Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Soft tissue and vascular complications related to spinal surgery are usually predictable and vary depending on the region being operated upon.
Cervical spine surgery–related soft tissue complications frequently include dysphagia, hoarseness, and vocal fold motion impairment. Less frequent is vascular injury. Otorhinolaryngological consultation is particular useful in addressing these soft tissue complications. Vascular injury is often approached with the assistance of vascular surgery or interventional radiology.
Thoracic and lumbar spinal procedures can result in serious adjacent tissue injuries and catastrophic vascular injury. Complications can be avoided by understanding the relevant anatomy, avoiding past-pointing with instrumentation, and being conscientious of a complication early on. Vascular injury must be addressed early after its occurrence.
Screw insertion and hardware implantation may result in acute complication but also delayed complication, especially in the setting of pseudarthrosis or infection.
Minimally invasive spine procedures carry unique complication profiles related to the anatomic corridors and instrumentation used.
Drs. Neel Anand, Eli M. Baron, and Donald A. Smith updated this chapter on Vascular and Soft Tissue Complications originally authored by David W. Cahill for the first and second editions of this textbook. Dr. Cahill perished tragically in 2003 at the height of his career. He had extensive personal acquaintance both with the successes of surgery and with its complications. Ambitious, brilliant, and unapologetically self-confident, he bootstrapped himself to become a largely self-created neurosurgical pioneer in the evolving field of complex and reconstructive spine surgery. He only half-jokingly referred to himself as a “maximally invasive surgeon,” content not merely to perform cutting-edge deformity corrections, but ultimately coming to do all his own retroperitoneal and transcavitary approaches as well.
Dr. Cahill held himself and others to the highest personal and technical standards. He was bluntly honest in dispensing his opinions and rarely in doubt. Although this habit was not endearing to all, it was refreshing to hear such plain talk from someone in the know. David’s knack for critical thought and openness to challenge have been fittingly memorialized in the highly popular Cahill Controversies in Spine Surgery debates featured annually at meetings of the Joint Section.
Above all else, David was a devoted husband and parent. Within the professional arena his proudest professional achievements were the establishment of a Neurosurgical Spine Fellowship and a fully accredited Neurosurgical Residency at the University of South Florida, where he was also the founding chair for the Department of Neurosurgery. He personally graduated over 20 fellows and residents who are the daily renewal of his legacy to our profession. — Donald A. Smith
The simplest and most direct ventral access to the craniovertebral junction is the transoral/transpharyngeal approach. Many different variations of this operation have been described, including combined resection of the hard palate, median labiomandibular glossotomy, maxillectomy, and LeFort osteotomies to expand the exposure from the midclivus to the C3 level. The main limitation of these procedures is the inevitable contamination of the wound by mouth flora. Additionally, the location of the vertebral arteries limits the lateral extent of these procedures. By reserving these approaches for extradural pathological conditions and using perioperative antibiotics, many of the septic complications that were initially encountered with this operation have been overcome. Airway management in transoral procedures demands special attention. Significant tongue swelling is often encountered, and this can easily lead to obstruction of the oropharynx. In cases of major resections or those in which the patient has any preoperative difficulty with swallowing or aspiration, a tracheotomy is routinely performed. In more limited operations at the C1‒C2 level and without concurrent lower cranial neuropathy, the patient may be left intubated for 48 to 72 hours postoperatively or until glossal swelling has abated. Periodic relaxation of the intraoral retractors during surgery may mitigate the problem. Additionally, precautions should be taken to ensure that the tongue is not trapped between the retractor blade and the lower teeth. Steroids are often invoked as well, but they are no substitute for controlled extubation in an intensive care unit setting by someone who is skilled in airway management. Close observation with a bedside tracheostomy setup is mandatory. Although intradural procedures and bone grafting can be successfully performed through this route, these maneuvers carry a heightened risk and can be the source of significant morbidity. A layered, tensionless reapproximation of the dorsal pharyngeal musculature and mucosa with resorbable sutures is important, especially if the dura mater has been violated. In this case, reinforcement of the dural repair with a fascial graft and fibrin glue and placement of a spine drain postoperatively are advised. If bone grafts or reconstructive cages have been inserted, they should have a low profile, without protrusion into the pharynx and resultant compromise of the soft tissue closure. Because the retropharyngeal soft tissues are well vascularized, surgeons tend to use electrocautery to divide and reflect these structures off the bone. This can result in significant retraction of the wound margins, which becomes most apparent at the time of closure. Infiltration of the retropharyngeal tissues with a dilute epinephrine solution before sharp incision and blunt reflection with the use of bipolar cautery for direct hemostasis minimize this problem. If a primary closure cannot be obtained (or if one should subsequently break down), satisfactory repair can usually be achieved with either a pharyngeal or a septal flap reconstruction. When the soft palate has been divided, a similar degree of attention should be devoted to the tensionless anatomic reapproximation of its edges, so that a cleft or fistula does not result. In the immediate postoperative period, oral feedings should be avoided for the first 5 days to minimize risk of fascial dehiscence.
Vertebral artery injury is always a theoretical risk during these procedures. At the arch of C1, the vertebral arteries are located approximately 24 mm laterally from the midline; at the level of the foramen magnum and the level of the C2‒C3 disc space, the arteries are approximately 11 mm from the midline. Pathology such as rotatory subluxation can significantly distort the relationship of these structures to the midline. Identification of the midline structures, such as the anterior tubercle of C1 and the pharyngeal tubercle on the clivus, are the most important steps in establishing orientation for these approaches. Furthermore, the anatomic midline can be identified by the symmetry of the anterior longitudinal ligament and longus colli muscles. Fluoroscopy is also useful in establishing the midline, as may be intraoperative neuronavigation. Regarding management of vertebral artery injury, please see the next section.
The ventrolateral approach to the subaxial spine, as popularized by Robinson and Smith, is among the most commonly performed spine surgeries. The esophagus, larynx, and trachea are mobilized medially as a unit, and the carotid sheath is retracted laterally. The incidence of clinically significant injuries to these structures is low during primary surgeries. When an injury does occur, sharp-toothed retractors are often implicated. Handheld blunt retractors are used exclusively until the musculus longus colli have been reflected off the vertebral bodies ventrolaterally to create two soft tissue leaves into which a self-retaining retractor system can be anchored. Great care is taken with the initial placement of retractors because this permits safe, stable, and sustained exposure that sets the stage for the remainder of the case. Toothed blades are inserted accurately under the musculus longus colli under direct vision. Proper engagement of the muscles usually requires the use of asymmetrical blade lengths, the medial blade being a bit longer.
The cervical sympathetic chain overlies the musculus longus colli more laterally. Occasionally Horner syndrome ensues after reflection of these muscles or because of heat transmission from electrocautery. This is usually transient and is not functionally disabling. Other structures that are at potential risk are the recurrent laryngeal nerve and the vertebral arteries. Injuries to the thoracic duct are occasionally incurred in left-sided approaches at the C6‒C7 and C7-T1 levels; these are reviewed separately in the following sections.
Vocal cord paresis is a complication in anterior cervical surgery that is probably underappreciated. In patients who have undergone the anterior cervical approach to the spine for discectomy or corpectomy, the reported rate of injury varies from 0% to 16%. Nevertheless, a prospective study looking at 120 patients undergoing anterior cervical spine surgery who underwent preoperative and postoperative laryngoscopy revealed a clinically symptomatic recurrent laryngeal nerve palsy rate of 8.3%, and the incidence of recurrent laryngeal nerve palsy not associated with hoarseness (i.e., clinically unapparent without laryngoscopy) was 15.9% (overall incidence, 24.2%). At 3-month follow-up evaluation, the rate had decreased to 2.5% in cases with hoarseness and 10.8% without hoarseness. Most of these are blunt injuries, believed to have resulted from retractor pressure against the recurrent laryngeal nerve within the tracheoesophageal groove. The left recurrent laryngeal nerve has a longer course, swinging around the aortic arch before ascending in the relatively protected cleft between the trachea and esophagus, whereas the right recurrent laryngeal nerve loops around the subclavian artery, and thus has a correspondingly shorter course. The extra length of nerve available on the left allegedly renders it less vulnerable to stretch injury than its counterpart on the right, but the evidence for this is scant. A recent prospective study assessed 242 patients undergoing anterior cervical spine surgery postoperatively with laryngoscopy. All patients underwent a left-sided approach, but one group (149 patients) was operated on with an additional reduction of endotracheal cuff pressure to below 20 mm Hg. Some 93 patients underwent a left-sided approach without reduction in cuff pressure. In the group with the left-sided approach and the low cuff pressures, the total rate of persisting (at 3 months) symptomatic and asymptomatic recurrent laryngeal nerve palsy was 1.3%. In the group with the left-sided approach without the reduced cuff pressures, the total rate of persisting (at 3 months) symptomatic and asymptomatic recurrent laryngeal nerve palsy was 6.5%. The authors noted that this compared favorably with their historic data, in which they noted a total rate of persisting recurrent laryngeal nerve palsy of 13.3% in patients undergoing the right-sided approach without reduction of cuff pressure.
In cases of suspected vocal fold motion impairment, an otorhinolaryngology consult should be obtained. Initial evaluation should include a detailed history with the patient relating symptoms and their time of onset, followed by a physical examination, in which particularly close attention is paid to the neck, and a neurological examination of the lower cranial nerves. This should be followed by visualization of the vocal cords with a fiberoptic laryngoscope. Also very valuable is a videofluoroscopic swallowing evaluation. This can show signs of pharyngeal plexus injury, such as disruption of velar movement, cricopharyngeal spasm, and other patterns of swallowing dysfunction. If there is an immobile vocal cord, a useful examination tool is laryngeal electromyography. Laryngeal electromyography can help in determining the site of a peripheral vagal lesion (high cervical vs. low cervical), as it allows separate testing of laryngeal muscles supplied by the recurrent laryngeal and superior laryngeal nerves. Laryngeal electromyography also allows for differentiation between vocal cord paralysis and vocal cord fixation.
As a rule, functional recovery occurs over a period of weeks to months. Nevertheless, injury may be permanent or slow to heal, and surgical intervention may be required. Various options exist for the treatment of unilateral vocal fold paresis and paralysis. These include injection laryngoplasty, medialization laryngoplasty, arytenoid adduction, and nerve-muscle transfer. Injection laryngoplasty may be performed with hemostatic gelatin (Gelfoam), fat, collagen, or Teflon (El Du Pont de Nemours & Co., Inc., Wilmington, DE). Medialization laryngoplasty is usually performed with silicone elastomer (Silastic) or hydroxylapatite. More recently, novel materials such as titanium, GORE-TEX (W. L. Gore and Associates, Inc., Flagstaff, AZ), and polylactic/polyglycolic acid have been used. Arytenoid adduction uses a permanent suture to relocate the arytenoid into a more physiologically sound position. ,
Transient swallowing disorders are commonly recorded after even uncomplicated primary anterior cervical surgeries. They may be seen in up to 80% of patients who undergo anterior cervical spine surgery. Symptoms usually resolve within a few weeks but may persist in up to 10% of patients, although only rarely at a level that is functionally disabling. Refractory cases should be evaluated with videofluoroscopic swallowing evaluation (modified barium swallow) to determine the integrity of the swallowing mechanism and whether the patient will safely tolerate oral intake. This then can expedite appropriate swallowing therapy and an appropriate route for nutrition. , Although many patients will do well, recovery, presumably through reinnervation of pharyngeal musculature, does not always occur. The speech pathologist can be of tremendous help here in determining the patient’s potential for recovery. If the dysphagia is related to cricopharyngeal spasm and lasts several months, and follow-up study does not show improvement with conservative therapy, surgical intervention such as cricopharyngeal myotomy may be considered.
Although the U.S. Food and Drug Administration (FDA) issued a warning letter regarding its use in the anterior cervical spine in 2008, bone morphogenetic protein still remains widely used in this setting. It has been associated with a significant risk increase for dysphagia, dysphonia, hematoma, and neurological complications. Its use in the anterior cervical spine has thus been questioned.
Esophageal perforation is a much more serious problem than dysphagia. Most of these injuries occur in the context of reoperative surgery or surgery performed for infection, for tumor, or after irradiation. Tissues are fibrotic and sometimes friable, and tissue planes are often scarred, distorted, and unyielding. Blunt mobilization of the esophagus off the prevertebral fascia might not be successful, and sharp dissection can be equally hazardous. Passage of a nasogastric tube that can be palpated within the esophageal lumen serves as a further point of orientation and as an aid to dissection. A combination of blunt and sharp techniques may be useful for dissecting the junction between the ventral aspect of the vertebral bodies and the overlying soft tissue structures as precisely as possible. If normal planes of dissection are not apparent, exposure is extended rostrally and caudally in search of recognizable anatomy in more virginal tissues. This may enable definition of the lateral margin of the vertebral corpus concealed beneath swollen musculus longus colli. The prevertebral fascia can then be incised in a paramedian plane down to bone, and the fascia and overlying laryngotracheal esophageal bundle can be mobilized as an undissected unit. Depending on the quality of the tissue planes that are developed in this fashion, the use of any form of toothed retractor should be avoided. In reoperative cases, some of these difficulties may be averted altogether simply by approaching from the side opposite the initial procedure. In this case, direct laryngoscopy should be performed preoperatively or at intubation to confirm preserved vocal cord function on the initially operated side, thereby precluding the catastrophic outcome of bilateral vocal cord paralysis at the second procedure.
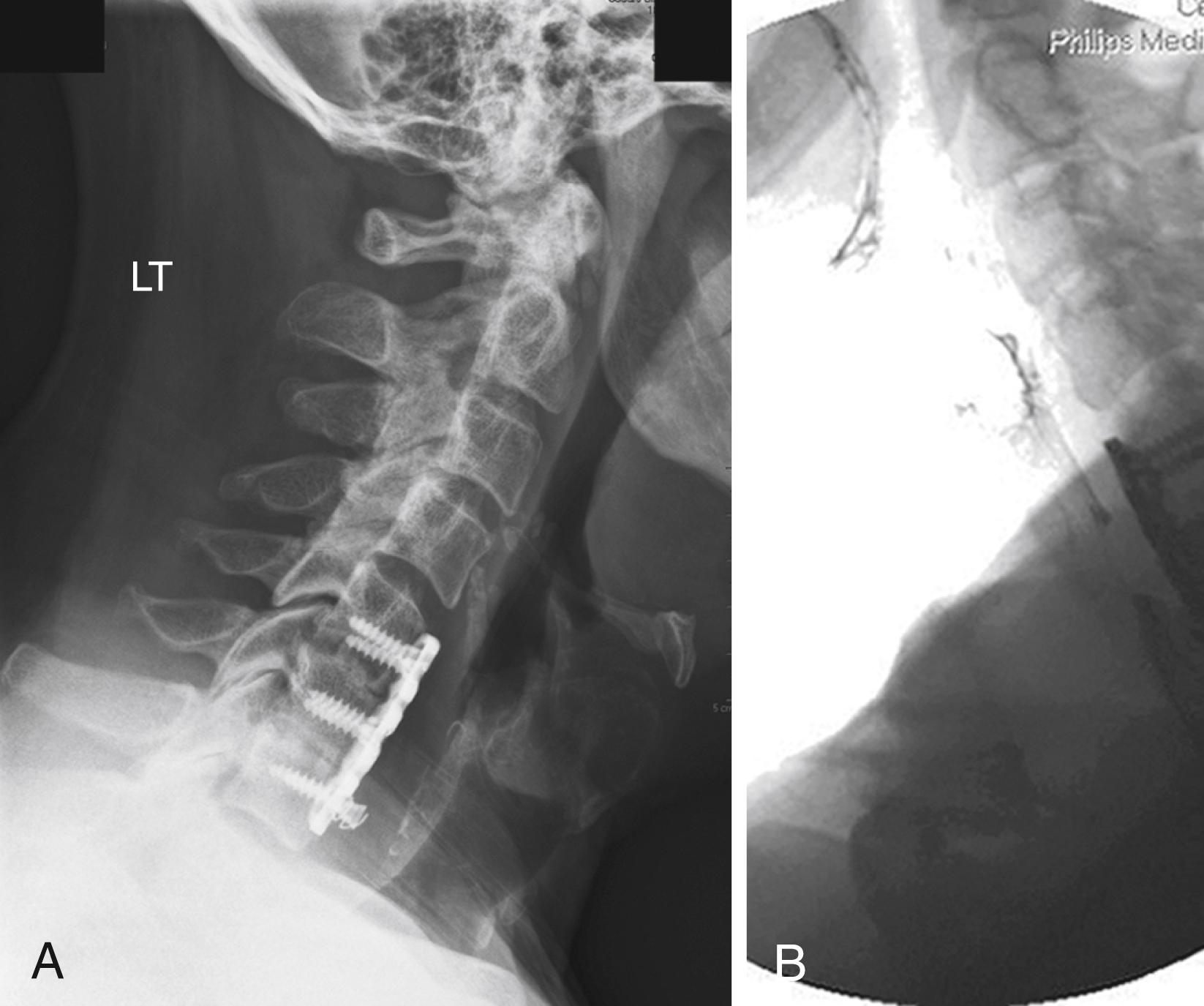
Esophageal perforation is also encountered as a delayed complication associated with ventral graft extrusion and hardware failure. This occurs most commonly because of infection, poor carpentry, a technical error in the method of instrumentation, or application of instrumentation in softened osteoporotic bone. This can also occur in the setting of pseudarthrosis ( Fig. 96.1 ). When screws are observed to back out in follow-up radiographs, their elective removal should be considered. There are now abundant reports of esophageal injury secondary to screw migration. Additionally, instrumentation may even be missing because it can pass through the gastrointestinal tract after fistula formation. Screw heads should be flush with the plate to minimize their profile and allow their locking mechanism to function properly to prevent backout. Plate length must be selected carefully so that there is no overhang over adjacent disc spaces, and unfused segments should not be instrumented, because these circumstances promote hardware loosening. If the quality of the bone stock is poor, bicortical screw fixation should be used. If this is not feasible, posterior segmental instrumentation should be performed.
Esophageal perforation may be apparent intraoperatively, but more often it presents postoperatively with deep wound infection, severe dysphagia, and mediastinitis. , Perforation related to hardware failure might not occur until years after the operative procedure. , Intraoperative tears may be either partial or full thickness. A partial-thickness injury to the esophagus is readily repaired with resorbable sutures and should not cause modification of the primary procedure. To ensure that a transmural injury has not occurred, the surgeon may instill indigo carmine dye into the hypopharynx and monitor for dye egress within the wound. Transmural injuries are repaired primarily, again with the surgeon observing the principles of a layered, tensionless closure using resorbable sutures. The wound is irrigated copiously with antibiotic-containing solution, and systemic antibiotic coverage is broadened to include anaerobic organisms. Assuming an absence of gross contamination and a satisfactory repair, the surgeon can proceed with the intended decompression and fusion in most instances. In these circumstances, any form of spine instrumentation should be used with caution. The patient is fed through a Silastic feeding tube during the first postoperative week. Intravenous antibiotics are continued for 2 to 6 weeks postoperatively. A further course of oral antibiotics thereafter is discretionary.
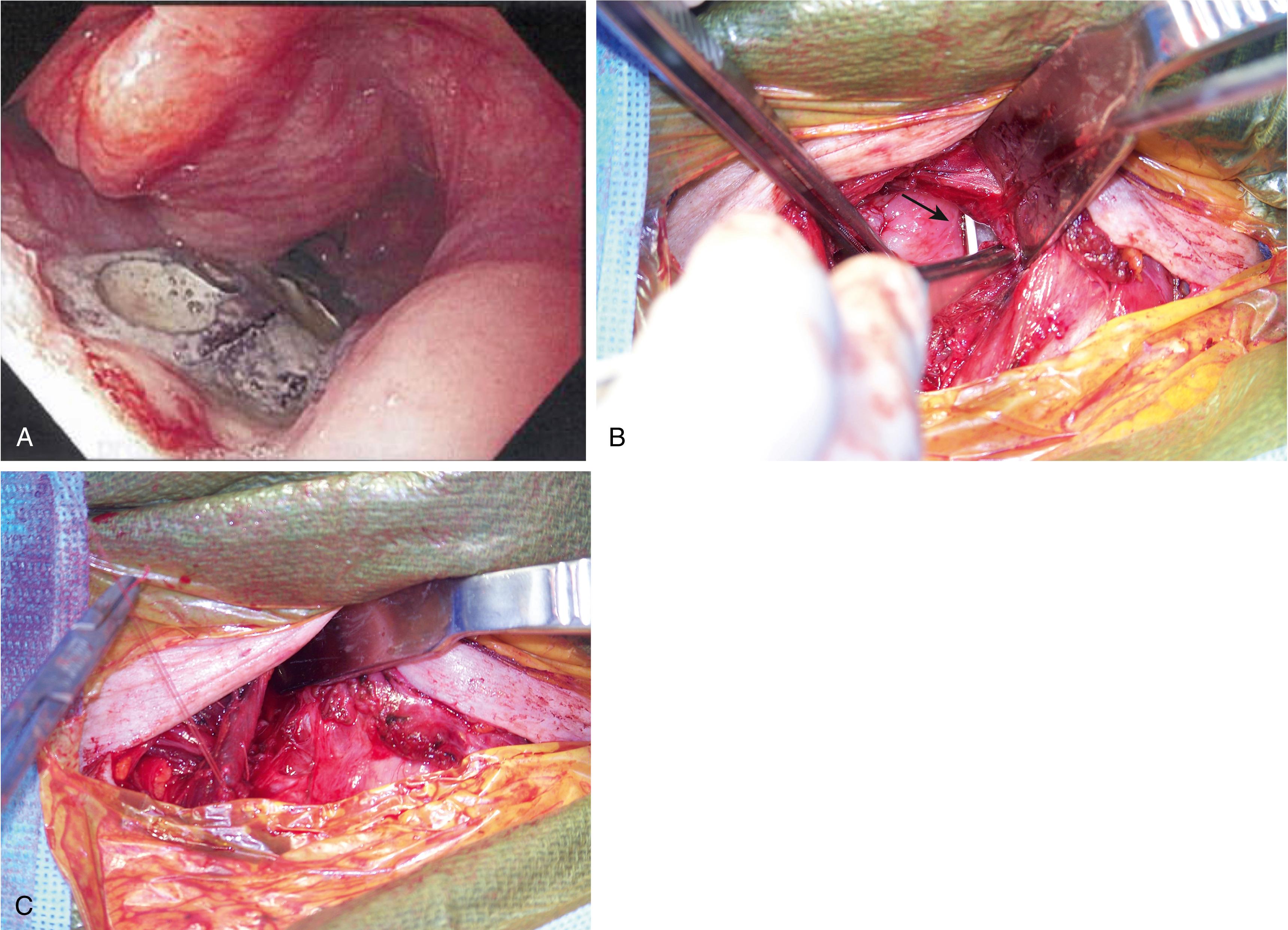
More complicated injuries with longer segments of tissue loss that no longer allow for tensionless reapproximation require longitudinal mobilization of the midesophagus and a reinforced repair backed by a vascularized muscle flap ( Fig. 96.2 ). Extensive injuries that do not lend themselves to repair in this fashion should be diverted proximally and distally to the skin surface and then reconstructed later. Primary reanastomosis may still be achievable after mobilization of the esophagus at the diaphragmatic hiatus to gain additional length. Although lacking in intrinsic coordinated propulsive activity, colonic and jejunal interpositions are yet other reconstruction options.
Delayed perforation may present with similar though less fulminant symptoms or with spinal osteomyelitis. In most cases, the original site of injury will have sealed over, although this should be evaluated with a swallowing study using a water-soluble contrast agent. Subsequent procedures depend on several factors. Any sign of contrast extravasation mandates operative repair; any deep abscess requires drainage. Grossly infected or collapsed bone grafts or vertebrae should be thoroughly debrided and regrafted after a vigorous washout. Long-term (6 weeks), organism-specific intravenous antibiotics should be administered. In less fulminant infections with good anatomic and neurological preservation, a more conservative approach with drainage of superficial pus and administration of systemic antibiotics may be elected initially. Close clinical and radiographic follow-up is extremely important. If the patient is without signs of deep infection, nonoperative management may be a viable option, even in the presence of spine instrumentation. The erythrocyte sedimentation rate and C-reactive protein level are useful laboratory parameters to monitor. Clinical or radiographic progression would then mandate operative management.
Sore throat and hoarseness are common and mostly transient complaints after anterior cervical surgery. Some researchers have sought to relate this phenomenon to increased pressure exerted on the laryngotracheal lumen by the endotracheal tube cuff following insertion of deep retractors. Venting enough air from the cuff to create a small air leak around the endotracheal tube may alleviate at least some of this problem.
Fortunately, serious injury to the trachea is rare. Minor lacerations that are observed intraoperatively are repaired primarily, leaving the patient intubated for 48 to 72 hours to allow the wound to seal. More severe injuries and those that are detected in a delayed fashion because of pneumomediastinum or neck emphysema may be more appropriately managed with primary repair and tracheostomy. Occasionally, the parietal pleura is violated during low anterior or upper thoracic discectomy. This requires no specific treatment as long as the visceral pleura has not been violated to cause a persistent air leak. This possibility can be assessed by flooding the wound with saline and observing for a bubble stream during positive-pressure ventilation. This bubble stream implies an ongoing air leak and indicates tube thoracostomy.
Carotid artery injury is unusual in the midcervical spine if care is taken during placement of toothed retractor blades. At this level, the artery is sufficiently removed from its tether points at the skull base and the aortic arch that the required degree of lateral mobilization is easily achieved. If the carotid sheath is scarred by previous radiation or operation, it should be freed longitudinally until the vessel can be displaced laterally without undue force or distortion.
Direct suture repair of carotid injuries is straightforward in first-time operated-on cases, because good proximal and distal control are readily achieved, and the arterial wall willingly accepts suture. Unfortunately, this complication is most likely to occur in reoperated case and/or wounds with a history of irradiation. Exposure is more difficult, the vessels can be very friable, and repair is challenging.
Vertebral artery injury is an unusual complication for cervical spine surgery, with an overall estimated incidence of 0.14%. The vertebral artery is not routinely encountered in routine anterior cervical approaches. It may be injured by lateral exploration of the neural foramen in pursuit of uncovertebral joint osteophytes. This type of injury is usually minor and is controlled with small amounts of hemostatic packing. Most commonly, the vertebral artery is injured in anterior cervical spine surgery in the V2 segment (extending from the C1‒C6 transverse foramina) by use of the drill off the midline, excessive lateral foraminal decompression/bone disc removal, or pathological softening of the bone of the lateral part of the spinal canal caused by infection or tumor. Additionally, the artery runs between the transverse process of C7 and the longus colli musculature. Thus, extensive lateral dissection at C7 should be avoided. More significant injury to the vertebral artery can result during cervical corpectomy if the decompression is taken too far laterally. These injuries are usually incurred by overly aggressive drilling. They can be avoided if all dissection is performed under magnification and if the drill is not permitted to penetrate the deep bony cortex. The vertebra is “eggshelled out” by the drill, leaving only a thin bony cortex to be avulsed with a fine curet or thin-footed Kerrison rongeur. The ventral aspect of the transverse processes of C3‒C6 is also marked by a small bony tubercle that alerts the operator to the laterality of the exposure. More often, however, the point of injury occurs on the medial side of the artery, where the drill has broken through the vertebral cortex. Preoperative imaging studies should image the vertebral artery when a carpectomy is considered, as a risk factor for vertebral artery injury is an aberrant medial vertebral artery. If this is present, an alternative procedure or additional interventions such as stent placement should be considered.
Vertebral artery injury with posterior cervical surgery has been most commonly associated with C1‒C2 transarticular screw insertion, with a reported incidence of 1.3%. The artery may be injured if the screw trajectory is too low or too lateral. C1 lateral mass and C2 pedicle constructs may reduce the risk of vertebral artery injury. Nevertheless, lateral perforation of the C2 pedicle may result in vertebral artery injury. Also, too far lateral exposure of the posterior or superior ring of C1 may predispose to vertebral artery injury. Subaxial lateral mass screw insertion may result in vertebral artery injury, but such an injury is most unusual.
When a vertebral artery injury occurs intraoperatively, there is usually sudden, nonpulsatile, copious bright red bleeding, although it may appear dark because of injury to the surrounding venous plexus. Injury is dangerous, as hemorrhage may be massive, and cerebral ischemia/embolic phenomena may result.
Strategies to manage a vertebral artery intraoperatively include tamponade, repair, and ligation. Tamponade includes use of hemostatic agents such as Gelfoam and oxidized cellulose (Surgicel). Although some have advocated use of hemostatic matrixes such as Floseal (Baxter Biosciences, Vienna, Austria) in the treatment of vertebral artery injury, there is concern of thromboembolic events should such a matrix be injected intravascularly, , and this is best avoided. Should tamponade fail to control hemorrhage, the surgeon must enlarge the exposure, including deliberate resection of the ventral lip of the transverse process to uncover more of the artery proximally and distally as localized pressure is applied over a cottonoid at the point of hemorrhage. The surgeon must then weigh the options of vertebral ligation versus repair. Most patients, especially younger patients, tolerate unilateral vertebral ligation well. However, a small number of patients will have an isolated vertebral artery terminating in the posterior inferior cerebellar artery or a compromised contralateral vertebral artery. Ligation of a vertebral artery in these circumstances could result in cerebellar or brainstem infarction. Because the status of the vertebral artery anatomy might not be known preoperatively, significant effort should be made to preserve vascular patency whenever possible. In this setting, intraoperative angiography should be considered. Endovascular treatment has become an important treatment modality in the setting of spine surgery–related vertebral artery injury, including placement of covered stents, parent artery occlusions, and coiling in the setting of pseudoaneurysms. , If injury occurs at C1‒C2 during transarticular screw insertion, many surgeons advocate placement of a screw into the drilled hole to reduce bleeding. ,
Postoperative management remains controversial. Some surgeons advocate that the patient be observed and that any postoperative intervention be dictated by the patient’s clinical course. Others recommend that a postoperative angiogram be obtained to rule out significant injury, stenosis, pseudoaneurysm, or arteriovenous (AV) fistula ( Fig. 96.3 ). This may allow for endovascular intervention or vessel sacrifice if need be. Additionally, the postoperative neurological examination should be followed, as anticoagulation and antiplatelet therapy may be needed to prevent vertebrobasilar thromboembolism. Complications of vertebral artery injury include AV fistulae, late-onset hemorrhage, pseudoaneurysm and thrombosis with embolic incidents, cerebral ischemia, stroke, and even death. The vascular complications might occur days to years later. Thus after identifying an injury, serial imaging with magnetic resonance angiography or computed tomography (CT) angiography should be considered to rule out development of a pseudoaneurysm.

Studying preoperative CT and magnetic resonance imaging (MRI) scans and noting the possibility of ectatic, tortuous, or aberrant vasculature can reduce the risk of vertebral artery injury. Additionally, these studies are useful for tumor surgery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here