Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Upper extremity disease and its management are amongst some of the most complex topics in vascular surgery. Unlike lower extremity disease, which is due to atherosclerosis most of the time, upper extremity arterial disease encompasses a wide variety of etiologies. These disease processes ranges from various autoimmune diseases, such as Takayasu and giant cell arteritis, to thoracic outlet disease, embolic disease, hypothenar syndrome, and atherosclerosis. Depending on the cause of upper extremity ischemia, treatment varies from strictly medical management to strictly surgical management, but most often a combination of both is required.
Upper extremity arterial occlusive disease is responsible for less than 5% of all cases of limb ischemia. Even in high-volume centers, arm reconstructions account for only 3% of elective limb revascularizations. Palmar and digital artery occlusive disease is the most common cause of upper extremity arterial occlusive disease, whereas large-vessel disease, including arteries proximal to the wrist, accounts for less than 10%. The majority of arm emboli are cardiac in origin (75%). The most common site for emboli is the brachial artery (60%), followed by the axillary artery (26%). In situ thrombosis accounts for only 5% of episodes of arm ischemia. This chapter deals with revascularization for both acute and chronic ischemia involving the intrinsic arteries of the upper extremities, including the axillary, brachial, radial, ulnar, and palmar arteries. Raynaud syndrome (see Ch. 142 , Raynaud Phenomenon), thoracic outlet obstruction (see Ch. 125 , Thoracic Outlet Syndrome: Arterial), occlusive disease of the great vessels (see Ch. 101 , Brachiocephalic Artery Disease: Surgical Treatment), Takayasu arteritis (see Ch. 140 , Takayasu Arteritis), and giant cell arteritis (see Ch. 138 , Vasculitis and Other Arteriopathies) are described elsewhere.
Between 9% and 30% of patients seen by vascular surgeons with upper extremity arterial occlusive disease are managed conservatively because of significant comorbid conditions or minimal symptomatology. Conservative therapy classically includes anticoagulation for acute or subacute ischemia. Adjunct therapies like calcium channel blockers, topical nitrates, and phosphodiesterase inhibitors have also been used with variable success. Smoking cessation, optimizing cardiac output, avoiding vasopressors, avoidance of caffeine and cold, and warming the upper extremity are also useful to obtain the best possible outcome.
Acute ischemia, typically embolic in nature, is best managed with operative embolectomy; however, postoperative mortality rates are as high as 12%, related to comorbid conditions. After successful brachial embolectomy, 95% of patients will remain free of symptoms. Patients managed conservatively are underreported in the literature. In the few reported series, assessment of symptoms and disability is inconsistent. However, in a series of 95 patients described by Baird and Lajos in 1964 with arm ischemia managed without surgery, 32% were left with permanent disability in the arm. In 1977, Savelyev and coauthors reported that 75% of patients managed conservatively had a poor functional outcome. In 1985, Galbraith and associates confirmed that 50% of their conservatively managed patients had persistent exercise-induced forearm pain (a claudication equivalent). Therefore, although conservative management is appropriate for some patients with acute ischemia, for those with a reasonable life expectancy, all efforts should be made to restore blood flow.
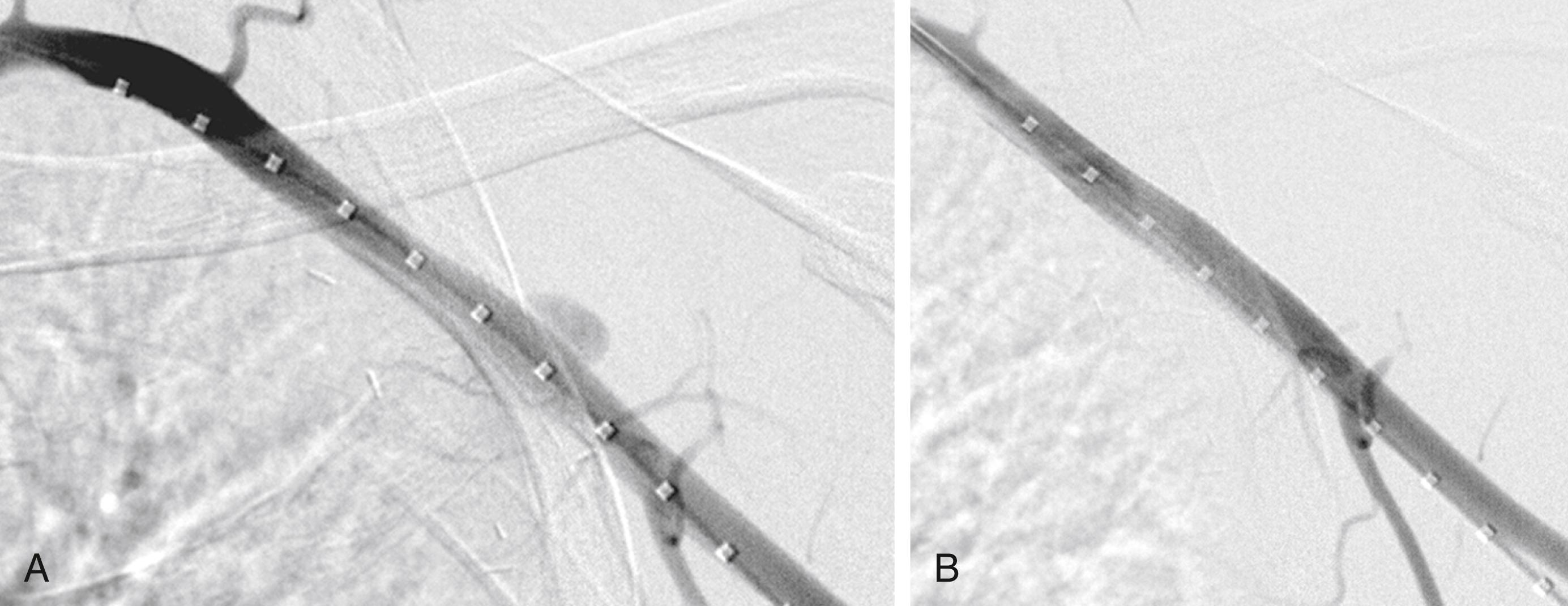
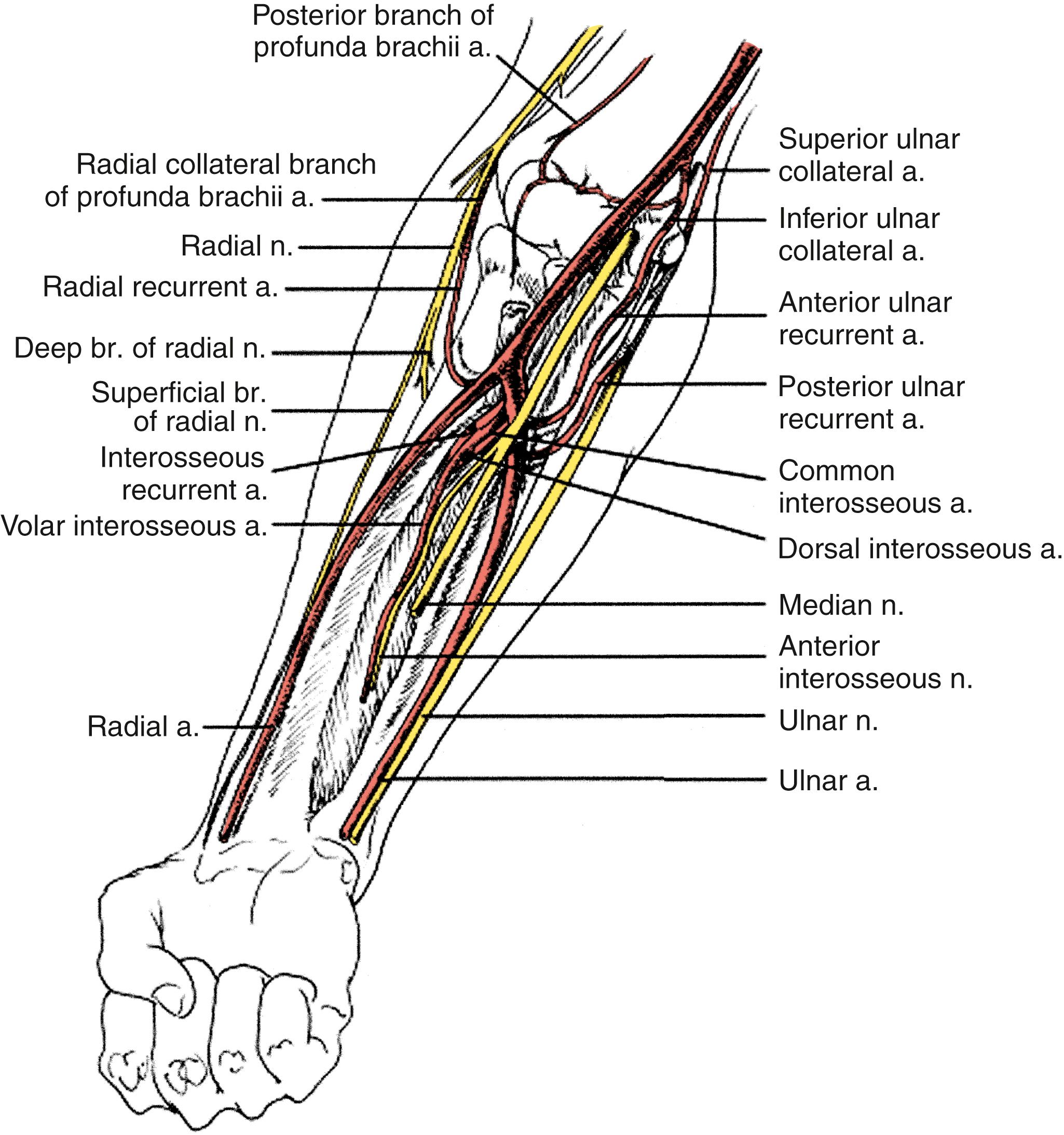
Endovascular therapies for the treatment of arterial occlusive disease have been increasingly performed during the last decade with advancement in catheter, balloon, and stent technology. The majority of lower extremity revascularizations in contemporary vascular surgery practices are now performed percutaneously. However, the upper extremity has not experienced the same paradigm shift, possibly due to the relative infrequency of interventions or the underlying causes of the arterial disease, as well as the simplicity of the open surgical procedures. A recent Japanese multicenter study reviewed 553 patients undergoing primary endovascular therapy with angioplasty and/or stenting for subclavian artery occlusive disease, with a primary patency of 90% at 1 year and 81% at 5 years, although it is unclear what aspect of the subclavian artery was involved. Most institutional reviews that describe treatment of occlusions in the axillary, brachial, radial, and ulnar arteries still involve surgical bypass or embolectomy. , There are scattered reports of emergency placement of covered stents in the axillary artery in trauma patients. An example of such therapy is illustrated in Figure 121.1 . There are also reports of small series of patients treated by axillary artery angioplasty for radiation-induced occlusion, by brachial artery atherectomy, and by radial artery stenting for digital gangrene, but their numbers are low and follow-up is minimal. Therefore, dissection and exposure of the arterial anatomy for revascularization will be described at the most common levels of intervention ( Fig. 121.2 ).
See Chapter 59 (Upper Extremity Vascular Exposure).
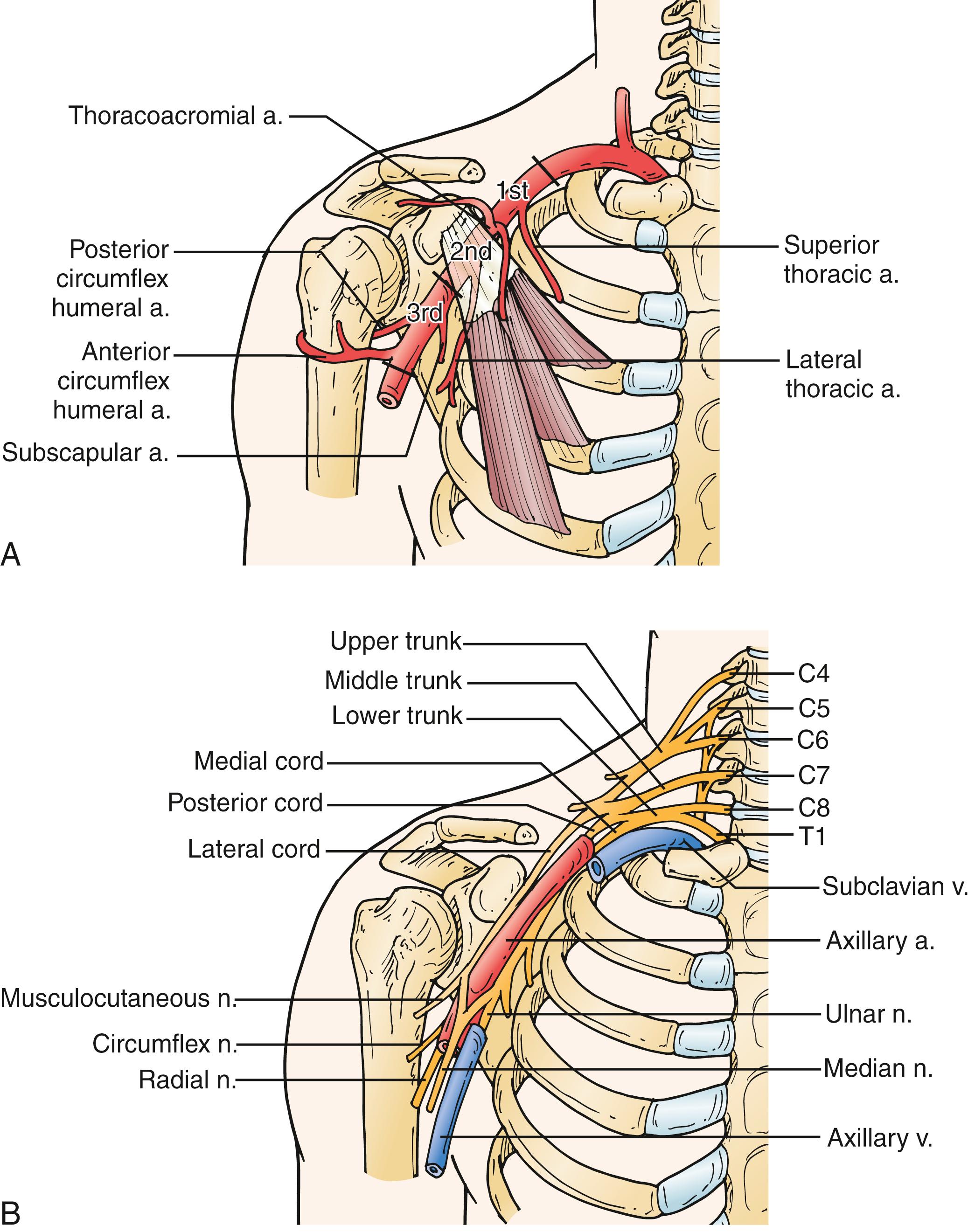
The patient is positioned supine and the arm is usually placed at the patient’s side if an infraclavicular incision is being made. This allows the surgeon to have better access to the operative field without hindrance. However, if the distal target is in the arm, circumferential prepping and draping may be needed. The axillary artery is exposed with a transverse incision 2 cm below the middle third of the clavicle ( Fig. 121.3 ). The underlying pectoralis major muscle is divided, when possible, in the decussation between the sternal and clavicular portions. Division of the pectoralis major exposes the clavipectoral fascia, which is divided. The axillary artery is located cephalad to the vein. It is dissected carefully to avoid injury to the surrounding cords of the brachial plexus. The second portion of the axillary artery can be exposed by dividing the pectoralis minor muscle. If needed, the distal third of the axillary artery may also be exposed. An oblique incision is made along the lateral margin of the pectoralis major muscle with the arm abducted 90 degrees relative to the thorax. Once the subcutaneous tissue is divided, the axillary sheath is located near the posterior and inferior border of the coracobrachialis. Careful dissection avoids injury to the medial and lateral cords of the brachial plexus medially and the median and ulnar nerves laterally.
The mid or distal brachial artery is exposed through a medial incision over the bicipital groove, allowing access to the proximal or middle third of the brachial artery. The basilic vein and cutaneous branches of the median nerve are located within the subcutaneous tissue and should be avoided during dissection. Traction or transection of the median antebrachial cutaneous nerve may lead to hyperesthesia or anesthesia along the medial dorsal surface of the forearm and can be quite debilitating to the patient. The brachial sheath is then incised longitudinally. The median nerve is the most superficial structure encountered. The nerve is gently mobilized and retracted to allow access to the brachial artery. Crossing vein branches should be divided to minimize the risk of injury to the posteriorly located ulnar nerve.
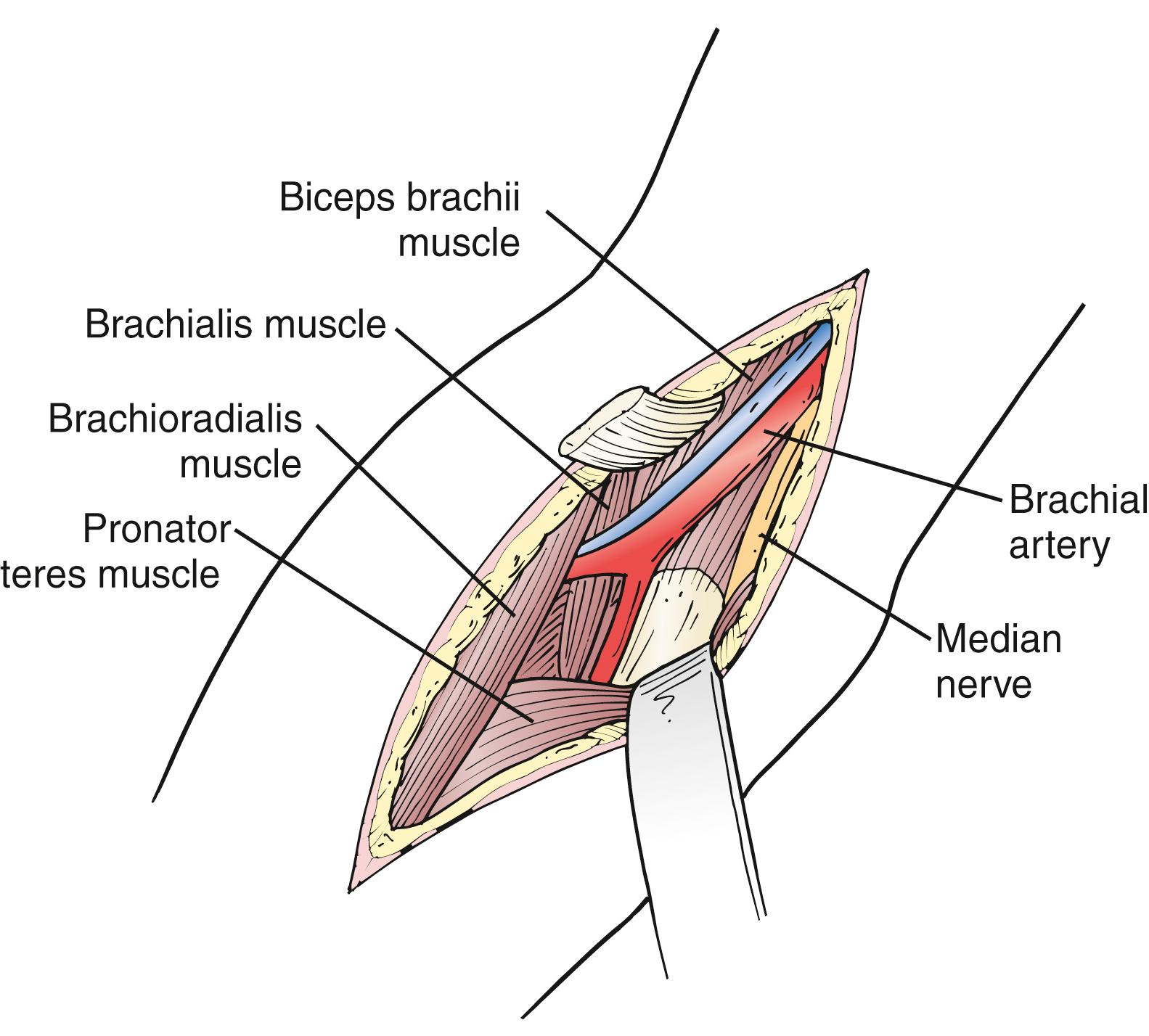
The distal third of the brachial artery and its bifurcation, in contrast, are exposed in the antecubital fossa ( Fig. 121.4 ). A lazy S-shaped incision is recommended to expose the origins of the ulnar and radial arteries and to decrease the risk of contracture over the antecubital fossa. For the distal most brachial artery, a vertical incision can be used beginning just below the fossa. The skin and subcutaneous tissues are divided. Care is taken to preserve the superficial veins, especially the median antecubital vein, because it may be required for autogenous patch angioplasty closure. The bicipital fascia is incised and the brachial artery is seen coursing between the biceps tendon laterally and the median nerve medially. Dissection is continued distally until the ulnar and radial arteries are encountered. The radial artery is really a continuation of the brachial artery. The ulnar artery, on the other hand, comes off the brachial artery medially and, within 2 to 3 cm, dives beneath the pronator and epitrochlear muscles.
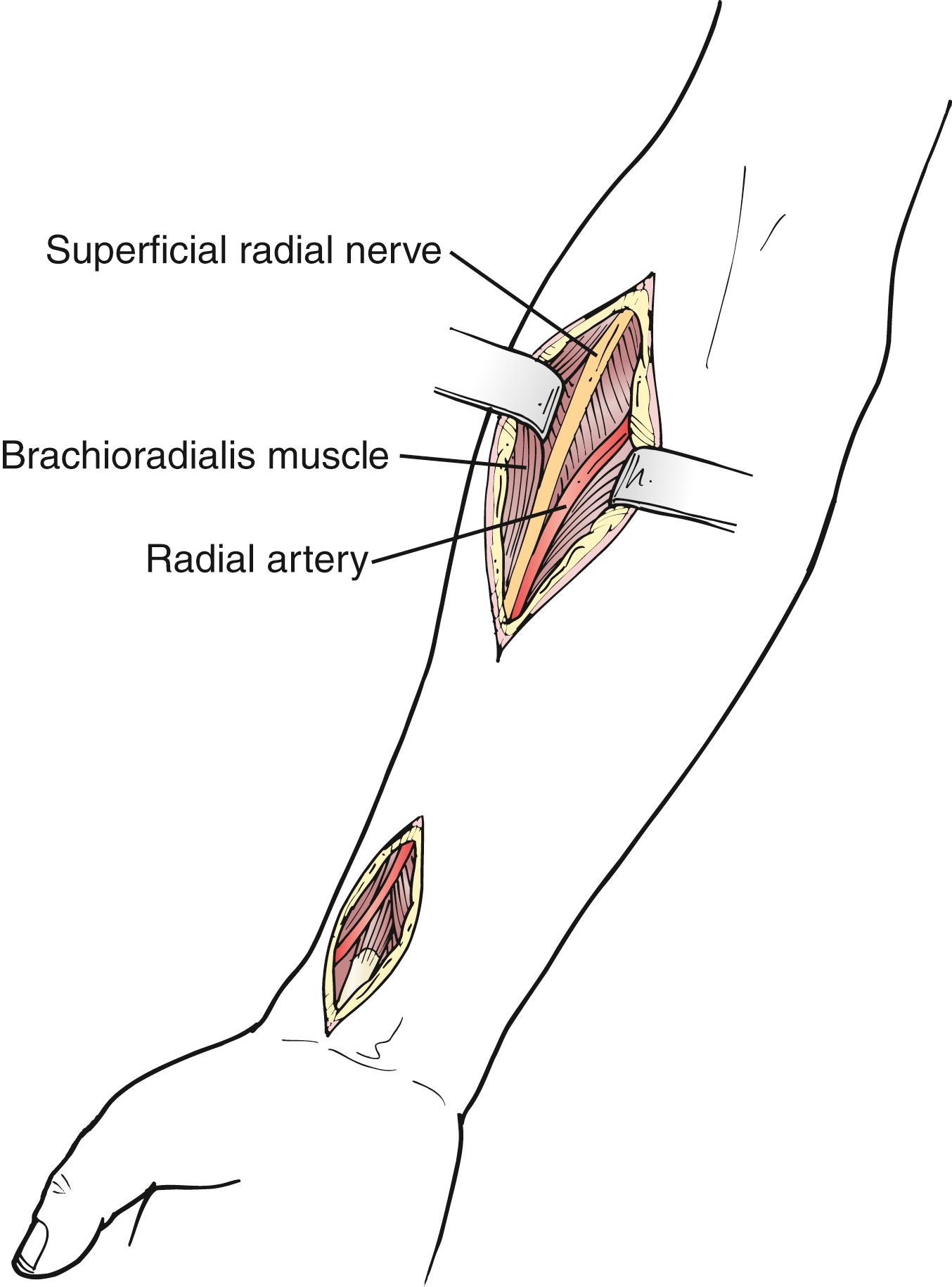
The course of the radial artery in the forearm follows an oblique line from the brachial artery pulse medial to the biceps tendon to the styloid process of the radius. In the midforearm, the radial artery is medial to the brachioradialis and lateral to the flexor carpi radialis. A lateral longitudinal incision is made. The muscles are separated to reveal the radial artery as needed ( Fig. 121.5 ). At the wrist the radial artery is exposed by a longitudinal incision between the tendons of the flexor carpi radialis and the brachioradialis muscles. This is the traditional site of the radial artery pulse in normal subjects. The artery is superficial and exposure is relatively straightforward. The superficial branch of the radial nerve is often located near the lateral aspect of the artery. Injury can result in troublesome paresthesias along the lateral aspect of the thumb.
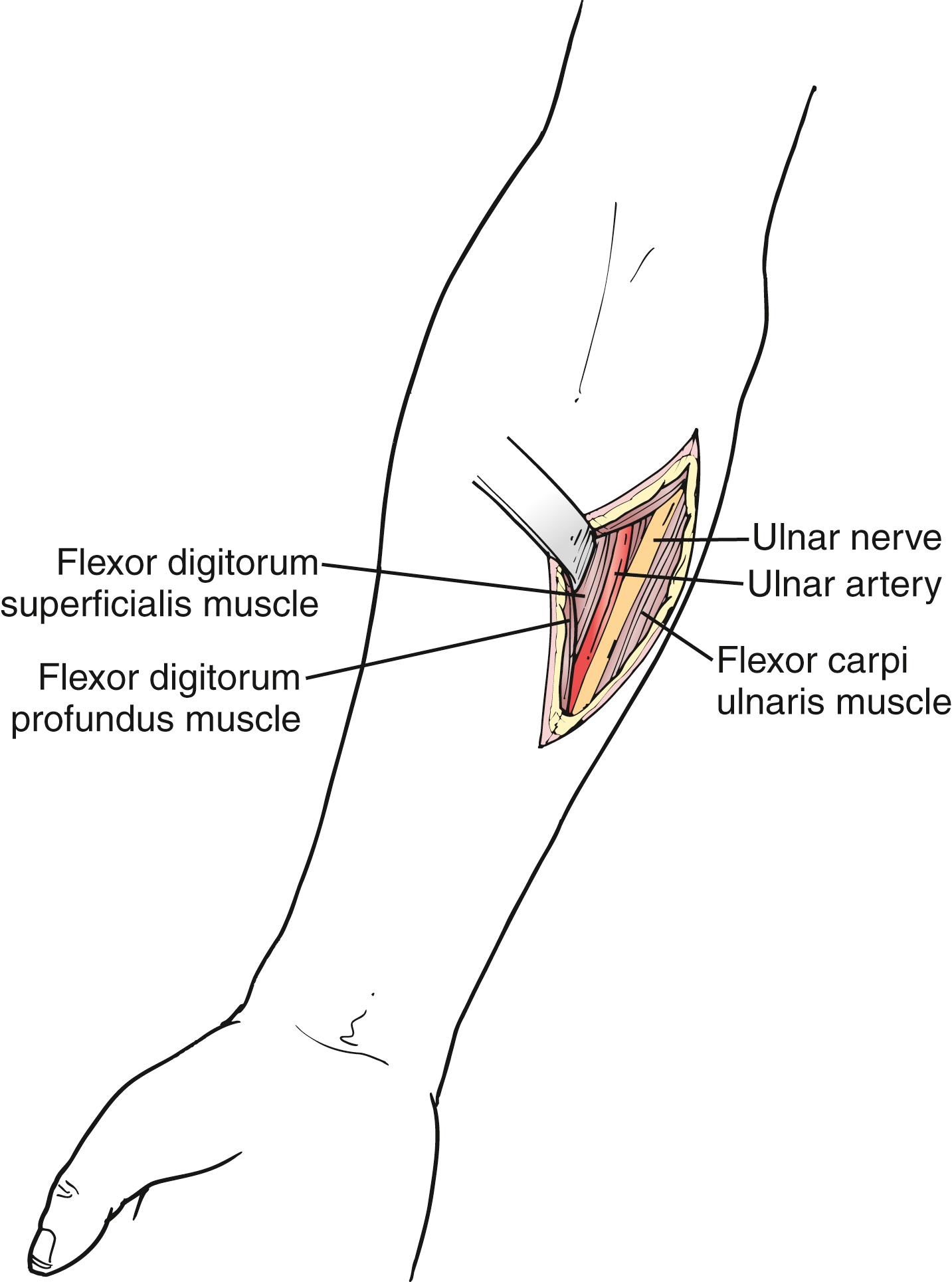
The ulnar artery extends from the medial epicondyle of the humerus to the pisiform bone. In the midforearm, the ulnar artery lies beneath the deep fascia between the bellies of the flexor digitorum laterally and the flexor carpi ulnaris medially ( Fig. 121.6 ). The ulnar nerve joins the artery on its lateral aspect for its distal two-thirds. It may be injured if not carefully identified and preserved. At the wrist, the ulnar artery is lateral to the flexor carpi ulnaris (it is the most medial tendon palpable at the wrist). For exposure, this tendon is identified and a vertical skin incision is made lateral to it. The ulnar artery is relatively deeper than the radial artery at the wrist but just as easily exposed. The palmar cutaneous branches of the ulnar nerve are superficial to the artery here and should be preserved.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here