Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The topic vascular diseases of the liver encompasses an array of disparate clinicopathologic entities, with the common thread that they specifically affect the hepatic vasculature. They can be arbitrarily classified into those that involve the hepatic artery and its branches, those that involve the portal vein, and those that involve the hepatic veins. The topics portal hypertension and portal vein thrombosis are addressed separately in Chapter 135 .
Hepatic artery aneurysms are rare, comprising approximately 20% of all visceral aneurysms. True aneurysms may be a manifestation of systemic diseases, including atherosclerosis or vasculitides such as polyarteritis nodosa and systemic lupus erythematosus. Pseudoaneurysms of the hepatic artery can result from hepatic trauma, iatrogenic, surgical injury to the artery, or rarely as a sequela of acute pancreatitis. Mycotic pseudoaneurysms resulting from bacterial endocarditis or following liver transplantation have also been reported.
Most commonly, hepatic artery aneurysms are solitary, involve the extrahepatic portion of the artery, and are 3 to 4 cm in diameter at the time of presentation. The clinical presentation varies considerably. Some are discovered incidentally by noninvasive imaging studies ( Fig. 129.1 ). Patients with mycotic pseudoaneurysms may present with pain, fever, or other signs of infection. Hemobilia following laparoscopic cholecystectomy, liver biopsy, or interventional radiologic procedures can result from rupture of a pseudoaneurysm into the biliary tree. Intraperitoneal or gastrointestinal hemorrhage–related rupture is associated with a high mortality rate.
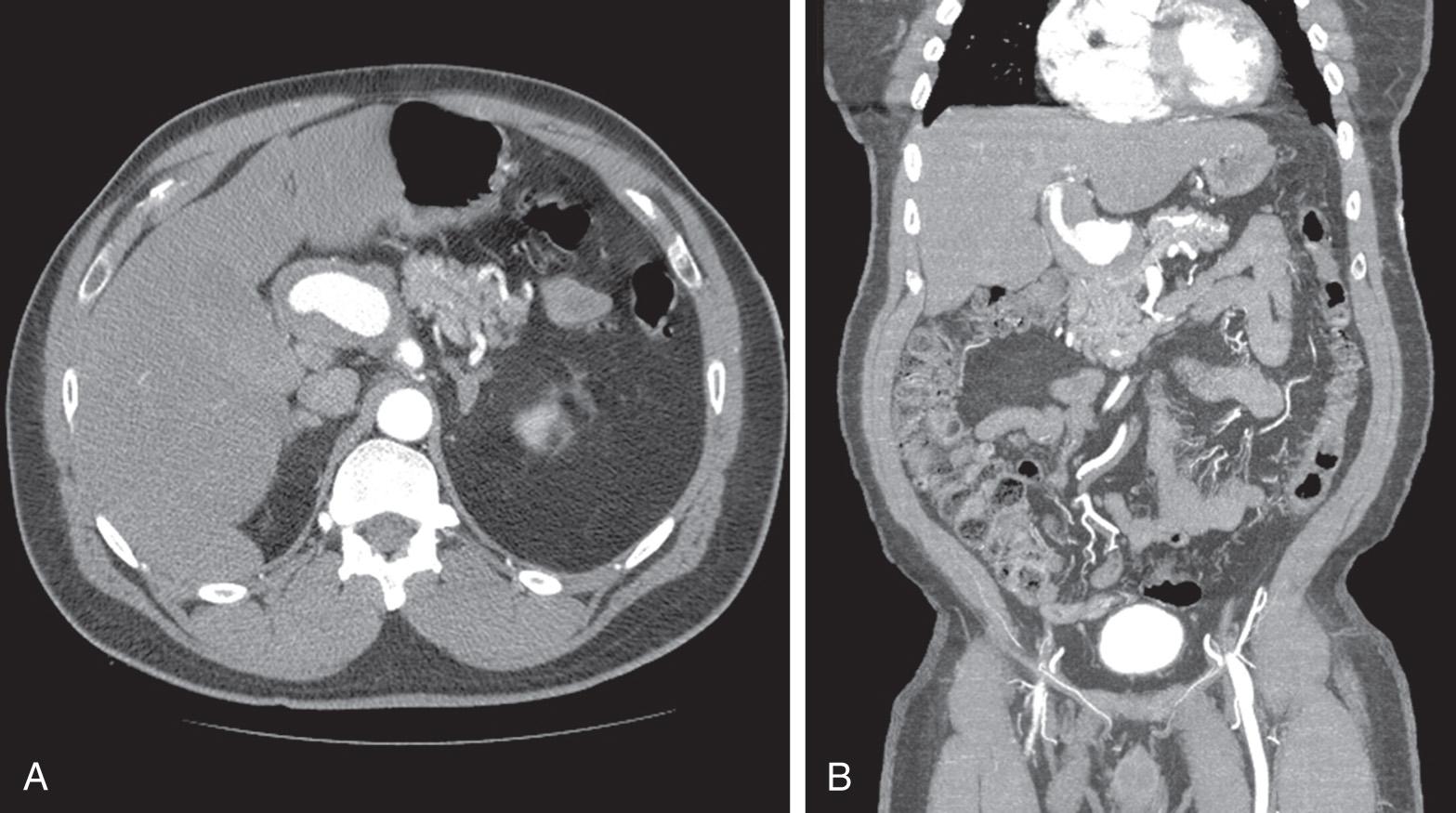
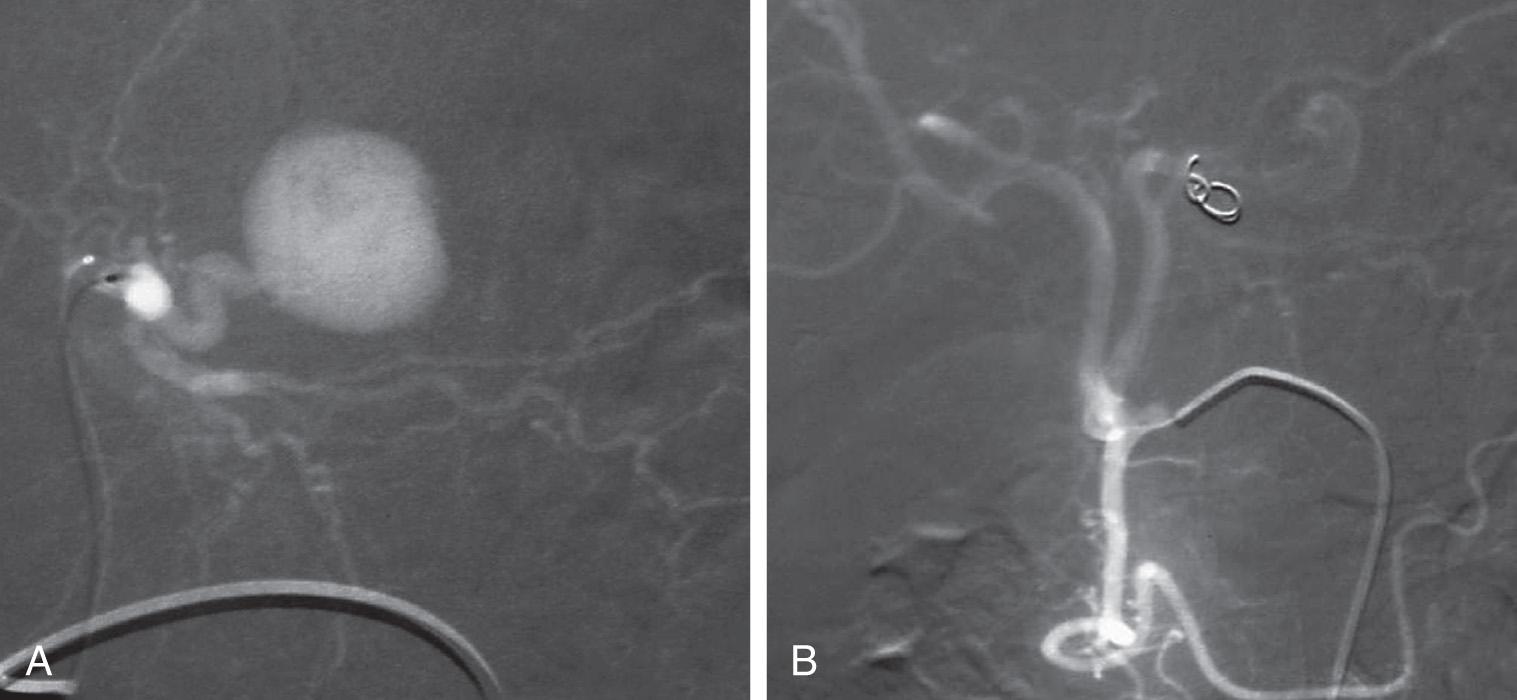
The diagnosis may be suspected based on the presentation but is confirmed by Doppler ultrasonography, intravenous contrast–enhanced computed tomography (CT), or magnetic resonance (MR) imaging. Angiography can be diagnostic, and with the aid of endovascular techniques, can be therapeutic as well.
The treatment of hepatic artery aneurysms is dictated by their cause, size, location, and patient condition. Although the natural history of these aneurysms is unclear, it seems that size correlates with the risk of rupture. In addition, the ubiquitous use of high-quality imaging techniques has led to an increased detection of small, asymptomatic aneurysms. The concern of eventual complications, especially hemorrhage, warrants the consideration of treating all of these lesions, even those that are asymptomatic or are discovered incidentally. Underlying conditions must be recognized and addressed, and adequate resuscitation is required for patients presenting with intraperitoneal or gastrointestinal hemorrhage.
Aneurysms of the extrahepatic portion of the artery are classically managed surgically. Despite advancements in endovascular technology, open repair remains the mainstay of treatment. Those affecting the common hepatic artery may be ligated proximally and distally if adequate collateral circulation to the liver is afforded by the gastroduodenal artery via the pancreaticoduodenal arcade. Those originating distal to the gastroduodenal artery, affecting the proper hepatic artery, can be treated by aneurysmectomy and revascularization of the liver.
A pseudoaneurysm of the hepatic artery following liver transplantation at the site of the arterial anastomosis is a serious complication. The usual treatment is resection of the pseudoaneurysm and revascularization of the liver. In an emergency, ligation of the artery proximally and distally may be the only option but is associated with a high likelihood of graft loss. Urgent retransplantation may be necessary.
Intrahepatic aneurysms can be managed by percutaneous transarterial catheter embolization ( Fig. 129.2 ). This approach is especially useful if the lesions are multiple, as seen in cases of polyarteritis nodosa. The risk of significant hepatic ischemia is minimized if there is adequate portal venous blood flow and the affected artery branch or branches are distal within the liver. Solitary, posttraumatic intrahepatic pseudoaneurysms, confined to a hepatic segment or lobe, may be treated by hepatic resection if an endovascular approach is not possible.
Traumatic injury of the hepatic artery is uncommon. Penetrating injuries to the portal triad outnumber blunt injuries, and associated injuries are the rule. The diagnosis is usually made at the time of laparotomy or postmortem. Portal triad injuries carry a high mortality rate because of exsanguinating hemorrhage or refractory shock. Successful treatment requires control of bleeding, aggressive resuscitation, and temporization of other injuries. Often concomitant biliary tract and/or portal vein injury must be addressed. Treatment options for the injured artery include ligation or primary repair. Better survival has been reported with hepatic artery ligation as compared with repair. The late sequelae of portal triad injuries, including hepatic ischemia, biliary strictures, portal hypertension, and liver failure, may mandate liver transplantation.
Iatrogenic injury of the hepatic artery is an uncommon but potentially devastating complication of laparoscopic cholecystectomy. Approximately one-fifth of cholecystectomy-related bile duct injuries have an associated hepatic artery injury, usually the right hepatic artery. The addition of an injury to the artery was thought to portend a higher complication rate after biliary reconstruction and a greater risk of mortality. A more recent literature review does not confirm the association between a concomitant arterial injury and failure of biliary repair. The injury is often not recognized at the time of surgery, even if the biliary injury is identified and corrected immediately. In the patient presenting with bile duct strictures after cholecystectomy, the presence of a concomitant arterial injury should be suspected based on the severity of the bile duct injury and the discovery of a report of difficulty gaining hemostasis during the cholecystectomy. The treatment of these injuries is usually directed toward repairing the bile duct endoscopically by primary repair or by Roux-en-Y hepaticojejunostomy. Arterial reconstruction, except when the injury is noted immediately, is seldom indicated or performed. Rarely, an injury to the right hepatic artery results in acute necrosis of the right hepatic lobe or intrahepatic strictures amenable to hepatic resection.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here