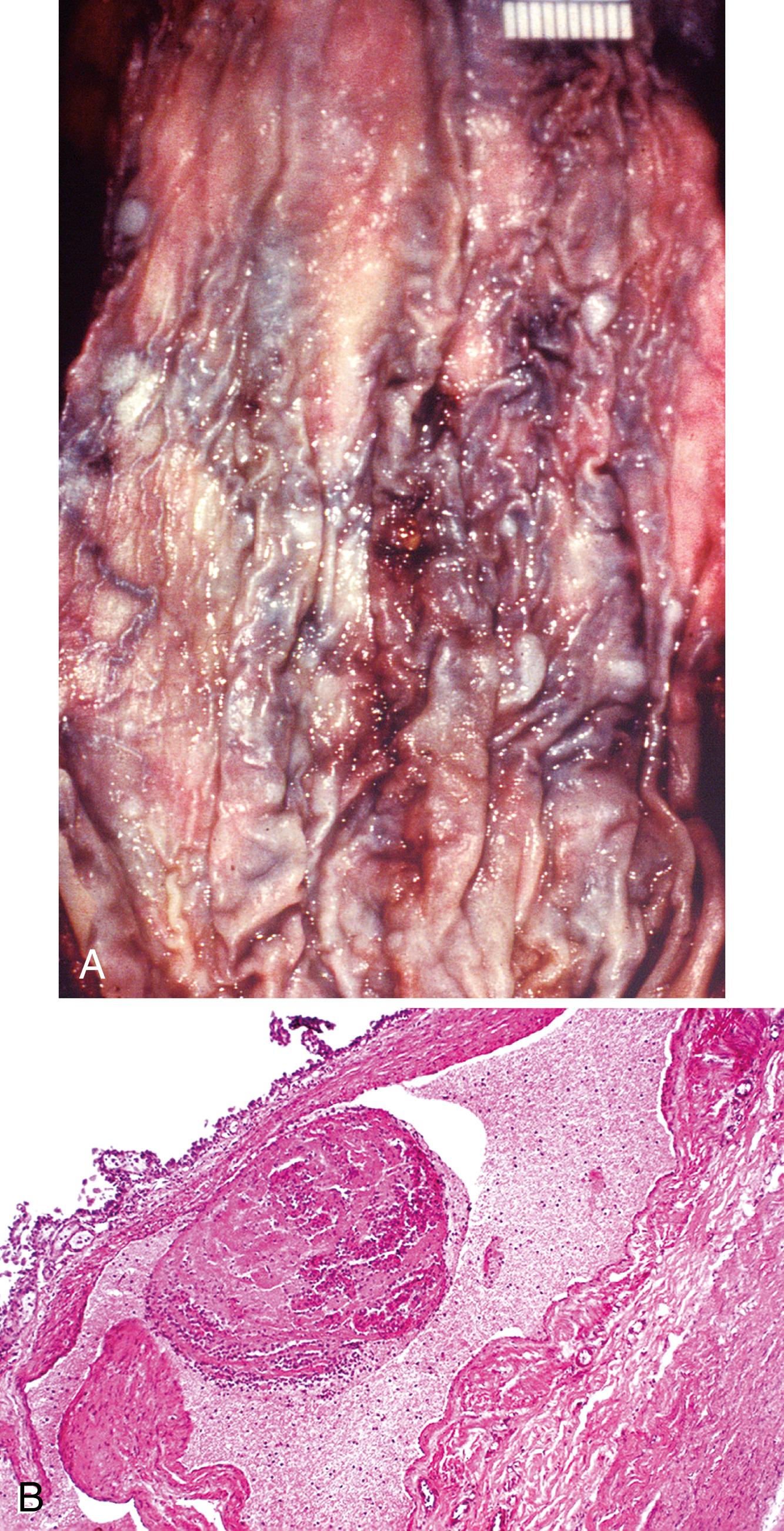
Histologically, dilated lamina propria and submucosal veins are characteristic. These are usually associated with fresh hemorrhage, organizing thrombi, and hemosiderin deposition ( Fig. 11.1B ). Surface ulcers, erosions, and reactive epithelial changes in the overlying epithelium may be present as well. In specimens examined after treatment with sclerotherapy or endoscopic ligation, other findings may include thrombosis, ulceration, necrosis, inflammation, and fibrosis as a late event. , Elastic and/or Movat stains can help highlight obliterated blood vessels.
Although variceal bleeding is the most important cause of hematemesis in patients with portal hypertension, other causes of upper GI bleeding are implicated in approximately 50% of patients who are seen with hematemesis ( Table 11.2 ; see Table 11.1 ).
| Entity | Key Clinical Features | Key Pathological Features | Treatment |
|---|---|---|---|
| Helicobacter pylori –induced peptic ulcers | Most common cause Decreasing prevalence rates |
Gastritis more common in antrum Typically superficially oriented lymphoplasmacytic gastritis with neutrophil infiltrate and spiral forms of H. pylori May have reactive lymphoid follicles, intestinal metaplasia, and mucosal atrophy Ulcers may be located in duodenum |
H. pylori eradication therapy Antisecretory therapy |
| Chemical-induced ulcers | NSAID use is a clear predisposing factor to gastric bleeding | Erosions or shallow ulcers More common in fundus and body Usually without background gastritis |
Discontinue medication, or significantly reduce dose |
| Mucin loss with nuclear enlargement and hyperchromasia in adjacent epithelium | Supportive therapy | ||
| Stress-related ulcers | Patients with multiple comorbidities; risk factors include prior PUD, CNS trauma or surgery, sepsis, multiple trauma, liver and kidney failure, and organ transplantation In hospital patients, duodenal ulcers more later in course Curling ulcer: following burns Cushing ulcer: following neurological injury or surgery |
Erosions or shallow ulcers Usually without background gastritis More common in fundus and body, may also be seen in duodenum Abrupt erosions or ulcers with interstitial hemorrhage, reactive epithelial atypia Adjacent mucosa with acute hemorrhagic gastritis, diffuse mucosal hyperemia, edema |
Supportive therapy; may include blood transfusion. Prophylactic therapy to prevent additional ulcers (includes PPI, antacids, H 2 antagonists, sucralfate, prostaglandin analogues) |
| Dieulafoy lesions | Most common in middle-aged and elderly men | Most common in proximal stomach on lesser curve Similar lesions reported in distal esophagus and small and large bowel Small mucosal defect with abnormally large, thick-walled artery in base Adjacent mucosa usually lacks inflammation |
Therapeutic endoscopy (e.g., clipping, electrocoagulation, injection sclerotherapy, banding) Surgical ligation or resection |
| Cameron ulcers | Associated with hiatal hernias | Linear ulcers in hiatal hernias Histological features of a benign ulcer |
Therapeutic endoscopy to control bleeding Surgical management of hernia |
| Varices ∗ | Most commonly in continuity with esophageal varix with similar morphology | See Table 11.1 | |
| Portal hypertensive gastropathy and gastric vascular ectasia | See Table 11.3 | See Table 11.3 | |
| HHT | Autosomal dominant disease with variable penetrance and expression Telangiectases on skin and mucous membranes Frequently have history of GI bleeding 20% have no family history of symptoms |
More common in the stomach, but also seen in the esophagus and duodenum Lesions include telangiectasias, arteriovenous malformations, aneurysms, venous varicosities, and arteriovenous fistulas Classically clusters or tufts of dilated, tortuous arteriolar-venular connections without intervening capillaries |
Medical therapy includes danazol, estrogen, aminocaproic acid Therapeutic endoscopy (coagulation, cautery, or laser) Surgical resection |
| Hemodialysis-associated telangiectasia | Long-term hemodialysis | Morphologically similar to HHT, may appear reddish and fernlike grossly | Therapeutic endoscopy (thermal coagulation) |
Esophageal varices often rebleed. The risk of dying within 6 weeks of an initial bleed is 20% to 30% in patients with cirrhosis-related portal hypertension. Variceal bleeding may precipitate hepatic encephalopathy in cirrhotic patients. Treatment modalities include sclerosis and banding of individual varices, portosystemic shunting, and pharmacological management of portal hypertension.
Mallory-Weiss laceration is a longitudinal tear of the mucosa located in the region of the gastroesophageal junction. These lesions may bleed profusely. A clinical history of retching or forceful vomiting is identified in approximately 30% of patients. Mallory-Weiss lacerations develop mainly in patients with chronic alcoholism and typically occur in the third to fifth decades of life. Concomitant aspirin use has been reported in approximately 30% of patients. Other risk factors include upward diaphragmatic movement related to coughing, heavy lifting, pregnancy, and abdominal trauma. Mallory-Weiss laceration is an uncommon complication of upper GI endoscopy in association with retching and hiatal hernia. In addition, some patients present with melena or iron-deficiency anemia.
The pathogenesis of Mallory-Weiss laceration is related to upward movement of the diaphragm and an increase in intraabdominal pressure, which leads to protrusion of the proximal stomach into the thoracic cavity. This is often preceded by nausea, which causes distention of the stomach and reflux of gastric contents into the esophagus. When protrusion of the distended stomach is forceful, longitudinal lacerations may develop. Lacerations are more likely to occur in patients with a hiatal hernia.
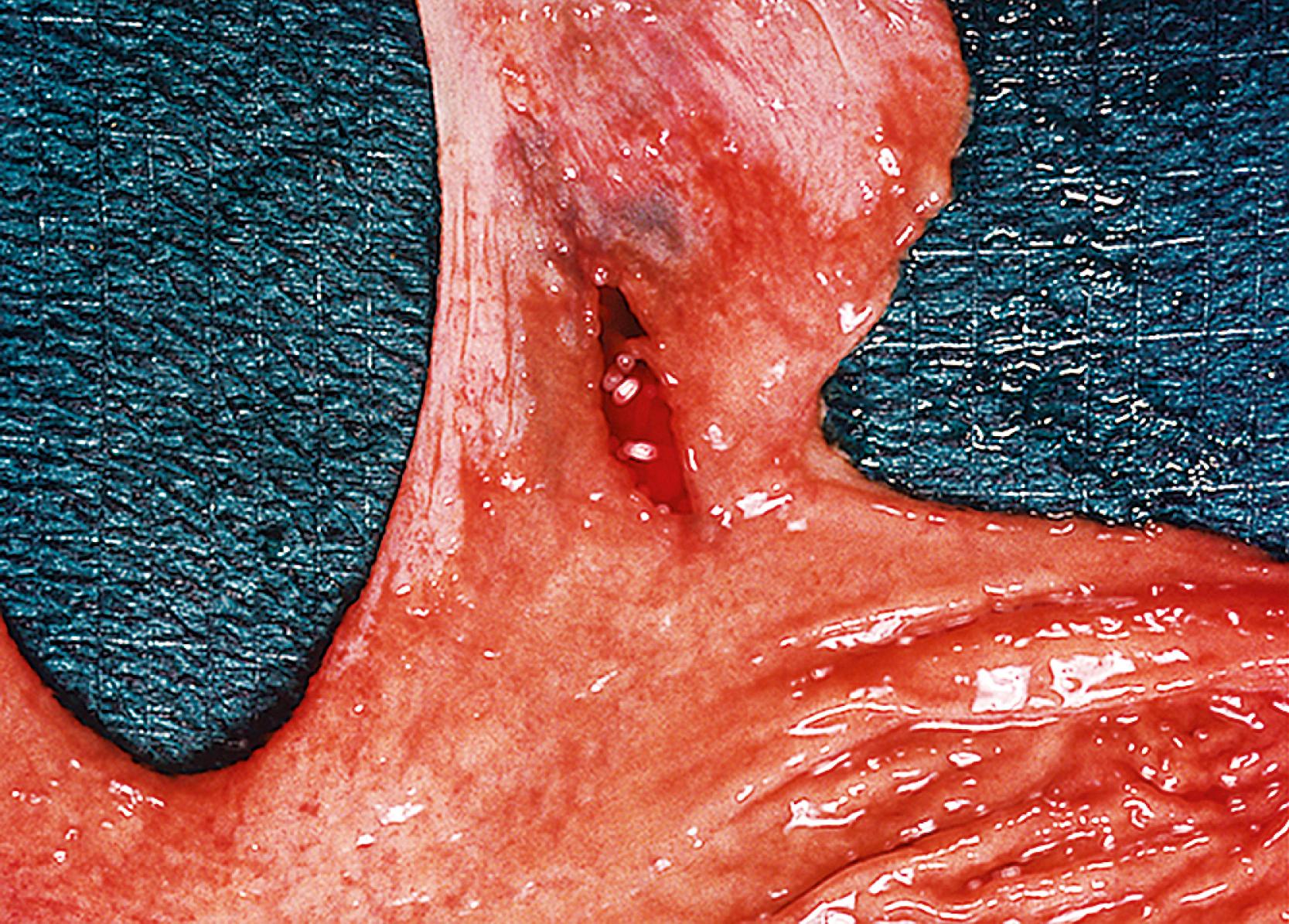
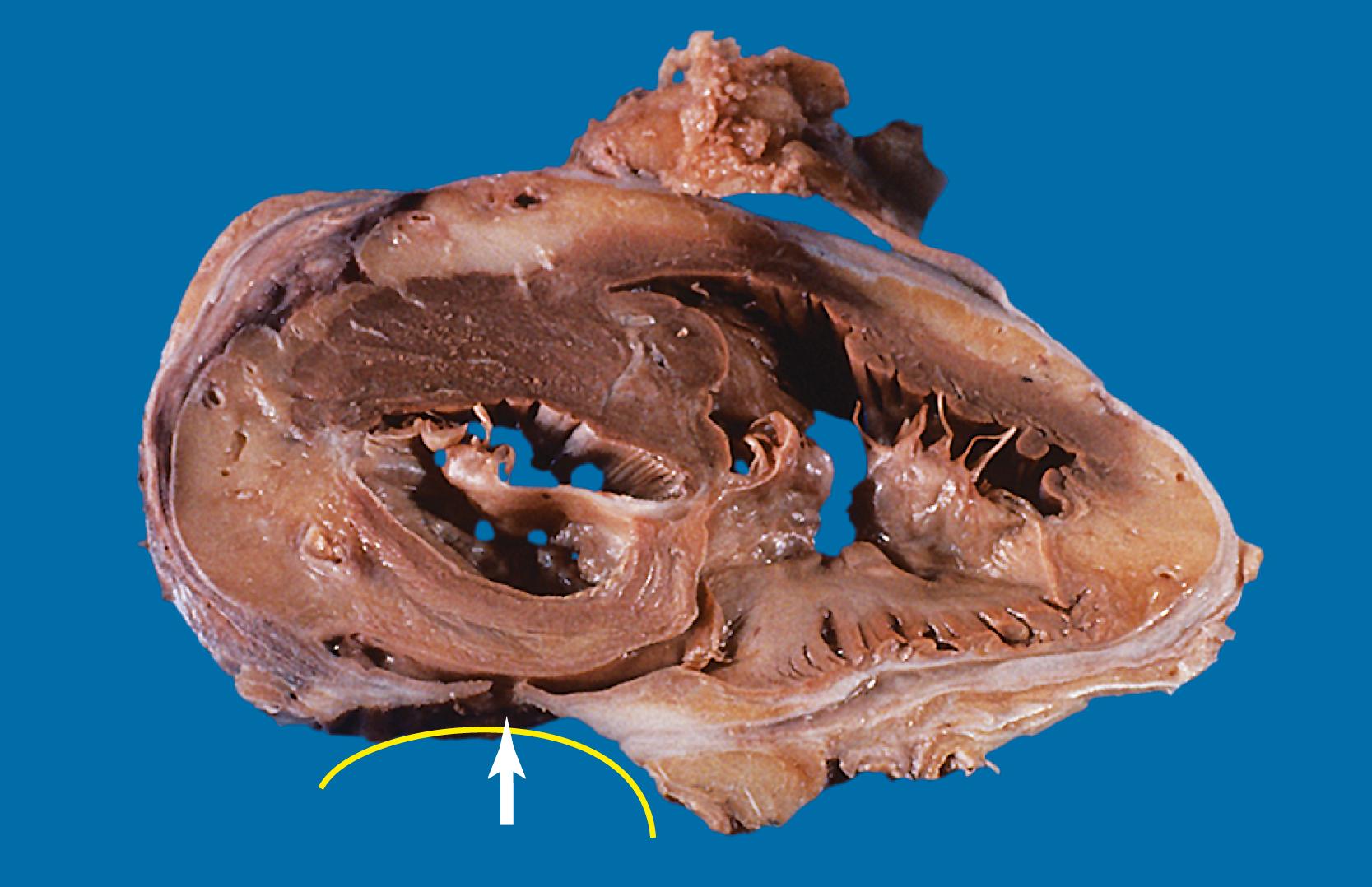
Most Mallory-Weiss lacerations are located on the gastric side of the gastroesophageal junction. Only a minority involve the tubular esophagus. They occur most commonly on the lesser curve of the proximal stomach ( Fig. 11.2 ) but may also occur at the gastroesophageal junction. Histologically, Mallory-Weiss lacerations are characterized by a longitudinal breach of the mucosa that extends into the submucosa, but generally not into the muscularis propria, usually accompanied by hemorrhage, either with or without an acute inflammatory response. Healing Mallory-Weiss lacerations show granulation tissue, fibrosis, epithelial regeneration, and other features of healing ulcers.
Mallory-Weiss lacerations are usually treated supportively. In some patients with persistent bleeding, pharmacological management, balloon tamponade, embolization, and, rarely, surgery may be required to establish hemostasis. Boerhaave’s syndrome (acute perforation of the esophagus) is a catastrophic event that is considered a complication of Mallory-Weiss lacerations. However, patients with Boerhaave’s syndrome do not typically present with severe acute GI bleeding.
Esophagitis and esophageal ulcers are most commonly caused by gastroesophageal reflux disease (GERD), infection (e.g., herpesvirus, Candida , cytomegalovirus), drugs, chemical or physical injury from accidental or intentional ingestion of toxic (alkaline and acidic) substances, or foreign objects. Bleeding from esophagitis is usually occult, and patients commonly present with anemia. Bleeding from esophageal ulcers varies in severity depending on the cause, but it is most often acute. Signs and symptoms include hematemesis, chest or epigastric pain, and odynophagia. Most patients with acute bleeding present initially in the emergency department, and many of them have significant comorbid conditions.
Overall, GERD-associated ulcers are most common, and they occur in all age groups, although they are more prevalent after 40 years of age. Ulcers caused by infections are more likely to occur in immunocompromised patients. Certain drugs are more commonly associated with esophageal mucosal injury, such as doxycycline, amoxicillin, ciprofloxacin, metronidazole, rifaximin, antihypertensive drugs, NSAIDS, bisphosphonates, and warfarin, among many others. Concomitant alcohol use has been reported in a subset of patients with NSAID-induced esophageal ulcers, suggesting that it may have a synergistic effect. Ulcers related to medication injury are common in the elderly, whereas those caused by foreign objects are more common in children. Reflux is less likely to be associated with bleeding than use of NSAIDs, which causes injury by direct mucosal contact.
Other causes of esophageal ulcers include Crohn’s disease and radiation-induced injury caused by vascular compromise. Injury from chemical agents, such as lye, is caused by their corrosive effect on the mucosa.
Ulcers resulting from GERD occur mainly in the distal third of the esophagus. Adjacent mucosal changes typical of reflux, such as squamous hyperplasia with prominent fibrovascular papillae and intraepithelial inflammation (eosinophils, neutrophils, and/or lymphocytes), are usually present. Herpesvirus inclusions are identified most readily in squamous cells at the edges of herpetic ulcers ( Fig. 11.3A,B ). In contrast, cytomegalovirus inclusions are most often found in endothelial cells and/or stromal cells at the ulcer base. Candida should be considered wherever neutrophils accumulate in the surface epithelium, usually in association with superficial desquamation. Morphological features of radiation injury include dilated and thickened capillaries with deposition of hyaline, prominent endothelial cells, and reactive stroma with atypical stellate fibroblasts. NSAID-induced ulcers are typically large, shallow lesions with a broad base and are most common in the middle esophagus ( Fig. 11.4 ). Pill esophagitis shows superficial epithelial sloughing, keratinocyte necrosis, spongiosis, intraepithelial eosinophils, and associated crystalline birefringent particles ( Fig. 11.5A,B ). Ulcerating malignant neoplasms may also be a source of bleeding, but this is an unusual presentation of esophageal cancer. However, the most common indication for endoscopy in patients with a secondary malignant neoplasm of the esophagus is GI bleeding. Bleeding from NSAID-induced ulcers is usually active and infrequently complicated by strictures. Rarely, esophageal or gastric ulcers perforate or penetrate into contiguous vascular organs, such as the heart and aorta, leading to massive bleeding ( Fig. 11.6 ). Ulcers resulting from foreign bodies are particularly prone to this type of complication.
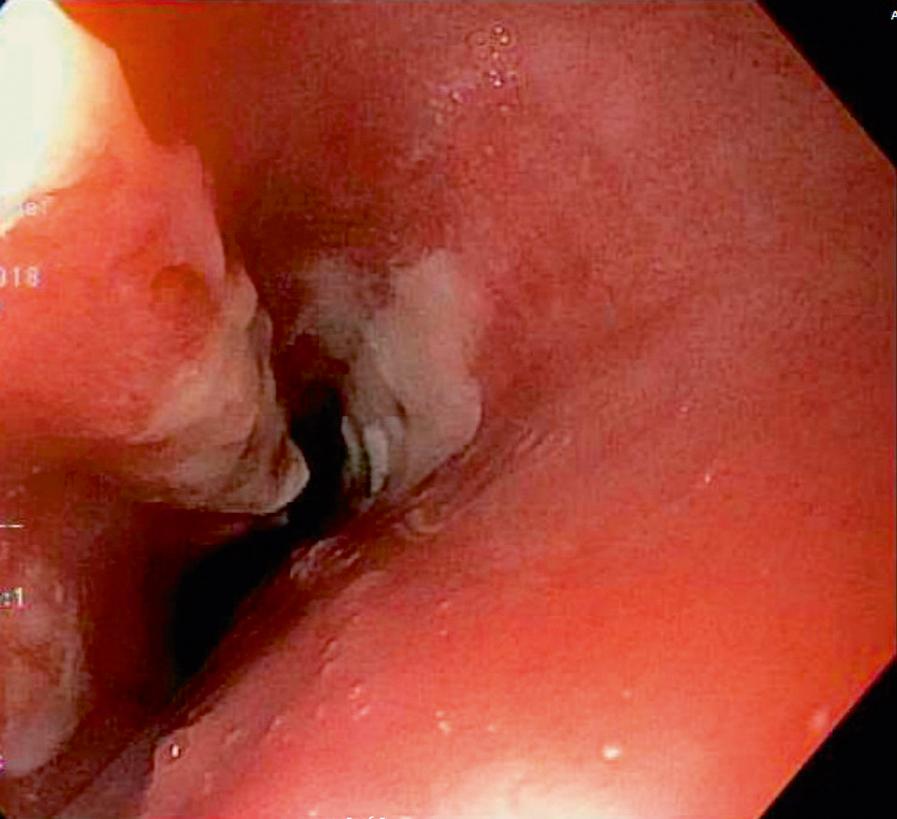
Acute esophageal necrosis (AEN; also known as black esophagus ) is a rare disease. It develops as a result of multiple factors, such as ischemia (hemodynamic compromise and low-flow states), corrosive injury (such as gastric contents in the setting of esophago-gastroparesis and gastric outlet obstruction), and in patients with decreased protective/reparative mechanisms of the mucosal barrier (which is common in malnourished and debilitated patients). Patients are frequently older-aged males who present with bleeding, epigastric/abdominal pain, vomiting, dysphagia, fever, and syncope. At endoscopy, and on macroscopic examination, there is diffuse circumferential black-colored mucosal discoloration that starts distally and extends proximally ( Fig. 11.7 ). Pathologically, necrosis of the esophageal mucosa, with variable involvement of the submucosa and muscularis propria, are typical features observed ( Fig. 11.8A,B ). This entity is associated with a mortality rate of approximately 32%. Complications include perforation, mediastinitis, esophageal stricture, and infection.


Esophageal diverticula are rare and usually asymptomatic. However, patients with diverticula may occasionally present with upper GI tract bleeding. Bleeding may occur in association with an ulcer, entrapped pills, or use of anticoagulants.
Aside from bleeding from varices, which commonly involves both the esophagus and the proximal stomach, gastric bleeding is most often caused by benign ulcers and erosive gastritis (see Table 11.2 ).
Gastric varices have clinical and pathological features similar to those of esophageal varices. They most commonly occur on the lesser curve of the proximal stomach, in continuity with esophageal varices. Reports vary as to whether gastric varices, compared with esophageal varices, are less likely or equally likely to bleed. Bleeding from gastric varices, when it does occur, is usually severe.
An estimated 350,000 cases of acute gastric ulcers are diagnosed annually in the United States. There are many causes of acute gastric (and duodenal) ulceration. Overall, gastric ulcers are more common in men than in women, and they most often occur in middle-aged and elderly patients.
Peptic ulcers, both acute and chronic (including those located in the duodenum), account for 20% to 50% of cases of upper GI bleeding. Risk factors for peptic ulcer disease include Helicobacter pylori infection, NSAIDs, and alcohol.
Stress ulcers are defined as acute gastric ulcers that develop in patients with shock, sepsis, or trauma. Stress ulcers have multiple synonyms, such as acute hemorrhagic gastritis. Curling ulcers are those that develop after severe burns. Cushing ulcers are those that develop after severe head trauma. Steroid ulcers are caused by steroid use. Risk factors for stress ulcers include respiratory failure, coagulopathy, recent major surgery, major trauma, severe burns, hepatic or renal disease, sepsis, and hypotension.
Bleeding from acute gastritis may also occur in long-distance runners and is of uncertain pathogenesis. , Cocaine can cause gastric erosions and bleeding. Bleeding may also occur when an ulcer erodes into an underlying blood vessel. For instance, Dieulafoy lesions (also called caliber-persistent artery ) are bleeding ulcers that occur most commonly in the lesser curvature of the stomach in close proximity to the cardia, but they can also occur in the small and large intestine and rarely in the esophagus. Dieulafoy lesions are characterized by the presence of a single, unusually largediameter mural arteriole that penetrates into the submucosa ( Fig. 11.9A ). These large vessels may cause massive bleeding ( Fig. 11.9B–D ). It has been reported in 1% to 2% of resection specimens and more recently with prior surgery. Cameron ulcers are defined as linear ulcers that form in a sliding hiatal hernia; they can cause gastric bleeding.
Mass lesions, located either in the mucosa or deeper within the gastric wall, may erode the overlying mucosa and cause chronic low-grade bleeding ( Fig. 11.10 ). Fundic gland polyps, gastric adenomas, ectopic pancreas, malignant tumors (e.g., primary gastric adenocarcinomas, lymphomas, endocrine tumors), GI stromal tumors, and metastatic tumors (e.g., melanomas, breast carcinomas) can all cause upper GI bleeding. Gastric bleeding may occasionally be iatrogenic in origin, such as in patients postsurgery for obesity.
Gastric ulcers are loosely defined as full-thickness loss of the gastric mucosa. Gastric erosions, in contrast, are defined by partial loss of mucosa, with preservation of the muscularis mucosae. On gross examination, erosions appear as small, focal, erythematous areas of mucosa. Gastric ulcers are sharply demarcated, usually circular depressions in the mucosal surface. Acute ulcers may have an erythematous base and are usually covered with clotted blood and fibrin. Chronic ulcers have a distinctive gross appearance resulting from scarring of the underlying tissue. It results in the formation of radiating cicatricial folds in the mucosa surrounding the ulcer. Histologically, erosions show loss of superficial mucosa, fibrinopurulent exudate, and reactive changes in the surrounding epithelium (loss of mucin, nuclear hyperchromasia, and increased mitotic activity). Acute ulcers show necrosis, granulation tissue, and hemorrhage. Chronic ulcers have a granulation tissue base with underlying fibrosis that often involves the muscularis propria. In cases of Dieulafoy lesions, the large-sized artery in the submucosa is usually associated with mucosal erosion and evidence of bleeding.
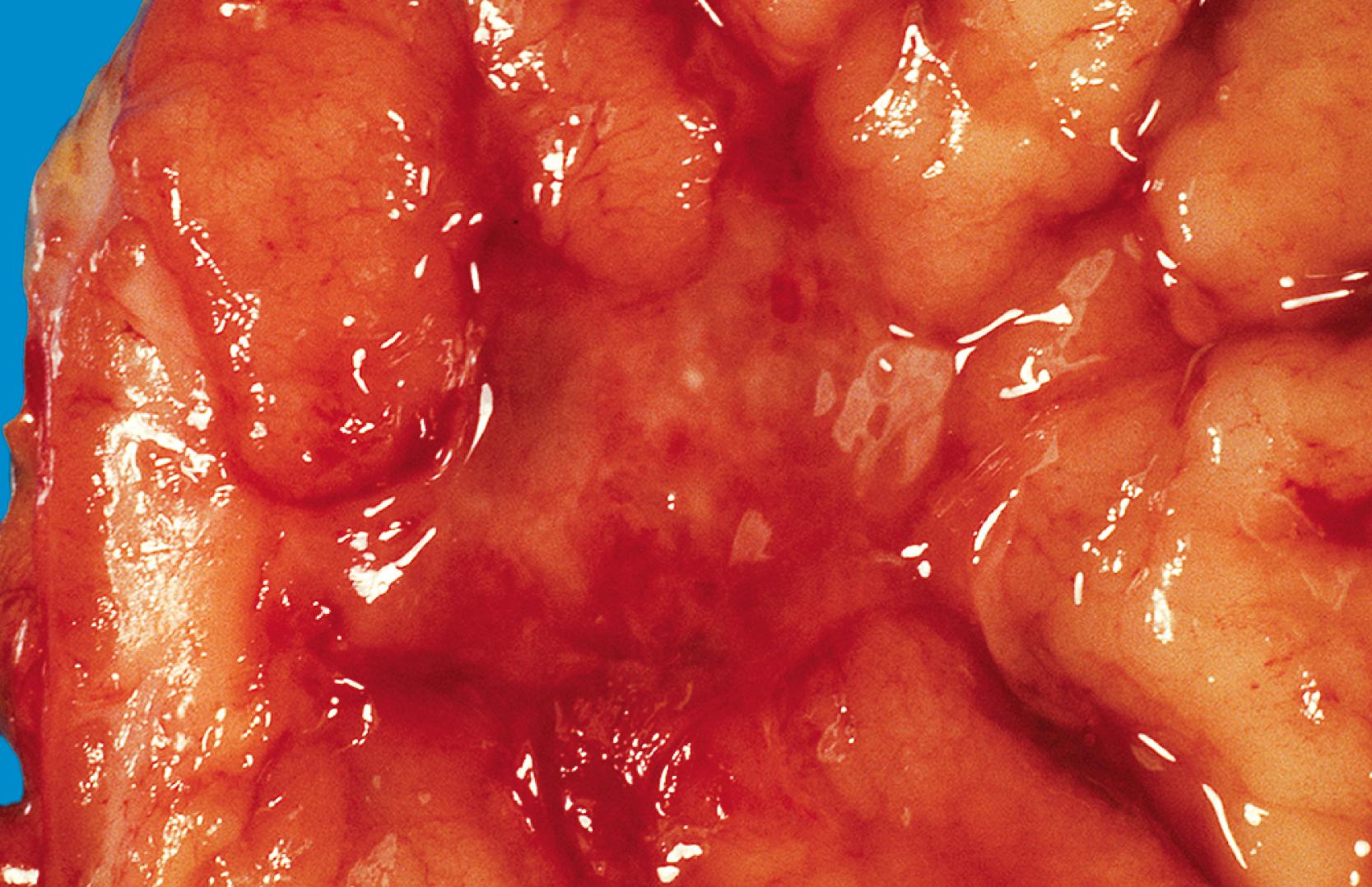
Portal hypertensive gastropathy occurs in up to 90% of patients with cirrhosis-related typically severe portal hypertension. It is characterized by a mosaic pattern of the mucosa at endoscopy, either with or without petechial hemorrhages, usually in the proximal stomach. Portal hypertensive gastropathy may also occur in patients without cirrhosis. It is most often detected in patients with portal hypertension who are being evaluated for variceal bleeding. Portal hypertensive duodenopathy has been described in 51% of portal hypertensive patients and is an uncommon cause of occult GI bleeding. Endoscopic features include erythema, erosions, ulcers, telangiectases, and duodenal varices. Some authors have described a characteristic “snakeskin” appearance to the gastric mucosa ( Fig. 11.11 ). Endoscopic-pathological correlation of portal hypertensive gastropathy is about 67%. Patients can be asymptomatic, or they can have abdominal pain and other symptoms of chronic bleeding.

Altered blood flow has been implicated in the pathogenesis of portal hypertensive gastropathy. Other postulated mechanisms include nitric oxide production, tumor necrosis factor-α synthesis, and sensitivity to prostaglandin inhibition.
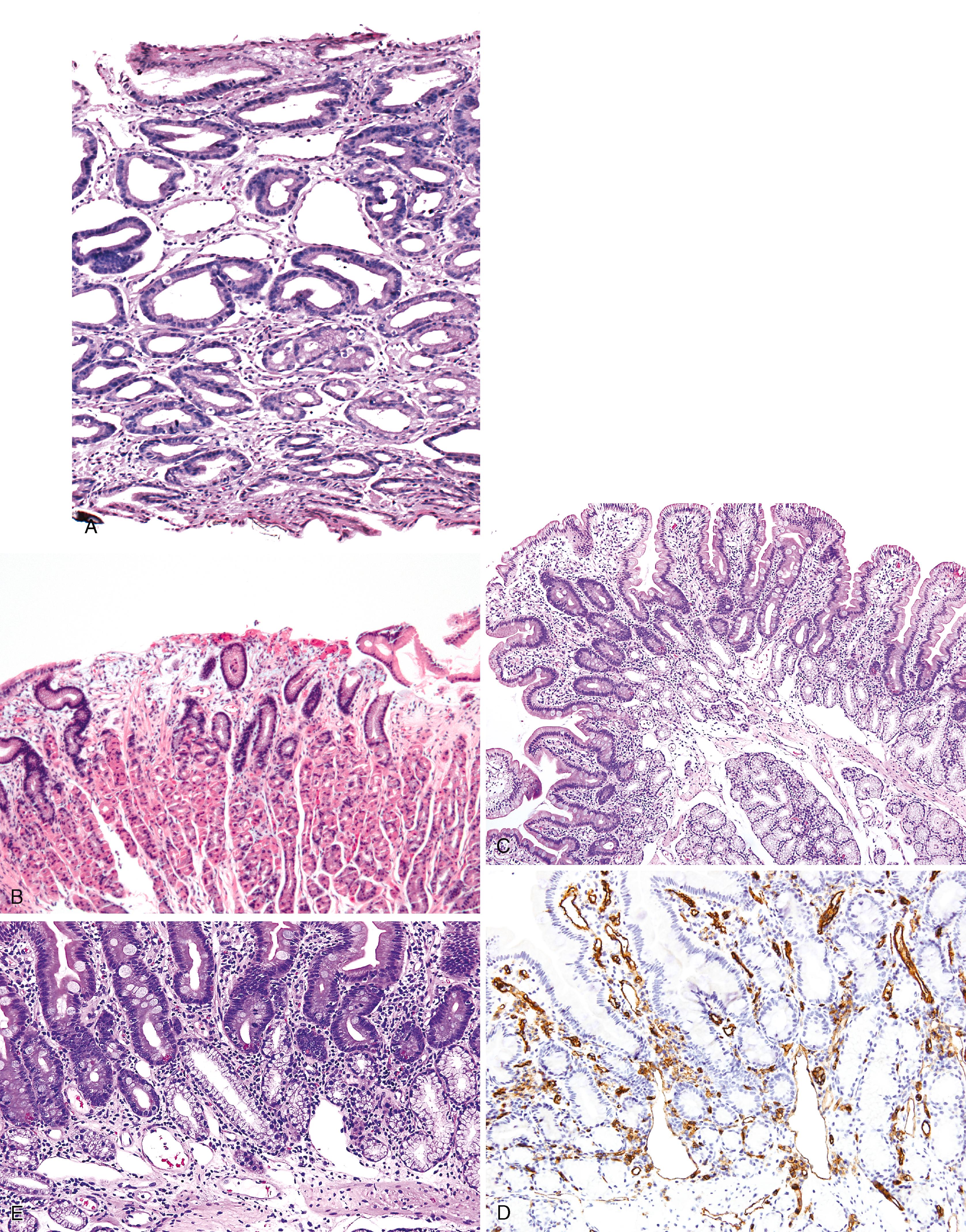
Portal hypertensive gastropathy occurs most commonly in the fundus and body of the stomach. Histological features include the presence of numerous ectatic and congested capillaries and venules in otherwise relatively normal-appearing mucosa and submucosa. However, morphological findings classic of “reactive” gastropathy are frequently present as well. Many cases show lamina propria edema below the surface epithelium ( Fig. 11.12A,B ). Fibrin thrombi, lamina propria inflammation, mucosal fibrosis, and fibrohyalinosis are not common components of portal hypertensive gastropathy, but they do occur in more chronic cases. There is no particular association with atrophic gastritis, CREST syndrome ( c alcinosis, R aynaud phenomenon, e sophageal involvement, s clerodactyly, and t elangiectases), or bone marrow transplantation ( Table 11.3 ). Portal hypertensive duodenopathy usually occurs in association with gastropathy; it is characterized by capillary congestion, capillary angiogenesis, and edema in the duodenal lamina propria ( Fig. 11.13A–D ), but usually only minimal inflammation.
| Features | Portal Hypertensive Gastropathy | Gastric Antral Vascular Ectasia |
|---|---|---|
| Clinical | ||
| Age | Adults and children | Middle aged to elderly |
| Gender | Male predominance | Female:male = 4:1 |
| Cirrhosis | ∼95% | ∼40% |
| Portal hypertension | 100% | ∼40% |
| Iron-deficiency anemia | Uncommon | Typical |
| Atrophic gastritis | Not associated | Associated |
| CREST syndrome | Not associated | Associated |
| Bone marrow transplantation | Not associated | Associated |
| Endoscopic | ||
| Location | Proximal stomach | Antrum |
| Red spots | Present | Present |
| Mosaic pattern | Present | Absent |
| Watermelon pattern | Absent | Often present |
| Pathological | ||
| Background mucosa ∗ | Oxyntic | Antral |
| Ectatic mucosal vessels | Present | Present |
| Fibrin thrombi ∗ | Absent | Present |
| Spindle cell proliferation ∗ | Absent | Present |
| Fibrohyalinosis ∗ | Absent | Present |
| CD61-positive stain in thrombi | Absent | Present |
| Treatment | ||
| Endoscopic ablation | Not required | Effective |
| Control of portal hypertension | Effective | May also be necessary |
Bleeding from portal hypertensive gastropathy is usually chronic and often controllable by medical or surgical management of the underlying cause of the patient’s portal hypertension.
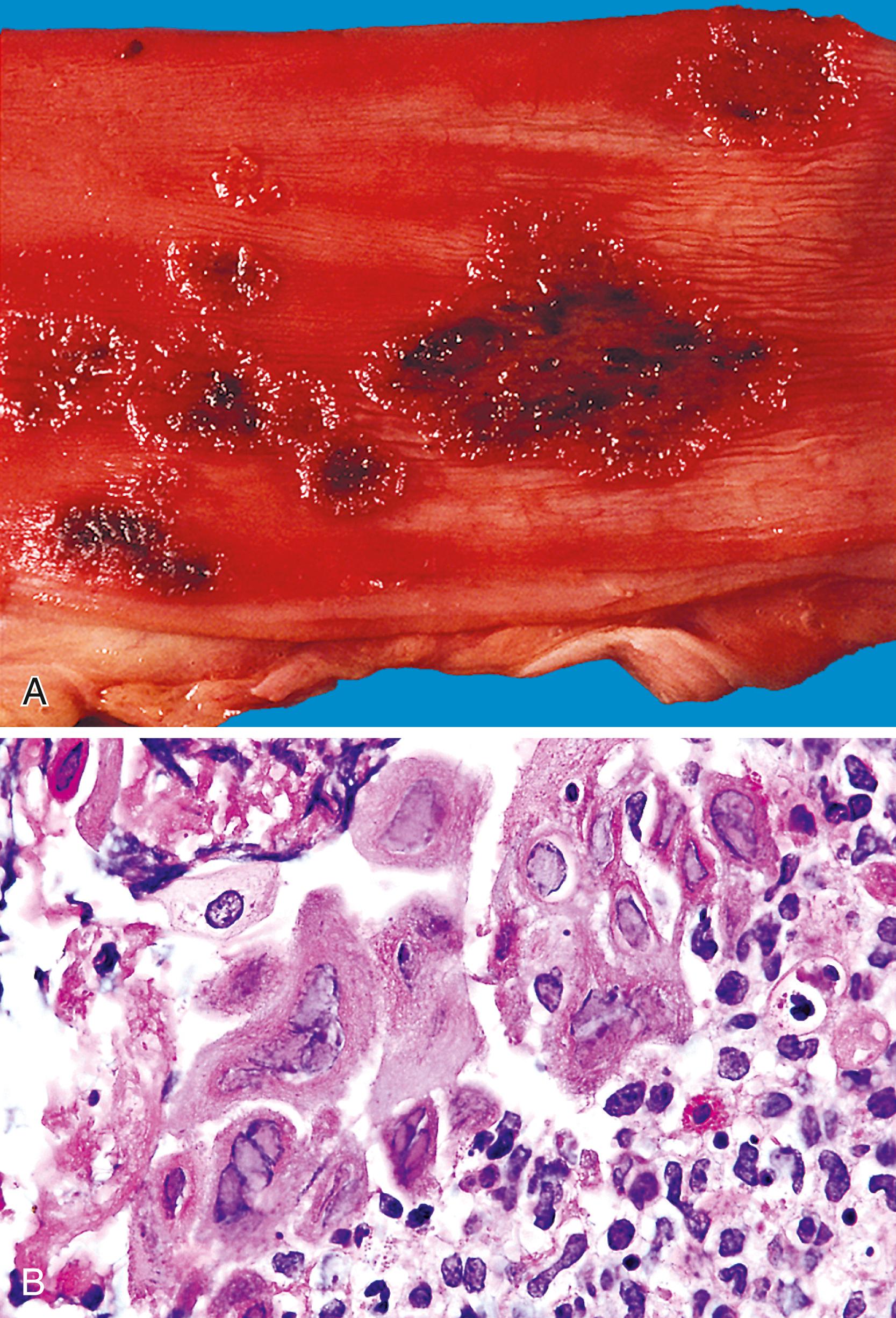
Gastric antral vascular ectasia (GAVE) affects mainly women of middle age, frequently causes iron-deficiency anemia, and is associated with portal hypertension/cirrhosis in about 30% to 40% of cases. It is sometimes associated with achlorhydria, atrophic gastritis, and CREST syndrome. Autoimmune disorders are present in approximately 62% of patients with GAVE. At endoscopy, GAVE is characterized by a linear pattern of mucosal hyperemia on the antral rugae that appears similar to the stripes of a watermelon; hence, the synonym, watermelon stomach ( Fig. 11.14 ). This endoscopic appearance tends to be more diffuse in cases of cirrhosis but usually involves only the gastric antrum. The pathogenesis of GAVE is believed to be altered gastric motility, but this has never been confirmed.

Histologically, GAVE is characterized by the presence of dilated capillaries in the mucosa and submucosa, often containing microthrombi, which represent the histological hallmark of this entity. Thrombi can be subtle on hematoxylin and eosin (H&E) stain. CD61 immunostain is a helpful diagnostic tool in some cases. Some studies have shown an increased number and caliber of mucosal vessels in GAVE in comparison with portal hypertensive gastropathy. Fibromuscular hyperplasia of the intervening lamina propria and focal hyalinosis are characteristic features, along with edema, congestion, and reactive changes of the foveolar epithelium , , ( Fig. 11.15A–C ). Inflammation is typically minimal. Surface erosion is uncommon.

In mucosal biopsies, both portal hypertensive gastropathy and GAVE should be distinguished histologically from chronic radiation gastritis, which also shows ectatic mucosal capillaries. In contrast, radiation injury is characterized by prominent endothelial cells and hyaline thickening of dilated capillaries and small blood vessels, sometimes associated with thrombosis ( Fig. 11.16 ). Features that differentiate portal hypertensive gastropathy from GAVE are summarized in Table 11.3 .

Endoscopic mucosal ablation and treatment of the underlying etiology are the main forms of treatment for most patients with GAVE. Antrectomy is reserved for patients with uncontrollable bleeding.
HHT, also referred to as Rendu-Osler-Weber disease, is an autosomal dominant condition in which telangiectases involve the mucous membranes of the oral cavity, but also any portion of the GI tract, where they may bleed. The disorder affects both sexes equally and occurs in all races. The typical clinical triad consists of telangiectasia (mucosal and/or visceral) and recurrent epistaxis in a patient with a family history of the disorder, such as in a first-degree relative. About 20% of patients do not reveal a family history of either telangiectasia or recurrent bleeding. Most patients express at least two of the following four manifestations: epistaxis, telangiectasia, visceral lesions (including GI telangiectasia), and a positive family history. At least 600 mutations, involving multiple gene loci ( ENG 61%, ACVRL1 37%, MADH4 ∼2%, rarely HHT3 and HHT4 ), have been implicated in HHT. GI bleeding is more likely in patients with HHT1/ENG mutations. Upper GI bleeding is common and can be difficult to distinguish from epistaxis; the two are the most common manifestations of HHT. GI bleeding is often difficult to control. Blood transfusion requirements in excess of 100 units have been reported in some patients.
GI tract lesions include telangiectases, arteriovenous malformations (AVMs), and angiodysplasias. Telangiectases, which are the most common lesions, appear grossly as bright red spots on the mucosa. They frequently involve the stomach and proximal small intestine. These lesions are composed of a tuft of dilated venules and arterioles that communicate directly with one another, thereby bypassing capillaries ( Fig. 11.17 ). The precise vascular architecture is often difficult to appreciate in routine histological sections, but evaluation of serial sections may help.

Telangiectasia may also occur in patients with scleroderma, as part of CREST syndrome. The morphology of telangiectases associated with scleroderma is similar to that in HHT, thus distinction therefore requires clinical and serological correlation (rheumatoid factor, antinuclear antibody, SCL-70 antibody, and anticentromeric protein antibody). Telangiectases may also develop in patients with chronic renal failure after hemodialysis.
Treatment options for GI hemorrhage associated with HHT include drug therapy with estrogen, danazol, or aminocaproic acid; endoscopic coagulation, cautery, or laser therapy; and surgical resection.
Lower GI tract bleeding refers to any type of bleeding from a source located distal to the ligament of Treitz. Hemodynamically significant bleeding from the lower GI tract is most commonly caused by colonic diverticula and angiodysplasia (angiectasia). Other causes are listed in Table 11.4 . Colorectal causes are more prevalent than small-intestinal causes. Chronic low-grade bleeding is often not visible to the patient. It may be detected only by fecal occult blood testing.
| Entity | Key Clinical Features | Key Pathological Features |
|---|---|---|
| Diverticular disease ∗ | Most frequent in elderly Accounts for 30% to 40% of cases of significant lower GI hemorrhage |
Most common in the sigmoid colon Thickened muscularis propria, exaggerated mucosal folds Pseudodiverticula extend through muscularis at points of entry of vasa recta Inflammation of diverticula may lead to vascular erosion and bleeding |
| Angiodysplasia ∗ | Common in elderly patients Chronic and recurrent bleeding Common cause of bleeding in renal failure |
Usually in right colon Dilated, tortuous, thin-walled submucosal veins, capillaries, and arterioles with arteriovenous anastomoses Most commonly submucosal; may involve mucosa |
| Arteriovenous malformation | Developmental defects, but may present at any age | Most common in sigmoid colon and rectum Arterialized veins with thick muscular walls are associated with a knot of tortuous, dilated veins and arteries |
| Dieulafoy lesion | See Table 11.2 | See Table 11.2 |
| Varices (rectal, stomal) | Associated with portal hypertension and mesenteric and splenic vein obstruction | Occur at portosystemic anastomoses in the rectum and at enterocolic-cutaneous stomas Histological features are similar to upper GI varices |
| Portal hypertensive colopathy | Seen in portal hypertension Strong association with cirrhosis, but no correlation with degree |
Dilated tortuous mucosal and submucosal capillaries correspond to red spots seen at endoscopy |
| Hereditary hemorrhagic telangiectasia | See Table 11.2 | See Table 11.2 |
| Hemodialysis-associated telangiectasia | See Table 11.2 | See Table 11.2 |
| Hemorrhoids | Common in adults, increase in prevalence after third decade | Dilated submucosal and mucosal blood vessels, usually with thrombosis and hemorrhage |
| Infections | See Table 11.5 | See Table 11.5 |
| Mucosal prolapse | History of prior lower GI tract trauma or surgery Diverticular disease |
Reactive, hyperplastic mucosa with fibromuscular lamina propria and architectural distortion |
| Meckel’s diverticulum | GI bleed most common presentation in children | True diverticulum on antimesenteric border of ileum Heterotopic oxyntic mucosa with peptic ulcer in 65% |
| Stercoral ulcers | Acute GI bleed in elderly patients Typically a history of constipation Common in renal patients treated for hyperkalemia |
Sharply demarcated ulcers in rectosigmoid, formed as pressure sores caused by hard feces High risk of perforation |
| Ulcerative colitis | Intermittent rectal bleeding, bloody diarrhea, and abdominal pain | Typically continuous colonic involvement proceeding proximally from the rectum with crypt architectural distortion, lymphoplasmacytic infiltrate, basal plasmacytosis, cryptitis, crypt abscesses, and ulceration |
| Crohn’s disease | More variable symptoms than ulcerative colitis, including abdominal pain, fatigue, weight loss, and fever | Typically patchy transmural involvement of small and/or large bowel by deep ulcers, mural fibrosis and lymphoplasmacytic inflammation with reactive lymphoid follicles, variable degrees of architectural distortion, pyloric gland metaplasia, and cryptitis and crypt abscesses, with or without granulomas |
| Ischemic enterocolitis | See Table 11.9 | See Table 11.9 |
| Radiation enterocolitis | History of prostate cancer common in men; cervical cancer common in women Rare cause of lower GI bleeding |
Dilated, tortuous mucosal capillaries with prominent endothelial cells in mucosa Hyalinized vessels with prominent endothelial cells, stellate fibroblasts, and fibrosis in submucosa |
| Collagenous colitis | Watery diarrhea Female predominance: 4:1 Rare cause of lower GI bleeding |
Marked thickening of the subepithelial collagen table with entrapment of inflammatory cells and capillaries; subepithelial collagen may mimic hyalinosis of ischemic colitis |
| Diversion colitis | History of previous bowel resection with fecal stream diversion May cause bloody rectal discharge |
Friable mucosa with normal or distorted architecture, mucin depletion, bandlike lymphoplasmacytic infiltrate most dense in the upper mucosa, rare cryptitis, Paneth cell metaplasia, and prominent reactive lymphoid follicles |
| Diaphragm disease | History of NSAID use | Transverse stenosing membrane composed of submucosa lined on both sides by mucosa, with central aperture |
| Ehlers-Danlos syndrome, vascular type | Acute hemorrhage and bowel perforation in young patients resulting from deficiency of collagen type 3 | Most commonly affects the sigmoid colon Thinned muscularis propria and diminished submucosa Proliferating fibroblasts surrounding fat Frayed, degenerated vascular and stromal collagen |
Lower GI bleeding occurs most commonly in the seventh decade of life. Although it is five times less common than upper GI bleeding, patients with lower GI bleeding are more likely to require surgery. The most common clinical presentation of patients with lower GI bleeding is passage of bright-red blood per rectum (hematochezia). Similar to upper GI bleeding, lower GI bleeding may result in melena, anemia, or hemodynamic instability. Investigative modalities useful for identification of the source of lower GI bleeding include colonoscopy, angiography, nuclear scan, barium enema, and push enteroscopy.
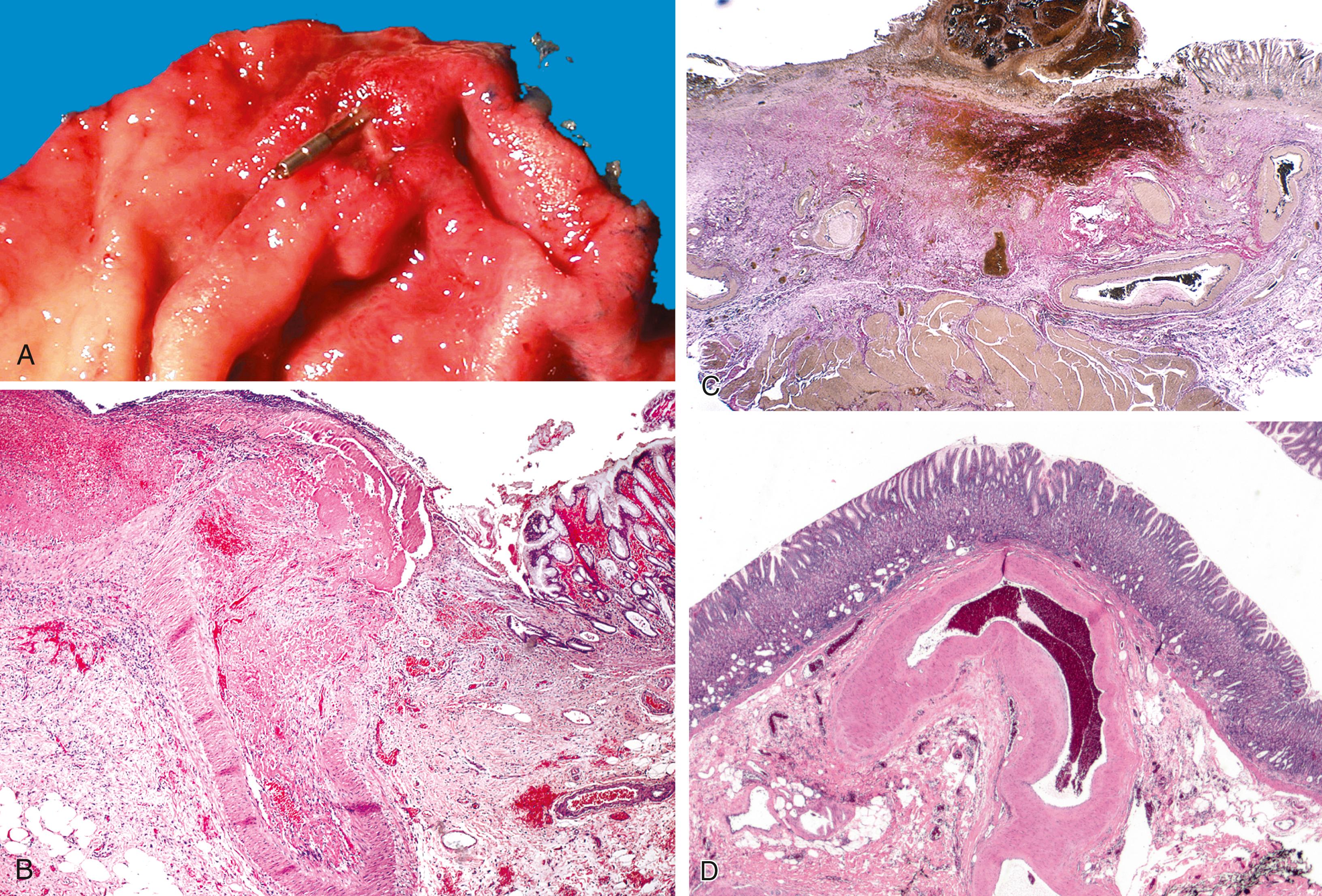
Diverticulosis accounts for 30% to 40% of cases of significant lower GI hemorrhage. Bleeding occurs in up to 15% of patients with diverticular disease, and is often associated with NSAID use, hyperuricemia, or cerebrovascular disease. Left-sided diverticula are defined as acquired outpouchings of the colonic mucosa that protrude through the muscularis propria, typically at the points of entry of the vasa recta ( Fig. 11.18A–C ). They are usually situated in intimate contact with penetrating blood vessels, where inflammation and ulceration of diverticula can lead to erosion of the vessel wall and bleeding. Diverticular bleeding may be slow and chronic if venous in origin, or acute and severe if an artery is involved. Right-sided diverticula are not usually associated with penetrating vessels. GI bleeding in Meckel’s diverticula is usually from foci of gastric heterotopia that cause peptic ulceration of the adjacent mucosa ( Fig. 11.19 ).


Most episodes of bleeding caused by colonic diverticula resolve spontaneously. However, up to one-third of patients require transfusion or therapeutic intervention. Treatment options include contact coagulation, epinephrine injection, hemoclip application, fibrin sealant, and surgical resection.
Angiodysplasia (angiectasia) is the second most common cause of lower GI bleeding in elderly patients (>70 years of age). Angiodysplasia is characterized by the presence of a cluster of abnormally dilated blood vessels in the mucosa and submucosa of the lower GI tract. Bleeding from angiodysplasia is usually chronic and recurrent, but massive hemorrhage occurs in approximately 10% to 15% of affected patients.
Angiodysplasia is an acquired lesion associated with aging. It has an overall incidence of 0.8% in screening populations. Angiodysplasia results from dilated preexisting venules, thus they are not considered true malformations. The majority of cases occur in the right colon (80%), and 10% to 15% occur in the small intestine. Although usually readily seen at colonoscopy and angiography, angiodysplasia is often difficult to detect on gross examination of a resection specimen without the use of specific injection techniques. By performing vascular injection studies of resected colons, Boley and Brandt determined that angiodysplasia develops as a result of intermittent partial obstruction of small veins that drain the colonic mucosa and submucosa as they course through the muscularis propria. They postulated that obstruction is caused by muscle contraction and increased tension within the bowel wall, which is highest in the region of colon with the greatest diameter (i.e., the cecum). With time, obstruction of the penetrating veins in the muscularis propria leads to dilation and tortuosity of the submucosal veins and, consequently, the venules and capillaries that drain them. Dilation of capillaries ultimately leads to loss of capillary sphincter function, which creates arteriovenous fistulas and secondary effects on the structure of the feeding arteries.
Angiodysplasia is often difficult to diagnose in pathological specimens. In resection specimens examined in the fresh state, one may see only small (usually 1 to 5 mm) focus of enhanced vascular markings and erythema, and even these subtle signs may be absent. Lesions can be multiple and be associated with surface erosion. In specimens examined after formalin fixation, the lesions are usually not visible on the mucosal surface. Few laboratories are equipped to perform injection studies, which require processing of fresh specimens. With fixed resection specimens, slicing the bowel wall with a sharp blade at the site of suspected mucosal abnormalities helps reveal the lesion. If a vascular lesion is detected, histological examination usually reveals a discrete cluster of dilated, thin-walled tortuous veins and venules within the submucosa ( Fig. 11.20A ), and some associated with dilated capillaries in the overlying mucosa as well ( Fig. 11.20B–D ). In long-standing disease, there may be arterialization of veins. Occasional enlarged arteries may be noted.

Diagnosis of angiodysplasia in biopsy specimens is usually problematic. The main histological component of angiodysplasia is normally situated in the submucosa, which may not be sampled in superficial endoscopic biopsies. When capillary dilation involves the mucosa, biopsy specimens may show only one or two ectatic capillaries, and these may collapse when the specimen is immersed in formalin. In more advanced lesions with more extensive mucosal involvement, clusters of dilated capillaries may distort the architecture of the mucosa, displacing glands and separating the crypts from each other ( Fig. 11.21 ).

In most instances, bleeding can be controlled adequately by medications and therapeutic endoscopy. Angiographic techniques not only enable precise localization of angiodysplasia but also allow for treatment by superselective embolization. Surgical resection is reserved for patients with uncontrolled bleeding.
In contrast with angiodysplasia, which is an acquired lesion that develops mainly in elderly, AVMs develop during embryological or fetal life and are typically present at birth. AVMs also differ from angiodysplasia in that the former results in an abnormal direct communication between arteries and veins. Because of this communication, arterial blood flows directly into the venous system at higher-than-normal pressures, bypassing the (high-resistance) capillary bed. AVMs can manifest clinically with bleeding at any age.
In the GI tract, AVMs occur most often in the sigmoid colon and rectum, and they are usually located external to the muscularis propria—that is, in the subserosa ( Fig. 11.22 ). The malformation usually consists of a tangled mass of tortuous, variably dilated arteries, veins, and vessels with intermediate characteristics. Veins in AVMs undergo “arterialization” in response to exposure to elevated (arterial) blood pressure. They develop a thick, muscular wall as a result of myointimal hyperplasia ( Fig. 11.23 ). It has been proposed that idiopathic myointimal hyperplasia of the mesenteric veins (discussed later) is an example of venous arterialization as a complication of AVM. Histologically, AVMs are characterized by the presence of a complex cluster of tortuous, dilated vascular channels and vessels that appear intermediate in structure between arteries and veins. The vascular architecture is more easily depicted by angiographic studies.


Most AVMs of the GI tract are treated angiographically by superselective embolization. Large lesions may require surgical resection.
Hemorrhoids are very common. Clinically, most patients present in middle age with anal pain or bleeding. Hemorrhoids arise from the anal cushions, which are normal anatomic structures of the anorectal canal. The anal cushions are composed of tufts of anastomosing arterioles and venules in the submucosa; they are embedded within compact, dense, submucosal collagenous and elastic fibrous stroma and covered by anorectal mucosa. Hemorrhoids develop as a result of degenerative changes that occur in the supporting stroma or as a result of locally increased intravascular pressure, or both. The blood vessels become engorged and the cushions prolapse, strangulate, thrombose, ulcerate, and bleed. Histological sections of hemorrhoids show tufts of engorged, dilated veins and arteries often associated with thrombi and hemorrhage, in a dense stroma, covered by anal or rectal mucosa, which is often ulcerated ( Fig. 11.24 ). In case of prolapsed hemorrhoidal tissue, the pathology specimen can include fibers of smooth muscle (part of the rectum muscularis propria and/or internal anal sphincter muscle) without significant clinical implications in most cases. It is extremely rare to see striated muscle in this setting as it denotes portions of external anal sphincter muscle within the specimen and a higher risk for postoperative complications. Treatment options for hemorrhoids include dietary modification, sclerotherapy, photocoagulation, diathermy, banding, laser ablation, cryotherapy, and surgical hemorrhoidectomy.

Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here