Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
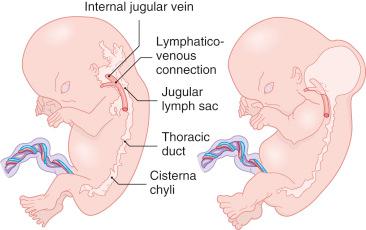
The lymphatics are an extensive unidirectional system of blunt-ending vessels that regulate normal tissue pressure by retrieving excess fluid from the interstitium, transporting it to regional lymph nodes, and returning it to the venous system by way of the thoracic duct. The lymphatic system makes its appearance during the sixth week of human embryonic development as an outgrowth from the venous system. On a molecular level, lymphangiogenesis is heralded by the polarized expression of the homeobox transcription factor PROX1 in a subpopulation of endothelial cells located within the cardinal vein. This event is accompanied by a budding of the endothelium from primitive veins and by the induction of lymphatic- specific genes, LYVE1 and VEGFR3 ( FLT4 ). Expression of PROX1 appears to be a master event in lymphangiogenesis, because in its absence there is agenesis of the entire lymphatic system. VEGFR3 in turn is largely responsible for the migration and formation of primary lymphatic sacs, which through budding growth give rise to the lymphatic vasculature. When lymphatic sacs are formed, the lymphatic and blood vasculature develop independently and only remain connected at certain specific points to allow return of the lymph fluid. The molecular events underlying late lymphangiogenesis are less well understood. One gene, FOXC2 , which is mutated in inherited lymphedema, appears highly associated with the morphogenesis of lymphatic valves, and deficiencies in angiopoietin 2 are associated with defects in both patterning and function of the lymphatic system.
Small lymphatics closely resemble capillaries but can be distinguished ultrastructurally and immunohistochemically. Unlike the vascular endothelial cell, the lymphatic endothelial cell is invested by neither a basement membrane nor pericytes, with the exception of large collecting lymphatic channels. These observations are borne out by immunohistochemistry (IHC). Whereas antibodies to type IV collagen and laminin demonstrate a linear pattern of immunoreactivity around vascular capillary endothelium, this pattern is lacking around lymphatic capillary endothelium. Although lymphatic endothelial cells occasionally manifest tight junctions (zonula adherens) and macula adherens, and desmosomes are present, there are many areas of simple overlapping of cells with no junctions. This arrangement creates a swinging-door effect so that fluid can passively enter the lymphatic space during periods of increased interstitial pressure. Pinocytotic vesicles, thin cytofilaments, modest numbers of mitochondria, and endoplasmic reticulum, similar to those in capillaries, are also present in lymphatic cells.
Further differences between vascular and lymphatic capillary endothelium can be demonstrated by IHC using antibodies targeted against lineage-specific proteins, basal lamina, and pericytes. Lymphatic endothelium typically expresses PROX1, LYVE1, and VEGFR3, but usually lacks CD34 and does not possess an investiture of actin-positive pericytes. The reverse phenotype is observed in blood vascular endothelium. Additionally, CD31 expression in vascular capillary endothelial cells is found only on the luminal surface, whereas lymphatic capillary endothelial cells show luminal and abluminal CD31 expression.
Lymphatic anomalies result from defects in development and maturation of function of the lymphatic system and can be broadly grouped as (1) lymphatic malformations, (2) lymphedema, chylothorax, and chylous ascites, and (3) overgrowth syndromes with a lymphatic component. The genetic events underlying many of these lymphatic anomalies have been identified ( Table 23.1 ). With the exception of localized massive lymphedema , a lesion secondary to morbid obesity and often confused with a soft tissue sarcoma, discussion of lymphedema, syndromic lymphedema, and syndromic chylothorax/chylous ascites is beyond the scope of this chapter, and the reader is referred to authoritative reviews on these subjects.
| Anomaly | Gene | Mutation Type | Inheritance |
|---|---|---|---|
| Isolated Lymphedema | |||
| Primary congenital lymphedema | FLT4 | Inactivating | AD, AR, de novo |
| Milroy-like disease | VEGFC | LOF | AD |
| Syndromic Lymphedema | |||
| Hennekam lymphangiectasia-lymphedema | CCBE1 | LOF | AR |
| Lymphedema-distichiasis and yellow nail syndrome | FOXC2 | LOF | AD |
| Hereditary lymphedema II | GJC2 | Missense | AD |
| Oculodentodigital dysplasia/lymphedema | GJA1 | Missense | AD |
| Choanal atresia/lymphedema | PTPN14 | LOF | AR |
| Hypotrichosis-lymphedema-telangiectasia syndrome | SOX18 | LOF? | AR, AD, de novo |
| Lymphedema-lymphangiectasia | HGF | LOF? | AD? |
| Microcephaly with or without chorioretinopathy, lymphedema, or mental retardation | KIF11 | LOF | AD, de novo |
| Noonan syndrome 1 | PTPN11 or SOS1 | GOF | AD |
| Emberger syndrome | GATA2 | LOF | AD |
| Osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia, and immunodeficiency syndrome | IKBKG | Hypomorphic | X-linked |
| Capillary malformation–arteriovenous malformation with lymphedema | RASA1 | LOF | AD |
| Aagenaes syndrome | Locus in 15q | Unknown | AR |
| Syndromic Chylothorax/Chylous Ascites | |||
| Fetal chylothorax | ITGA9 | Missense | AR, de novo |
| Noonan syndrome, cardiofaciocutaneous syndrome | KRAS | GOF | AD |
| Noonan syndrome 1 | RAF1 | GOF | AD |
| Costello syndrome | HRAS | GOF | AD |
| Syndromes with Lymphatic Malformations | |||
| Turner syndrome | Monosomy X | Sex-linked | |
| Proteus syndrome/PTEN hamartoma syndrome | PTEN | LOF | AD, de novo |
| CLOVES syndrome, Klippel-Trénaunay-Weber syndrome | PIKC3A | GOF | Somatic |
| Proteus syndrome | AKT1 | GOF | Somatic |
Regarded as an abnormality of morphogenesis rather than as a neoplasm, lymphangiomas are now referred to as lymphatic malformations ( Fig. 23.1 ). They are subclassified as microcystic , macrocystic (cysts >0.5 cm), or combined . Diffuse lymphatic malformations involving multiple organs are still often referred to as lymphangiomatosis .
The pathogenetic mechanisms underlying lymphatic malformations are poorly understood but likely vary depending on the type of malformation. Type I hereditary lymphedema , a malformation of small lymphatic vessels that presents shortly after birth, is the result of a germline mutation of VEGFR3 . Type II hereditary lymphedema , a malformation presenting later in life and associated with distichiasis (double eyelashes), is caused by mutations in the FOXC2 transcription factor gene. Lymphatic abnormalities also occur in association with mutations in the SOX18 transcription factor gene and the NEMO ( IKBKG ) gene. But the vast majority of lymphatic malformations are sporadic. Given an understanding of the molecular basis of normal lymphangiogenesis, it is not unreasonable to assume that, in the future, many will be traced to somatic mutations in genes controlling normal lymphangiogenesis.
Relative to vascular malformations, lymphatic ones are rare; Bill and Sumner estimated that they accounted for 5 of 3000 admissions at Children’s Orthopedic Hospital. The gender incidence is approximately equal. Half of all lymphatic malformations are present at birth, and as many as 90% are evident by the end of the second year of life. Those that present during adult life are superficial cutaneous malformations ( lymphangioma circumscriptum ).
Lymphatic malformations affect almost any part of the body served by the lymphatic system but show a predilection for the head, neck, and axilla ( Figs. 23.2 and 23.3 ), sites that account for one-half to three-fourths of all lymphatic malformations ( Table 23.2 ). They also occur sporadically in various organs, including lung, gastrointestinal tract, spleen, liver, and bone. In the last three locations, they occasionally signify the presence of diffuse or multifocal disease (see section on lymphangiomatosis). Lymphatic malformations also occur in association with hemangiomas in Maffucci syndrome.


| Anatomic Location | No. |
|---|---|
| Head | 35 |
| Tongue | 8 |
| Cheek | 7 |
| Floor of the mouth | 7 |
| Parotid | 5 |
| Other | 8 |
| Neck | 25 |
| Trunk and extremities | 43 |
| Axilla | 15 |
| Pectoral | 10 |
| Arm | 6 |
| Scapula | 5 |
| Other | 7 |
| Internal | 6 |
| Mediastinum | 5 |
| Abdomen | 1 |
∗ There are more than 61 tumors because large tumors were tabulated under several locations.
The most common presentation of a lymphatic malformation is that of a soft fluctuant mass that enlarges, remains static, or waxes and wanes during the period of clinical observation. The overlying skin may appear normal or slightly blue. In some cases, rapid enlargement is the result of an upper respiratory tract infection, which causes obstruction in the lymphatics draining the lesion.
Lymphatic malformations also produce site-specific signs and symptoms. For example, malformations of the major lymphatic ducts produce chylous pleural or pericardial effusions; those in the soft tissues of the extremities produce overgrowth and gigantism, whereas those in the bone produce osteolysis, termed disappearing bone disease (Gorham disease).
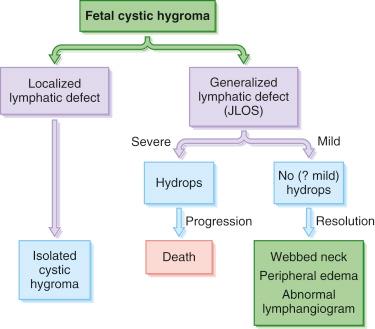
Lymphatic malformations can be effectively imaged by magnetic resonance imaging (MRI) or, in the case of macrocystic lymphatic malformations, by ultrasonography. MR lymphangiography may be very useful for the classification of these anomalies. In utero imaging of lymphatic malformations is especially important because they are associated with hydrops fetalis and Turner syndrome and high mortality ( Figs. 23.4 and 23.5 ). Chervenak et al. found that 11 of 15 intrauterine macrocystic lymphatic malformations (cystic hygromas) were associated with the cytogenetic abnormalities of Turner syndrome (45,X/O or 46,XO/46,XX). Of the 15 fetuses, 13 had severe hydrops, and none of the 15 ultimately survived. The authors suggested that severe aberrations of the lymphatic system in this condition are incompatible with life; milder forms are compatible with survival but give rise to webbing of the neck and edema of the hands and feet, which characterize the Turner syndrome infantile phenotype ( Fig. 23.6 ). Other syndromes may also be associated with fetal macrocystic lymphatic malformations, including Noonan syndrome, familial pterygium colli, fetal alcohol syndrome, and several chromosomal aneuploidies. Because aneuploidic conditions may recur during subsequent pregnancies, cytogenetic analysis of fetuses born with a macrocystic lymphatic malformation is indicated.

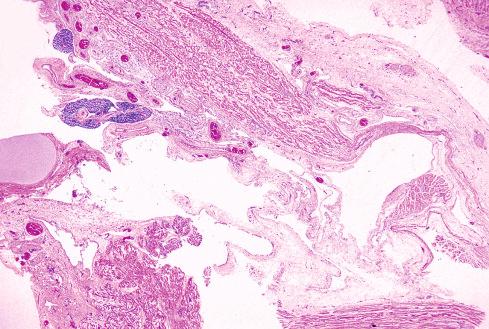
Lymphatic malformations are most common in the neck, where they typically lie in the supraclavicular fossa of the posterior cervical triangle or extend toward the crest of the shoulder. Less frequently, they are located in the anterior cervical triangle just below the angle of the jaw. Tumors in this location may present with airway or feeding problems. Lymphatic malformations are the most common cause of enlargement of the tongue. About 10% of lymphatic malformations of the neck extend into the mediastinum and require careful imaging to define the surgical approach. Grossly, the lesions are unicystic or multicystic masses that involve the superficial soft tissue and tend to bulge outward rather than extend inward (see Fig. 23.3 ). Consequently, they usually do not compromise vital structures, such as the trachea and esophagus, unless they are large. In contrast, malformations involving the soft tissues of the lips, cheek, tongue, and mouth frequently involve deep soft tissue structures and cause functional impairment, depending on their size.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here