Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Infections constitute one of the biggest problems in dermatology in tropical countries of the developing world.
However, tropical infections may also be seen in countries in which they are non-endemic—among visitors and immigrants, or when acquired abroad by the indigenous population.
Leprosy is a chronic disease caused by Mycobacterium leprae. This is an acid- and alcohol-fast bacillus that cannot be cultured in the laboratory. Nasal droplets spread the infection, and the incubation period is several years. The disease is usually acquired in childhood, as the risk to exposed adults is about 5%. Leprosy is no longer endemic in northern Europe. In several developing countries the World Health Organization has coordinated leprosy elimination programmes that are succeeding. Pockets of endemicity are still found in Angola, Brazil, Central African Republic, Congo, India, Indonesia, Madagascar, Mozambique, Nepal and Tanzania.
The manifestation of the disease depends on the degree of the delayed (type IV) hypersensitivity response in the infected individual. Those with strong cell-mediated immunity develop the tuberculoid paucibacillary type, whereas those in whom cell-mediated reactivity is poor develop lepromatous multibacillary leprosy. Borderline lesions are seen in those whose immune state is intermediate.
M. leprae has a predilection for nerves and the dermis but, in the lepromatous type, infection may be much more widespread. Tuberculoid leprosy is characterized by a granulomatous reaction in the nerves and dermis with no acid-fast bacilli demonstrated using the Ziehl–Neelsen stain. In contrast, bacilli are plentiful in the dermis of the lepromatous type, and large numbers of macrophages are seen on microscopy.
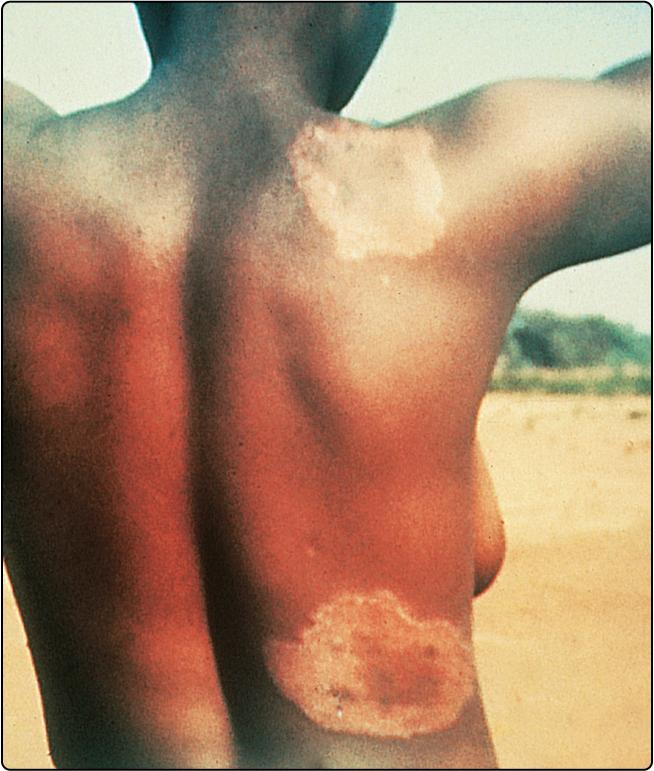
Tuberculoid leprosy affects the nerves and the skin. Nerves may be thickened, and anaesthesia or muscle atrophy is found. Skin lesions often occur on the face, and as few as one or two may be seen. They usually take the form of raised red plaques with a hypopigmented centre, which is typically dry and hairless ( Fig. 34.1 ). Sensation may be impaired within the plaque.
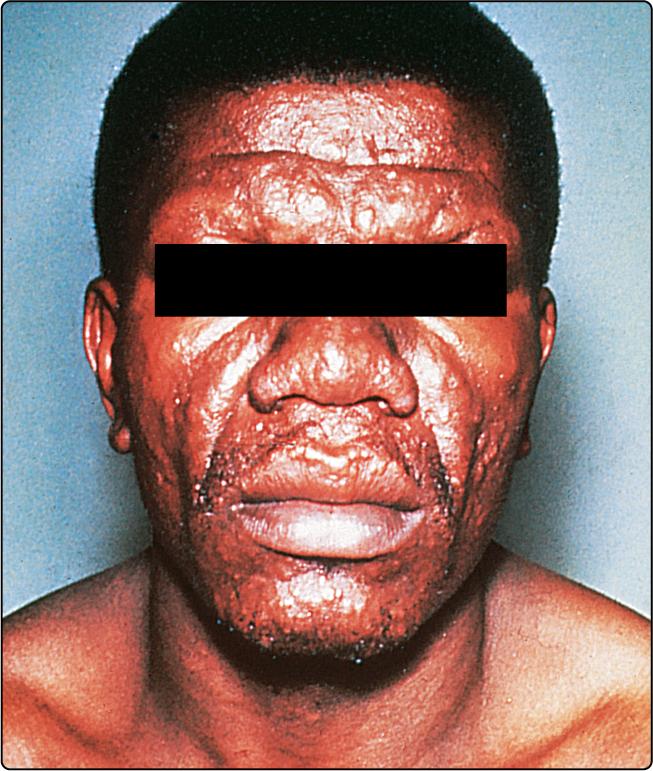
The skin lesions of lepromatous leprosy are more numerous and take the form of macules, papules, nodules and plaques. They are symmetrical and tend to involve the face, arms, legs and buttocks. Sensation is not impaired. Untreated, the condition is infectious from the nasal involvement. Progression gives a thickened furrowed appearance to the face (leonine facies) with loss of eyebrows ( Fig. 34.2 ). Borderline leprosy shows features intermediate between lepromatous and tuberculoid.
Leprosy must be distinguished from a variety of other dermatological conditions ( Table 34.1 ).
| Type of leprosy | Differential diagnosis |
|---|---|
| Tuberculoid | Vitiligo, pityriasis versicolor, pityriasis alba, sarcoidosis, lupus vulgaris, granuloma annulare, post-inflammatory hypopigmentation |
| Lepromatous | Disseminated cutaneous leishmaniasis, yaws, guttate psoriasis, discoid lupus erythematosus, mycosis fungoides |
Tuberculoid leprosy may result in bone damage to a hand or foot from repeated trauma to an insensitive area. In lepromatous leprosy, nasal damage may progress to a saddle nose defect. Ichthyosis, testicular atrophy and leg ulcers are seen. A peripheral neuropathy leads to shortening of the toes and fingers from repeated trauma. Lepra reactions, which result from an upgrading or a downgrading of the immune response, can produce nerve destruction or acute skin lesions.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here