Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Metaphyseal fit and ingrowth can provide both rotational and axial stability without distal diaphyseal support.
Bone remodeling after insertion of metaphyseal engaging short stems shows endosteal condensation and cortical hypertrophy in the proximal metaphyseal region of the femur.
Functional Harris Hip Scores and Western Ontario and McMaster Universities Osteoarthritis Index pain scores are equivalent in patients with metaphyseal engaging short stems and uncemented stems of conventional length.
The surgical technique for accurately, reproducibly inserting metaphyseal short stems is virtually identical to the technique for inserting cementless stems of conventional length.
Total hip arthroplasty (THA) is a highly successful, safe, and cost-effective intervention for the treatment of moderate and severe degenerative arthritis. Porous coated, uncemented femoral stems were introduced for use in THA in the early 1980s. Noncemented stems achieve their fixation by either porous diaphyseal fixation or porous metaphyseal fixation; nonporous diaphyseal contact produce dependable long-term fixation and pain-free function in patients of all ages and bone quality, and in patients with a wide range of clinical function. Uncemented, porous femoral implants are now routinely used in virtually all patients undergoing primary THA. Despite the documented success of these implants, current uncemented stems are being used in patients whose size, age, level of physical activity, and bone quality present particular challenges for uncemented fixation technologies. These challenges include (1) the need for very long term fixation, (2) the preservation of proximal femoral bone stock, (3) the potential need for effective, safe, bone-preserving femoral component revision, (4) the desire to reproduce a wide range of proximal femoral extraarticular anatomic variations with the provision of multiple offset options, (6) the elimination of thigh pain in extremely active patients of all ages and bone quality, and (7) the ability to insert implants safely, securely, and reproducibly with specific surgical approaches, for example, the direct anterior, which are currently being evaluated and promoted. The success that has been achieved with uncemented femoral stems of a wide range of designs is now encouraging investigators to consider uncemented femoral implant concepts that address these challenges without compromising the high level of success obtainable with current uncemented femoral components.
In particular, there is an interest in short uncemented stem designs that rely on femoral metaphyseal fixation for their stability. The purpose of this chapter is to review the principles underlying these types of femoral components, describe the various design characteristics of these stems, and summarize the clinical results with these stems.
Metaphyseal fit and ingrowth can provide both rotational and axial stability without distal diaphyseal support.
Bone remodeling after insertion of metaphyseal engaging short stems shows endosteal condensation and cortical hypertrophy in the proximal metaphyseal region of the femur.
Patient-reported outcome measurement scores are equivalent in patients with metaphyseal engaging short stems and uncemented stems of conventional length.
The surgical techniques for accurately and reproducibly inserting metaphyseal short stems are virtually identical to the techniques for inserting cementless stems of conventional length.
To understand the design rationale that is currently being applied to short, metaphyseal engaging femoral stems, it is important to consider the function of each portion of a femoral implant. The section of the femoral component that engages the diaphysis contributes to the initial stability of the device. This portion of the component may be cylindrical or tapered ( Fig. 69.1A–C and Video 69.1 ). Tapered stems may be two-dimensional (a coronal taper and a nontapered rectangular lateral border) or three-dimensional (tapered in both the coronal and sagittal planes). The diaphyseal engaging stem may be made of cobalt-chrome alloy or titanium alloy. It may be fully coated with a three-dimensional porous surface, a thin layer of hydroxyapatite, a grit-blasted finish of varying degrees of roughness, or a combination of some or all of these surfaces. The diaphyseal portion of the stem may also be polished. The femoral stem may have flutes and/or slots to resist rotation and decrease stiffness. The intended function of the diaphyseal portion of a femoral stem is reflected in its shape, metallurgy, and surface treatment.
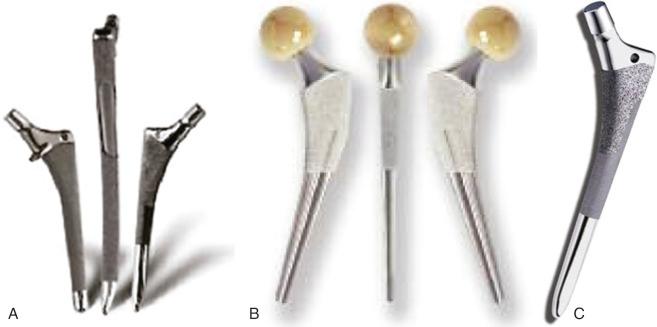
Metaphyseal engaging tapered short femoral stems.
Cylindrical, cobalt-chromium, extensively porous coated stems (e.g., the Anatomic Medullary Locking [AML]) of conventional length are designed to provide rigid initial and long-term fixation in the diaphysis. Initial axial fixation is achieved by tightly engaging a significant segment of the endosteal diaphyseal cortex. Although this engagement with the diaphysis may provide initial rotational stability, the porous coating also provides some resistance to rotational stresses. Long-term fixation is achieved by bone ingrowth into the porous coating. The long-term clinical and radiographic results of cylindrical, extensively coated stems have been well-documented. The long-term stability of stems of this design in patients of all ages and bone quality is excellent. The consistent concerns associated with these stems have been stress shielding and thigh pain a
a References .
( Fig. 69.2 ). Cylindrical stems without porous coating may be made of either cobalt-chromium or titanium alloys. The surfaces may be grit-blasted to varying degrees or polished. Cylindrical stems with a titanium alloy core and flexible polymer coating are also available. These stems are designed to provide a degree of initial axial and rotational fixation by coming in contact with the diaphysis, but to avoid the stress shielding and thigh pain that might be associated with large, long, stiff metal cylindrical stems.

Cylindrical femoral components of conventional length without diaphyseal porous coating rely on metaphyseal bone contact to enhance their initial axial and, especially, rotational stability. Moreover, these stems seek long-term fixation through bone ingrowth or ongrowth in the metaphysis. These stems achieve metaphyseal stability by attempting to optimize resistance to rotation with rectangular shapes, lateral antirotation ridges, or wedge shapes. Some implants with uncoated cylindrical stems seek to achieve rotational stability and optimized proximal bone restoration by maximizing the fit and fill of the metaphysis (e.g., the PCA implant). All current metaphyseal engaging implants with nonporous coated diaphyseal stems of conventional length seek to increase rotational stability and positive bone remodeling with metaphyseal circumferential porous coatings or ongrowth surfaces. There are a number of reports with more than 10 years of follow-up that indicate that femoral components with cylindrical stems of conventional length without ingrowth or ongrowth coating are associated with durable fixation and very satisfactory and reliable clinical results. a
a References .
The goals of stems of this design are to decrease the incidence of thigh pain and stress shielding associated with extensively porous coated, cylindrical stems while retaining, through osseointegration in the metaphysis, durable fixation. In general, stems of this design seem to be associated with a lower incidence of thigh pain and less proximal stress shielding than extensively coated, cobalt-chromium, cylindrical stems. b
b References .
Tapered uncemented femoral components of conventional length seek to achieve fixation in two stages. Initial rigid fixation is achieved by three-point self-locking fixation ( Fig. 69.3 ). When the tapered stem is securely inserted into the cylindrical femur, hoop stresses are generated. When stress relaxation of the femur has occurred, equilibrium is set up between the bone and stem and the axially loaded tapered component will not advance. In principal, this mechanism of initial axial fixation works best in proximal femoral morphologies with tapered medullary shapes. Therefore, stems of this design are best applied to Dorr type A (champagne fluted) and type B (funnel shaped) and less well-suited to type C (cylindrical shape) femurs. The proximal component taper seeks to maximize implant-bone contact with the intramedullary proximal femoral shaft taper and provide a gradual loading profile to the proximal femur.

The establishment of initial rotational stability of tapered stems of conventional length is critical for achieving initial rigid fixation. Some tapered stem designs (e.g., the Zweymüller and Cementless Locking Stem) are rectangular. Some (e.g., Taperloc) have antirotation lateral ridges. Other stems (e.g., the Syngery stem) have wedge-shaped proximal geometries. Still others (e.g., the ABG stem) have anatomically shaped metaphyseal designs that seek to achieve rotational stability by maximizing fit and fill in the proximal femur ( Fig. 69.4 ).

The second stage of fixation sought by tapered stems occurs in the metaphysis and depends on the presence of a circumferential ingrowth or ongrowth surface. It is believed that the more extensive the area of contact between implant and metaphyseal bone, the more secure will be the secondary fixation and the more positive will be the proximal bone restoration and remodeling. The goals of tapered stems of conventional length are to achieve rigid, durable fixation; eliminate thigh pain; and minimize stress shielding. A substantial number of studies have established the clinical and radiographic reliability and durability of tapered stems of many designs. a
a References .
In general, the use of femoral components of conventional length with tapered diaphyseal stems is associated with less thigh pain than implants with cylindrical stems. b
b References .
In summary, the diaphyseal portion of femoral stems, both cylindrical and tapered, are designed to provide the primary axial stability to the component and varying degrees of rotational stability. This portion of the implants is particularly critical for the achievement of rigid initial fixation. The metaphyseal portion of femoral implants provides initial rotational stability. The provision of this stability may be particularly important in stems of tapered designs or polished cylindrical designs in which localized bone contact and the absence of porous coating reduces the resistance to rotation provided by the diaphyseal portion of these implants.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here