Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The surface anatomy of the trunk is of vital importance for operative planning. In the anterior thorax, the sternocleidomastoid (SCM) is the most superior of the critical landmarks. The SCM is the largest of the cervical muscles, traveling obliquely across the neck. It originates on both the manubrium and the clavicle and inserts on the mastoid process of temporal bone. The clavicle is a bone that runs between the sternoclavicular joint and the acromioclavicular joint. It lies directly above the first rib and can be palpated throughout its course in the thorax. The jugular notch, also known as the suprasternal notch, is a recess located between the clavicles medially and just superior to the sternum. The nipple–areolar complex (NAC) is located bilaterally on the breast, roughly at the level of the fourth rib, and consists of an areola with a centralized nipple. Aesthetically, the breast footprint is the effective outline of the breast against the chest wall. The four borders of the breast are the clavicle superiorly, the inframammary fold inferiorly, the sternum medially, and the anterior border of the latissimus muscle laterally. The inframammary fold is the point at which the breast meets the chest wall. These landmarks, as well as Blondeel’s concepts of footprint, conus, and skin envelope, are important in breast surgery. Deep to the breast lies the pectoralis major muscle, which originates at the clavicle and sternum and inserts on the bicipital groove of the humerus. The sternum is a bone located at the center of the thorax and is separated into three parts: manubrium, body, and xiphoid process (superior to inferior). The body of the sternum articulates the manubrium superiorly, the xiphoid process inferiorly, and the costal cartilage of ribs two through six bilaterally. The xiphoid process, the inferior-most aspect of the sternum, is a cartilaginous structure located at the level of T10 which ossifies throughout adult life. The axilla is a critical anatomic region which contains key arteries, veins, nerves, and lymph nodes, found laterally in the thorax. The borders of the axilla are the humerus laterally, the serratus anterior and thoracic cage medially, pectoralis major anteriorly, and the latissimus dorsi and teres major posteriorly.
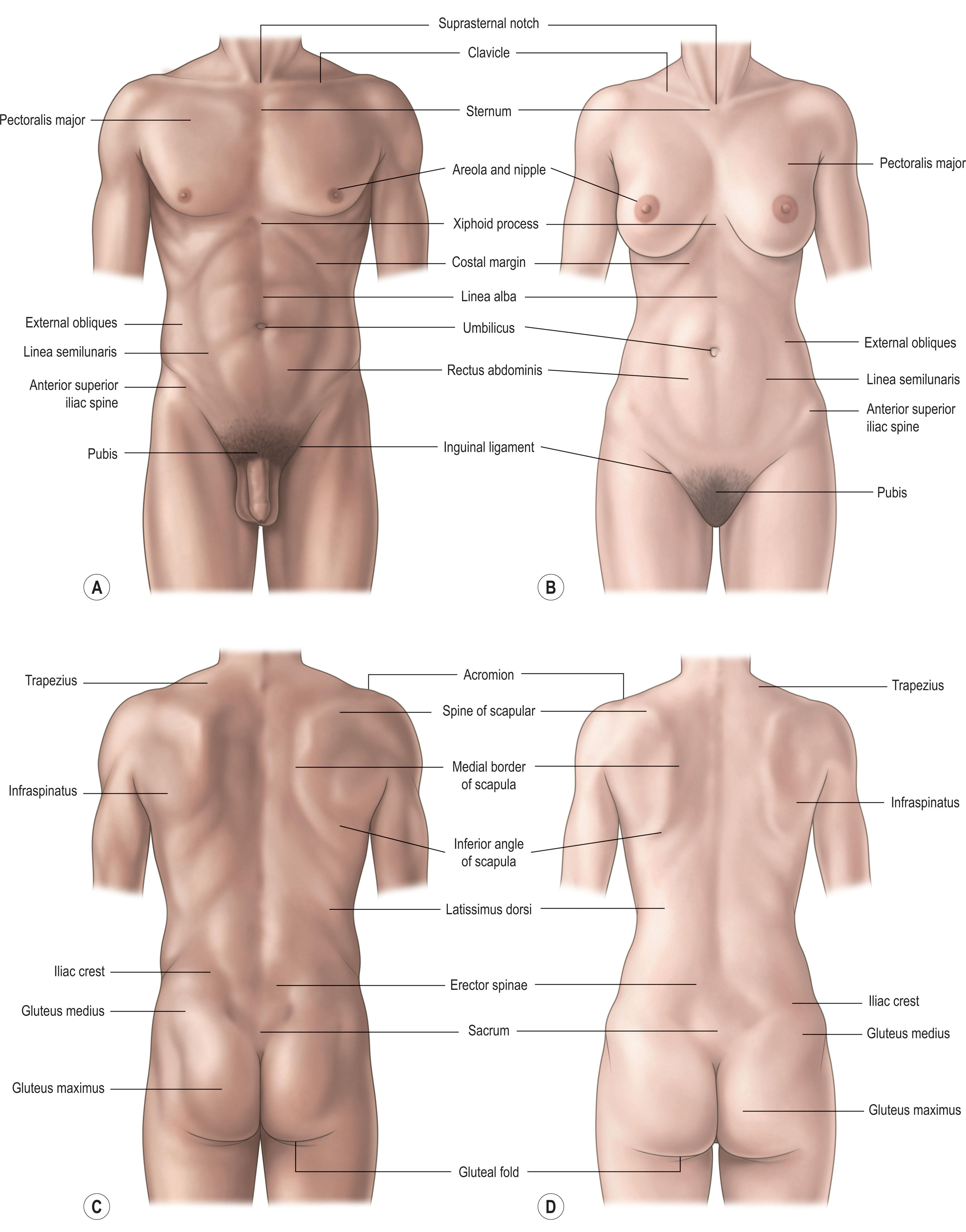
A description of the surface anatomy of the abdomen begins with the umbilicus, a midline remnant of the umbilical cord attachment, which is generally located at the L3–L4 level. Deep to the umbilicus, at the midline, is the linea alba (“white line” in Latin), which runs from the xiphoid process to the pubic symphysis and is a dense white structure formed by the fusion of the components of the anterior abdominal wall. This structure can be seen externally as the midline recess between the two halves of the rectus muscles. Running perpendicularly through the linea alba lie the rectus abdominis inscriptions, which are three tendinous bands coursing through the rectus sheaths. These inscriptions are what form the well-defined anatomic division of the rectus into three pairs. Laterally, the anterior superior iliac spine (ASIS) is a key surface landmark that is often used for orientation and operative planning in abdominal surgeries. This structure represents the superior-most projection of the iliac crest and is found at the level of the L4 vertebra.
In the posterior thorax, the most superior landmark is the trapezius muscle. The trapezius is a large, tripartite muscle which attaches to the occipital bone superiorly, the cervical and thoracic vertebrae medially, and the acromion and scapular spine laterally. Just deep and inferolateral to the trapezius lie the scapular spines, bilaterally. The scapular spines are key points of attachment for the functional muscles of the shoulder and can be palpated on the posterior thorax bilaterally as they travel transversely from the level of the T3 vertebra to the acromion. Inferior to the scapular spines lies the latissimus dorsi, one of the workhorse flaps in plastic surgery and the largest muscle in the upper body, which inserts on the humerus and originates on T7–L5 vertebrae, the iliac crest, and the inferior angle of the scapula (with known anatomic variations). The posterior superior iliac spine (PSIS) is the posterior border of the ala and is located at the midpoint between the S1 and S2 vertebrae. The PSIS can be palpated along the back as the “dimples” found superior to the buttocks. The sacral promontory, just inferior and medial to the PSIS, is the portion of the sacrum that articulates with the final lumbar vertebra and is the posterior border of the pelvic inlet. The intergluteal cleft is the ridge formed between the two buttocks that runs from the sacrum to the perineum anteriorly. Laterally within the perineum lie the ischial spines. These spines serve as the posterior borders of the ischium and are key structures in anesthetic nerve blocks. Just superficial and inferior to the ischial spines lies the gluteal fold, the crease formed by the terminal gluteus maximus at the inferior-most aspect of the buttock as it meets the posterior thigh. Finally, the greater trochanter of the femur is a bony eminence on the femur located approximately 2–4 cm inferior and lateral to the femoral head. This structure serves as a key point for muscular attachment and may be a source of pressure in trochanteric pressure ulcers.
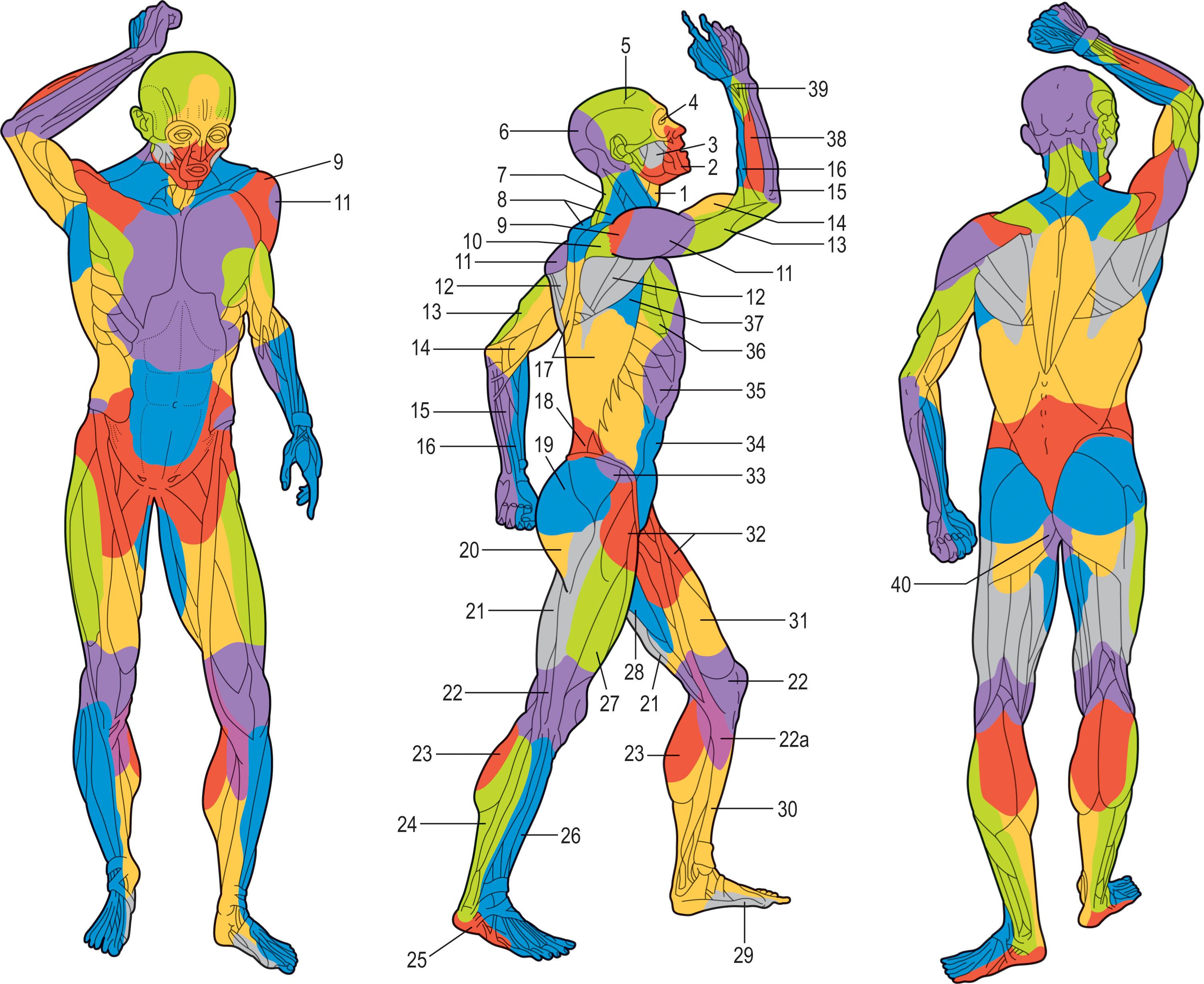
Initially described in 1987 by Taylor and Palmer, the angiosome concept has proven to be useful for designing tissue flaps. An angiosome is an individual composite unit of skin and its underlying soft tissues which is typically supplied by a source vessel. This concept has been further developed to include angiosomal regions supplied by choke vessels, which are smaller-caliber vessels between angiosomes that can dilate to supply neighboring tissue when operatively delayed or with decreased sympathetic input. The small vessels that typically create the angiosome are called perforators and exit the muscle fascia to perfuse a specific region of skin. The concept of angiosomes has been extended into perforasomes to allow for surgeons to plan tissue flaps.
Consistent with the functional nature of the area, the skin of the trunk is generally thick. This is especially true for the back, which has some of the thickest skin in the body. In general, the skin serves as a mechanism for protection from the outside world, thermoregulation, and synthesis of vitamin D. The skin comprises two layers. Most superficially, the epidermis comprises five sublayers (stratum basale, spinosum, granulosum, lucidum, and corneum). Deep to the epidermis is the dermis, which primarily drives skin thickness and is composed of two sublayers (reticular and papillary). Due to the thick nature of the regenerative dermis, skin grafts taken from the back and buttock region are favorable for healing. Wound healing is also favorable in the trunk region due to the available laxity of surrounding tissues and the robust dermis. However, several challenging scenarios can occur within these regions. When radiation is used for breast cancer treatment, the skin of the upper chest and axilla may become highly fibrotic, creating functionally limiting tightness and scar contracture. Additionally, the skin of the upper anterior trunk is highly susceptible to hypertrophic scar following surgical injury (port placement, median sternotomy, etc.).
The anterior chest has both functional and aesthetic contributions. The muscles and ribs serve to protect the contents of the chest cavity and assist in respiration. In the male chest, the pectoralis muscles are easily seen and often outwardly reflect physical strength of the individual. In the female chest, the breast form may reflect beauty and attractiveness relative to reproductive potential. The breast gland is also highly susceptible to cancer, and reconstruction of the breast and chest is a common procedure in which anatomic appreciation is at a premium.
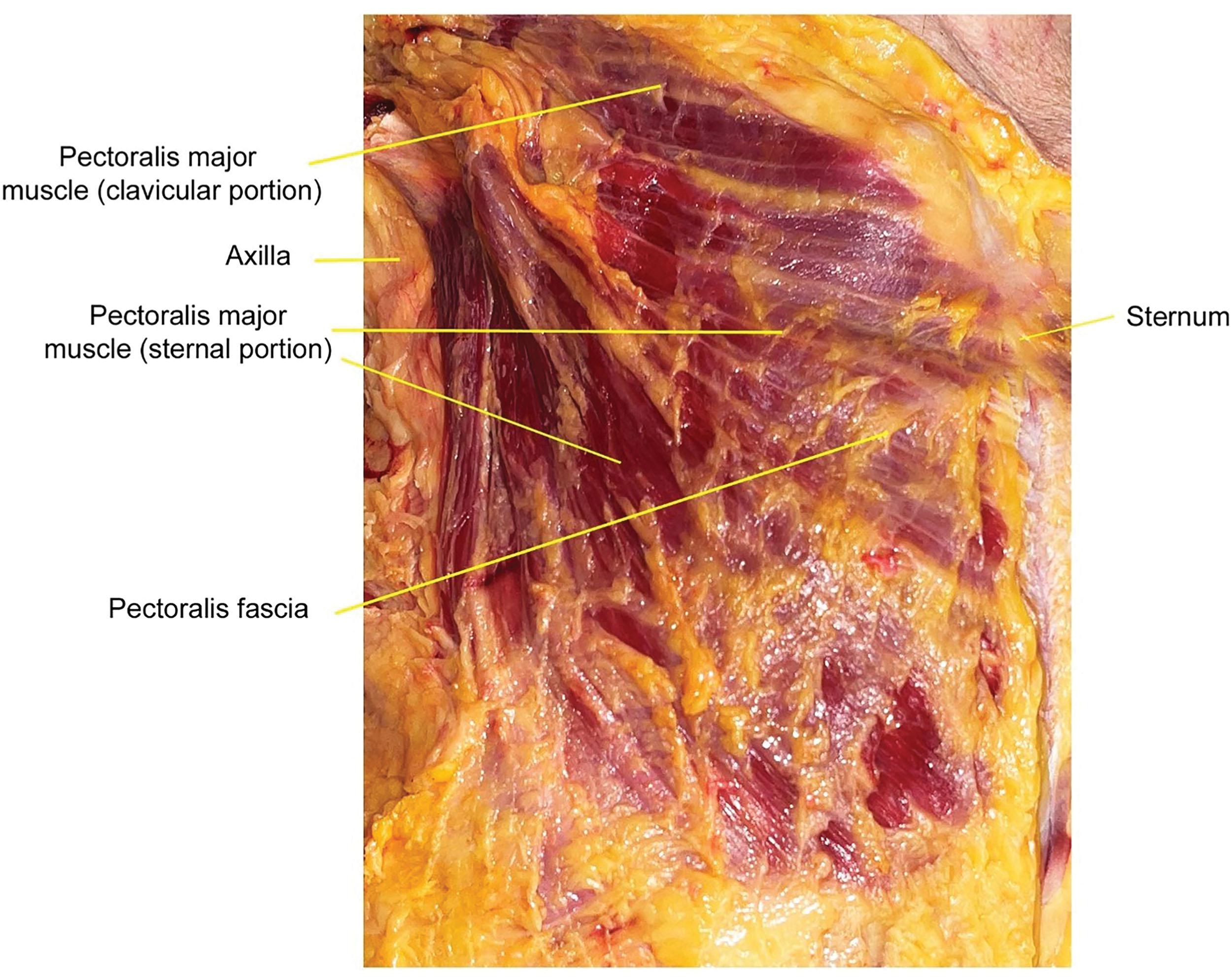
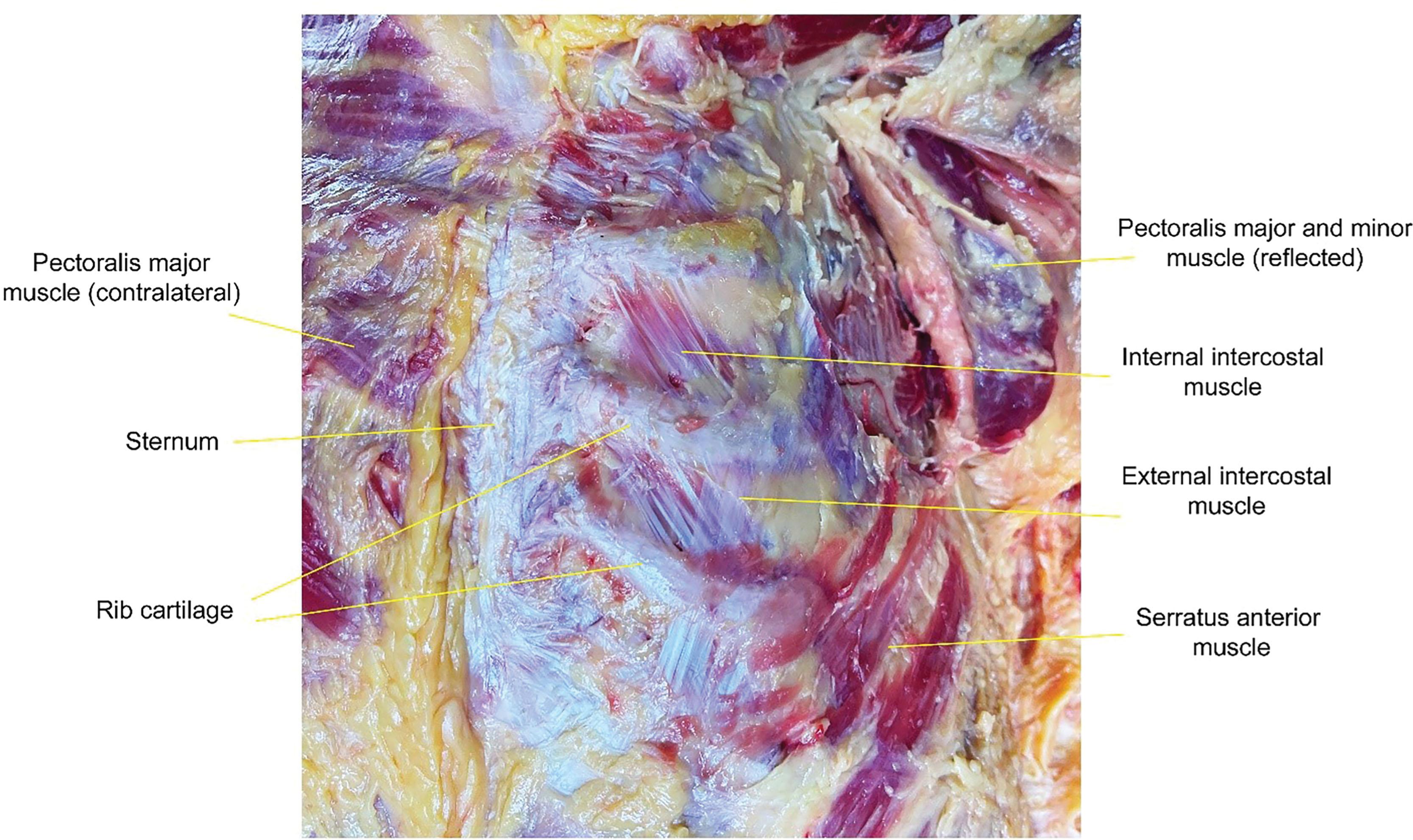
The pectoralis muscles of the anterior chest are frequently encountered during surgery and serve as landmarks for many procedures. The pectoralis major has two portions that originate from the humerus. The first is the clavicular portion, and the second is the sternal portion ( Fig. 10.3 ). In patients with Poland syndrome, it is common that the sternal portion of the pectoralis major is missing. The lower lateral portion of the pectoralis muscle is loosely adherent to the chest wall and is frequently elevated to cover a breast implant. The pectoralis major is considered a type V flap due to the predominant blood supply from the thoracoacromial artery ( Fig. 10.4 ) and secondary segmental blood supply from internal mammary artery perforating vessels. Innervation is supplied by the medial and lateral pectoral nerves. Just deep to this muscle lies the much smaller pectoralis minor, which has a similar blood supply and innervation. Utility of this muscle within reconstructive surgery is rare, however, it can be used as a free flap for functional muscle transfer. Deep to the pectoralis muscles lie the intercostal muscles, which are located between the ribs and found in a complex of three, with the external, internal, and innermost intercostal being listed from superficial to deep ( Fig. 10.5 ). The intercostal muscles receive their primary blood supply and innervation from the intercostal vessels, direct branches of the internal mammary artery anteriorly and the aorta posteriorly, and the intercostal nerves. These neurovascular bundles are found on the posterior–inferior aspect of the rib – a key surgical landmark for chest wall procedures involving the rib.
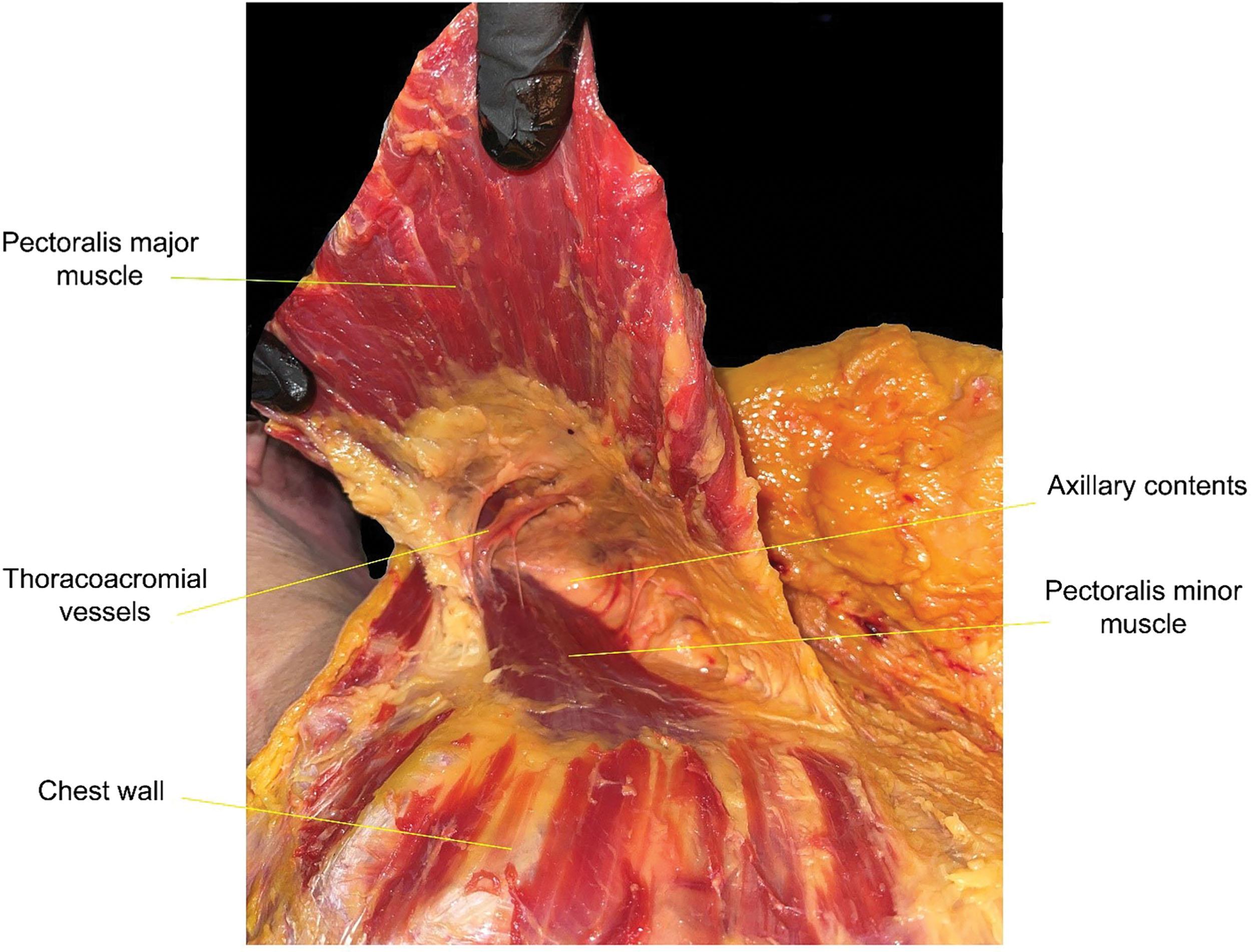
While the internal mammary artery is a key vessel in blood supply to the muscles of the anterior chest wall, it is also commonly used as a free flap recipient vessel. The internal mammary artery is a branch of the subclavian artery and can be found just deep to the costochondral cartilage found at the articulation between the sternum and the rib. As a donor, these vessels (artery and vein) are most often dissected at the level of the third rib due to size-match considerations with the recipient vessel.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here