Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Schistosomiasis, which is classified as a neglected tropical disease, is a parasitic infection caused by the trematode worms (blood flukes) of the genus Schistosoma. It has been reported in 78 countries worldwide, with 290 million people infected and nearly 800 million at high risk for infection. Mortality from schistosomiasis is estimated at 13,000 deaths per year, and the burden of disease at 3.3 million disability-adjusted life-years lost per year.
Six major species of Schistosoma affect humans and cause two main forms of schistosomiasis: intestinal ( S. mansoni, S. japonicum, S. intercalatum, S. mekongi, and S. guineensis) and urogenital ( S. haematobium) . Schistosomas are long, cylindrical worms. The large male (6 to 11 mm × 2 to 4 mm) has a ventral gynecophoric canal in which the female (7 to 28 mm × 1 to 2 mm) is held during copulation.
Schistosomiasis occurs mainly in areas with poor sanitation in rural, periurban, and urban areas in endemic countries. The World Health Organization has set a goal of eliminating schistosomiasis by 2030, but schistosomiasis is still endemic in 78 countries. S. mansoni is found in the Arabian Peninsula, Egypt, Libya, Sudan, most countries in sub-Saharan Africa, Brazil, Suriname, and Venezuela. S. mansoni is found in Africa, South America (Brazil, Venezuela, and Surinam), and the Caribbean. S. haematobium is found in Africa and the Middle East, S. japonicum in China and the Philippines, S. intercalatum in West and Central Africa, S. mekongi in Southeast Asia, and S. guineensis in Cameroon, Equatorial Guinea, Gabon, and Sao Tomé.
The endemicity of schistosomiasis depends on the urban disposal of urine (S. haematobium) and feces (S. mansoni, S. japonicum, S. intercalatum, S. mekongi, S. guineensis), the presence of suitable snail hosts, and human exposure to cercariae. The freshwater snail intermediate hosts are Biomphalaria species in Africa and Biomphalaria glabrata (Australorbis) and Tropicarbis in South America and the West Indies. In some cases, the endemicity of schistosomiasis may be maintained by animal reservoirs. Such is the case with S. japonicum, which infects dogs and cows.
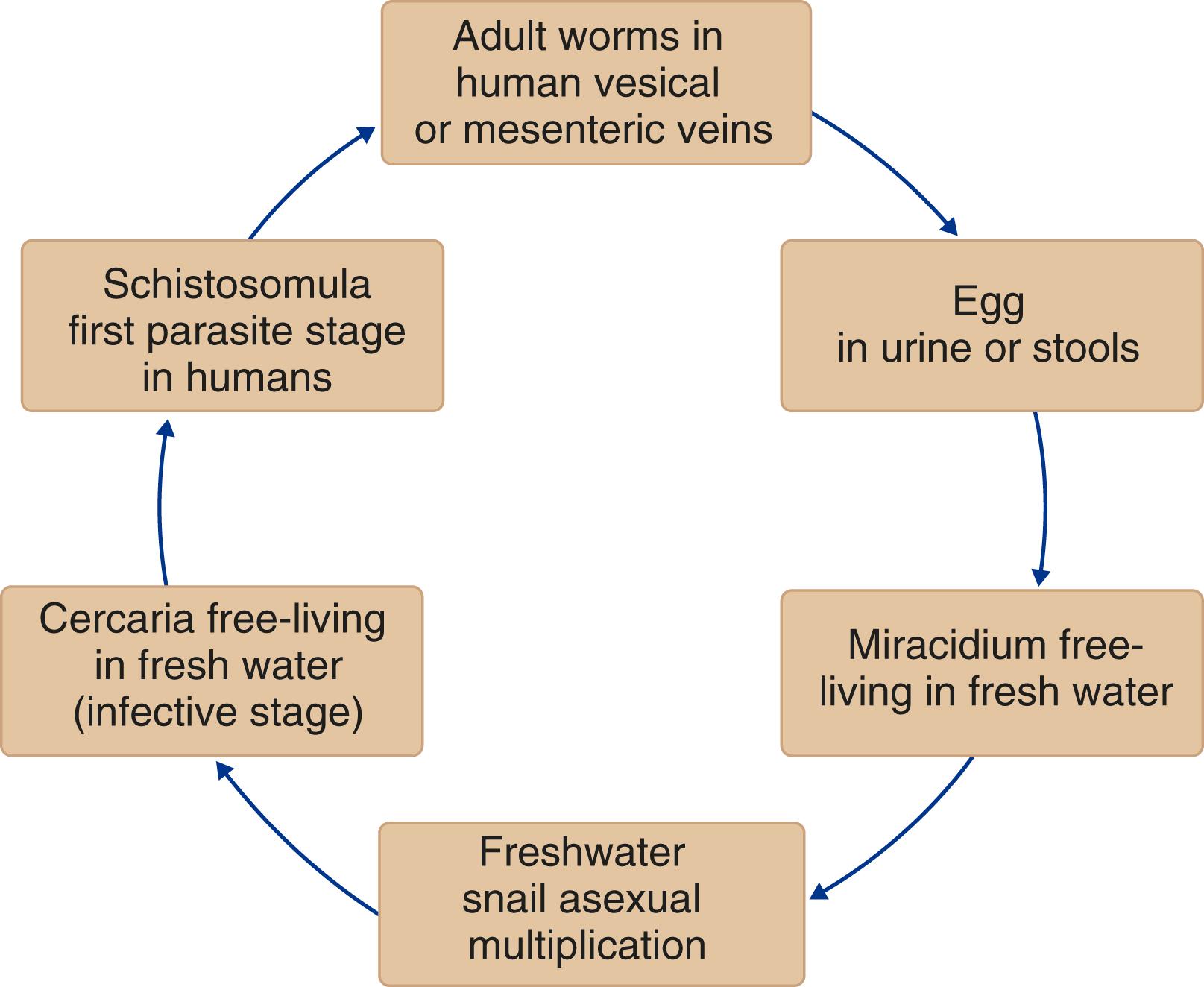
Adult worms live in the mesenteric veins ( S. mansoni , S. japonicum, S. mekongi, S. intercalatum, and S. guineensis ) or in the venous plexus around the lower ends of the ureters and the urinary bladder ( S. haematobium ) ( Fig. 326-1 ). In these sites, they start their sexual reproduction by releasing eggs. Once deposited in the host, eggs may stay in the mesenteric vein, be trapped in the intestines, escape to the intestinal lumen, and migrate by portal blood to the liver ( S. mansoni, S. japonicum; Fig. 326-2 ). Eggs of S. haematobium, which may be trapped in the intestines and bladder, may escape to the intestinal or bladder lumen. After being excreted with feces or urine into fresh water, the eggs hatch and release ciliated motile miracidia that penetrate into snails, which are the intermediate hosts. Following asexual multiplication in the snail, the development of cercariae, which are the infective forms for humans, requires 4 to 7 weeks. After leaving the snails, the cercariae can survive in fresh water for almost 72 hours. When penetration of the skin in the human host occurs, the cercariae lose their tails and change into schistosomula. Schistosomula migrate to the lungs and, in about 6 weeks, mature to adult worms that descend to their final habitat. Viable eggs can be seen in excretions (i.e., stool or urine) 5 to 9 weeks after cercarial penetration. The lifespan of the worms ranges from 5 to 10 years.

Four main pathophysiologic mechanisms have been proposed in acute human schistosomiasis infection: a serum sickness-like hypersensitivity reaction ( Chapter 230 ), which is triggered by the deposition of eggs; a systemic hypersensitivity reaction against the migrating schistosomula and eggs; a toxemic and allergic reaction to the migrating and maturing larvae of Schistosoma, but not to eggs; and a more generalized systemic, immunologically mediated, Loeffler-like reaction, not specifically related either to larvae or to adult worms or to eggs.
In chronic schistosomiasis, tissue injury is mediated by egg-induced granulomas and the subsequent appearance of fibrosis. In S. haematobium, infected eggs induce the formation of granuloma in the urinary tract. Because the habitat of S. mansoni, S. japonicum, S. mekongi, S. guineensis, and S. intercalatum worms is the mesenteric blood vessels, the intestines are involved primarily, and egg embolism results in secondary involvement of the liver. Host genetics, immunologic response, and parasite load measured by egg count in the stool are associated with a greater chance for hepatosplenic involvement. Interleukin (IL)-4, IL-13, and IL-17 have been associated with granuloma formation and liver fibrosis. Enzymes and antigens released from eggs sensitize host lymphocytes, which migrate to areas of egg deposition and recruit other cell types, such as macrophages, eosinophils, and fibroblasts. The size of these granulomas and the resulting fibrosis lead to most of the characteristic chronic fibro-obstructive lesions in schistosomiasis. In the liver, the granulomas result in perisinusoidal obstruction of portal blood flow, portal hypertension, splenomegaly, esophageal varices, and portosystemic collateral circulation. Liver cell perfusion is not reduced; consequently, liver function test results remain normal for a long time.
In schistosome-infected populations, the intensity of infection increases during the first two decades of life as children accumulate worms, and then declines. Although exposure decreases with age, the lower intensities of infection in older individuals are due in part to acquired resistance. In the S. haematobium –infected population, immunoglobulin (Ig) E increases progressively with age, and IgE antibodies directed against adult worm antigens are associated with subsequent low intensities of reinfection. Similar associations between high IgE levels or a high IgE/IgG4 ratio and resistance to reinfection have been found among Brazilian and Kenyan subjects exposed to S. mansoni . In contrast, susceptibility to reinfection has been associated with IgG4, which may serve as blocking antibody that inhibits the action of IgE. A major codominant gene, called SM1, in the human host’s genome controls the intensity of infection by S. mansoni .
Modulation of the immune response is a characteristic of chronic schistosomiasis, and S. mansoni antigens downmodulate the immune response by increasing their production of regulatory cytokines such as IL-10 and the frequency of regulatory T cells. S. mansoni infection attenuates the clinical manifestations of type 1 diabetes and experimental autoimmune encephalitis in mice. In humans, S. mansoni attenuates the clinical manifestations of asthma and is inversely associated with the development of myelopathy related to human T-cell leukemia virus type 1 (HTLV-1) infection ( Chapter 360 ). S. mansoni infection may impair immunologic response to vaccines and change manifestations of other infectious diseases.
Clinical manifestations of schistosomiasis are divided into schistosome dermatitis, acute schistosomiasis, and chronic schistosomiasis. Schistosome dermatitis, or swimmer’s itch, is seen mainly when avian cercariae penetrate the skin and are destroyed. Schistosome dermatitis is a sensitization phenomenon that occurs in previously exposed persons. The cercariae evoke an acute inflammatory response with edema, early infiltration of neutrophils and lymphocytes, and later invasion of eosinophils. A pruritic papular rash occurs within 24 hours after the penetration of cercariae and reaches maximal intensity in 2 to 3 days.
Acute schistosomiasis occurs usually 20 to 50 days after primary exposure. Though asymptomatic in endemic areas, acute schistosomiasis is becoming a frequent and major clinical problem when nonimmune individuals from urban regions are exposed for the first time to a heavy infection in an endemic area. The clinical syndrome (i.e., fever, chills, liver and spleen enlargement, and marked eosinophilia) originally described for S. japonicum infection, and still common for this species, is increasingly being diagnosed in Brazil and Africa in individuals with S. mansoni infection. Malaise, diarrhea, weight loss, cough, dyspnea, chest pain, restrictive respiratory insufficiency, and pericarditis are also documented in this phase. Acute disease is not observed in individuals who live in endemic areas for schistosomiasis.
In chronic schistosomiasis, intestinal involvement commonly manifests with abdominal pain, irregular bowel movements, and blood in the stool. Hepatosplenic involvement is the most important cause of morbidity with S. mansoni and S. japonicum . Patients may remain asymptomatic until the manifestation of hepatic fibrosis and portal hypertension develops. Bleeding esophageal or gastric varices may cause hematemesis. Anemia and decreasing levels of serum albumin are observed. Some patients develop severe hepatosplenic disease, with jaundice, ascites, and hepatic failure.
Concomitant infection by Salmonella species ( Chapter 284 ) and, to a lesser extent, other gram-negative bacteria with S. mansoni or S. haematobium leads to a picture of prolonged fever, hepatosplenomegaly, and mild leukocytosis with eosinophilia. Coinfection with S. mansoni and hepatitis B or C virus ( Chapters 134 and 135 ) exacerbates liver pathology.
Glomerulonephritis ( Chapter 107 ) and hypersplenism ( Chapter 154 ) are other complications associated with hepatosplenic schistosomiasis. Pulmonary hypertension ( Chapter 69 ), which is increasingly recognized with the use of more advanced diagnostic technology, is detected in about 10% of patients with liver fibrosis. In countries endemic for S. mansoni, up to 30% of all cases of pulmonary hypertension are due to schistosomiasis.
Cerebral schistosomiasis, which is observed in patients with S. japonicum infection, may occur as early as 6 weeks after infection, and its most common manifestation is focal seizures. Signs and symptoms of generalized encephalitis may occur. In S. mansoni infection, neurologic involvement is mainly characterized by transverse myelitis.
An association between S. mansoni or S. haematobium and human immunodeficiency virus (HIV) infection has been documented in areas where both infections are present. Although the immune response of patients with schistosomiasis is altered by HIV, it has not been reported to be associated with any clear changes in the degree of infection or severity of manifestations of schistosomiasis.
In S. haematobium infection, the main organ system involved is the urinary tract. The acute granulomatous response to parasite eggs in the early stages causes urinary tract disease, such as urethral ulceration and bladder polyposis. In chronic disease, usually in older patients, granulomas at the lower ends of the ureters obstruct urinary flow and may cause hydroureter and hydronephrosis. Bladder fibrosis and calcification are also seen in this phase. Up to 70% of infected individuals have hematuria, dysuria, or urinary frequency. Radiologic findings include hydronephrosis, hydroureter, ureteral strictures, dilation or distortion, ureteral calcifications, ureterolithiasis, calcified bladder, polyps, reduction in bladder capacity, irregular contraction of the bladder wall, or a dilated bladder because of bladder neck fibrosis. An increased incidence of squamous cell urothelial carcinoma of the bladder ( Chapter 182 ) is seen in endemic areas of S. haematobium infection. Female genital schistosomiasis can lead to infertility and a higher risk of HIV transmission. S. haematobium eggs have occasionally been found in the lungs, with subsequent focal pulmonary arteritis and pulmonary hypertension.
Epidemiologic risk factors such as a history of contact with contaminated water and appropriate clinical manifestations are key to raise suspicion of schistosomiasis. About 50% of infected patients have eosinophilia. Liver enzymes and the serum bilirubin level are usually normal or mildly elevated. Anemia and thrombocytopenia may occur in severe chronic schistosomiasis. Hematuria is common in S. haematobium .
Molecular techniques to detect schistosoma DNA in stool, urine, and blood specimens have a high sensitivity for diagnosing acute infection and are very useful in returning travelers and in individuals who may have light infection. Quantification of circulating cathodic antigen (CCA) in urine also has a high sensitivity and can monitor the efficacy of antischistosome chemotherapy. A significant decrease in antigen levels is observed as early as 10 days after therapy. Serologic assays can detect antibodies to S. mansoni antigens but cannot distinguish between active and past exposure. As a result, they can be very useful for diagnostic purposes in travelers with suspected acute infection but not for residents in endemic areas.
Despite the appeal of these molecular and immunologic tests, examination of the stool for eggs is an essential part of the evaluation, and a definitive diagnosis still often requires finding schistosome eggs in stool, urine, or a biopsy specimen, usually from the rectum ( Table 326-1 ). , Because schistosome eggs may be few, concentration by sedimentation should be performed. All eggs from stools, urine, or tissues should be examined under high power to determine their viability by visualizing the activity of cilia of the excretory flame cells of the enclosed miracidium. Dead eggs may persist for a long time after successful therapy or natural death of the worms. The presence of only dead eggs does not necessarily require treatment. Because the intensity of infection is associated with morbidity, quantitative techniques are recommended. For S. mansoni and S. japonicum, the Kato-Katz thick smear method is used. In patients with chronic S. mansoni and S. japonicum infection and liver disease, the diagnosis is sometimes made by documentation of eggs in liver specimens. Ultrasonography allows determination of the degree of liver fibrosis. S. mekongi and S. intercalatum infections are diagnosed by examining the stool for eggs.
| SCHISTOSOME | EGGS | DIAGNOSIS |
|---|---|---|
| S. haematobium | Mainly found in urine but may be found in stools or rectal biopsy specimens Eggs: 143 × 50 µm; spindle shaped: rounded anterior, conical posterior, tapering to a terminal delicate spine |
PCR in serum: 90% of patients in acute infection are positive Obtain urine sample at midday (when eggs are excreted); more than one sample may be needed PCR in urine is more sensitive than microscopy and is highly specific Examine urine directly or by filtering 10 mL of urine through a nucleopore membrane Urine-circulating antigen test for diagnosis of light infection and serologic test to diagnose early or light infection Rectal biopsy in suspected cases with negative urine for egg and for circulating cathodic antigen |
| S. mansoni | Found in stool eggs: 155 × 66 µm; oval with lateral, long spine | PCR in serum: 90% of patients in acute infection are positive Examine stool for eggs PCR of stool is more sensitive than microscopy and is highly specific Use the Kato-Katz thick smear method for quantification purposes Urine-circulating cathodic antigen test, serologic testing, or rectal biopsy to diagnose stool-negative cases, particularly in lightly infected patients |
| S. japonicum | Found in stool Eggs: 89 × 67 µm; oval or rounded with a lateral, short, sometimes curved spine |
Examine stool for eggs Kato-Katz thick smear (for quantitative assessment) Urine-circulating cathodic antigen test, serologic test or rectal biopsy for those with light infections, especially with less common manifestations (e.g., cerebral schistosomiasis) Nested PCR is promising for diagnosis in endemic areas |
| S. mekongi | Found in stool Eggs: 60 × 32 µm; smaller than eggs of S. japonicum |
Examine stool for eggs |
| S. intercalatum | Found in stool Eggs: 180 × 65 µm; terminal spine |
Examine stool for eggs |
Urine examination for S. haematobium eggs can be performed by direct or concentration methods. Samples should be obtained at midday, when excretion of eggs is maximal. Assessment of urinary tract pathology by ultrasonography is recommended after the diagnosis is confirmed because of the increased incidence of carcinoma of the bladder ( Chapter 182 ).
Praziquantel, which is a pyrazinoisoquinoline derivative, is the drug of choice for the treatment of schistosomiasis. The standard recommended treatment is a single dose of praziquantel, 40 mg/kg, for S. mansoni, S. haematobium , and S. intercalatum infection. In S. japonicum infection, a total dose of 60 mg/kg is recommended, split into two or three doses in a single day. For S. haematobium, overall cure rates are similar with single-dose (40 mg/kg) and double-treatment (40 mg/kg with 2-week interval) praziquantel, but double treatment significantly reduces the intensity of infection and microhematuria, so it may reduce morbidity. S. mekongi may require two treatments at 60 mg/kg body weight.
Oxamniquine (40 mg/kg) is also effective as an alternative to praziquantel. Combination therapies, such as single-dose praziquantel plus dihydroartemisinin piperaquine (40 mg/320 mg), may be even more efficacious for the treatment of intestinal schistosomiasis.
The most common adverse events observed with praziquantel or oxamniquine are related to the gastrointestinal tract: abdominal pain or discomfort, nausea, vomiting, anorexia, and diarrhea. These symptoms can be observed in up to 50% of patients but are usually well tolerated.
Mass drug administration with praziquantel has been used as the mainstay of programs for the control and prevention of schistosomiasis morbidity, with school-based programs showing the most promising results. , However, this approach alone is not sufficient to eliminate or interrupt transmission of this disease. The development of anti- Schistosoma vaccines is necessary. Additional measures such as provision of clean water, use of molluscicides, adequate sanitation, and improvement of socioeconomic conditions also should be implemented to control the disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here