Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vertebral compression fractures are the most common fractures due to osteoporosis. Vertebral fractures are two to three times more prevalent than hip or wrist fractures. It is estimated that a vertebral fracture due to osteoporosis occurs every 22 seconds worldwide in men and women over age 50. In the United States alone, an estimated 700,000 new osteoporotic vertebral compression fractures occur each year. A 50-year-old white female is estimated to have a 16% lifetime risk of developing a vertebral fracture compared with 5% risk in a male. As only one-third of osteoporotic vertebral compression fractures are recognized clinically, underdiagnosis of vertebral fractures is an important problem.
The estimated annual cost of treatment for vertebral compression fractures is 5–10 billion dollars in the United States. Hospital admissions for vertebral compression fractures exceed 150,000 each year, with an average cost of $12,000 per admission.
The incidence of osteoporotic vertebral compression fractures increases with age in both males and females. In a large cohort of middle-aged individuals studied with serial radiographs over two decades, 24% of women and 10% of men sustained a vertebral fracture during the study. Although the rate of fracture for men and women over age 50 is not significantly different, the prevalence of fractures is higher in females due to longer life span.
An important risk factor for development of a vertebral compression fracture is a history of osteoporotic fracture. A person who experiences a vertebral compression fracture is five times more likely to experience an additional fracture, when compared with a control with no fracture.
Additional risk factors include genetics, race, physical inactivity, smoking, high alcohol intake, prolonged use of glucocorticoids, and low body weight. The risk factors for vertebral compression fractures mirror those for osteoporosis and are classified as modifiable or nonmodifiable:
Potentially Modifiable Risk Factors
Smoking
Low body weight
Estrogen deficiency
Low calcium or vitamin D intake
Alcohol excess
Caffeine excess
Impaired eyesight despite correction
Recurrent falls
Inadequate physical activity
Poor health or frailty
Glucocorticoid use
Nonmodifiable Risk Factors
History of fracture during adulthood
History of fracture in a first-degree relative
Early or surgical menopause
Race (White, Asian)
Advanced age
Female sex
Dementia
Poor health or frailty
Following an initial compression fracture, the loss of vertebral body height leads to kyphotic deformity as the anterior spinal column load-bearing capacity is compromised. As kyphosis at the fracture site increases, the posterior elements of the spine are unloaded, which further increases the load on the compromised anterior spinal column. A vicious cycle develops, which leads to progressive spinal deformity and additional fractures.
Osteoporotic vertebral compression fractures have a significant impact on health-related quality of life (HRQOL) measures. A review of 600 patients with various osteoporotic fractures demonstrated that after 2 years from injury, those with vertebral fractures improved slightly from baseline, but still had significant impairment in both physical and mental domains on HRQOL as measured with the 36-Item Short Form Survey (SF-36). In contrast, those with wrist or shoulder fractures returned to normal function after 2 years. Studies have documented an increased mortality risk following osteoporotic vertebral compression fractures compared with a control group. The increased risk of death following vertebral fracture is higher for men (72% survival) than women (84% survival) at 5 years.
Osteoporotic vertebral compression fractures occur most commonly at the thoracolumbar junction and the midthoracic region but may occur at any location along the spinal column. Cervical osteoporotic fractures are less prevalent than thoracic or lumbar fractures. Fractures above the T5 level are considered as suspicious for a possible spinal tumor.
Vertebral compression fractures may present as acute , subacute , or chronic deformities. Statistics show that approximately one-third of radiographically detectable vertebral compression fractures are recognized clinically.
Patient evaluation begins with a detailed history and physical examination. Important elements of the history include acuity of pain onset, antecedent trauma, height loss, and prior fractures. Query of medical conditions that affect bone mineral metabolism, such as renal failure, hypogonadism, or chronic steroid use, is important. The onset of symptoms may be insidious, with a specific inciting event reported only in 40% of patients. Pain is often described over the posterior spinal region near the level of the fracture. In some cases, pain may radiate along the chest or abdominal wall, or to proximal or distal spinal regions. Symptoms of back, flank, sacral, or abdominal pain in a patient with risk factors for osteoporosis should prompt consideration of a vertebral compression fracture.
On physical examination , the entire spine should be palpated to identify areas of tenderness because the level of the fracture often exhibits point tenderness with palpation or percussion over the posterior spinous process. Although usually normal, a thorough evaluation of motor strength, sensation, and reflexes in the upper and lower extremities should be documented.
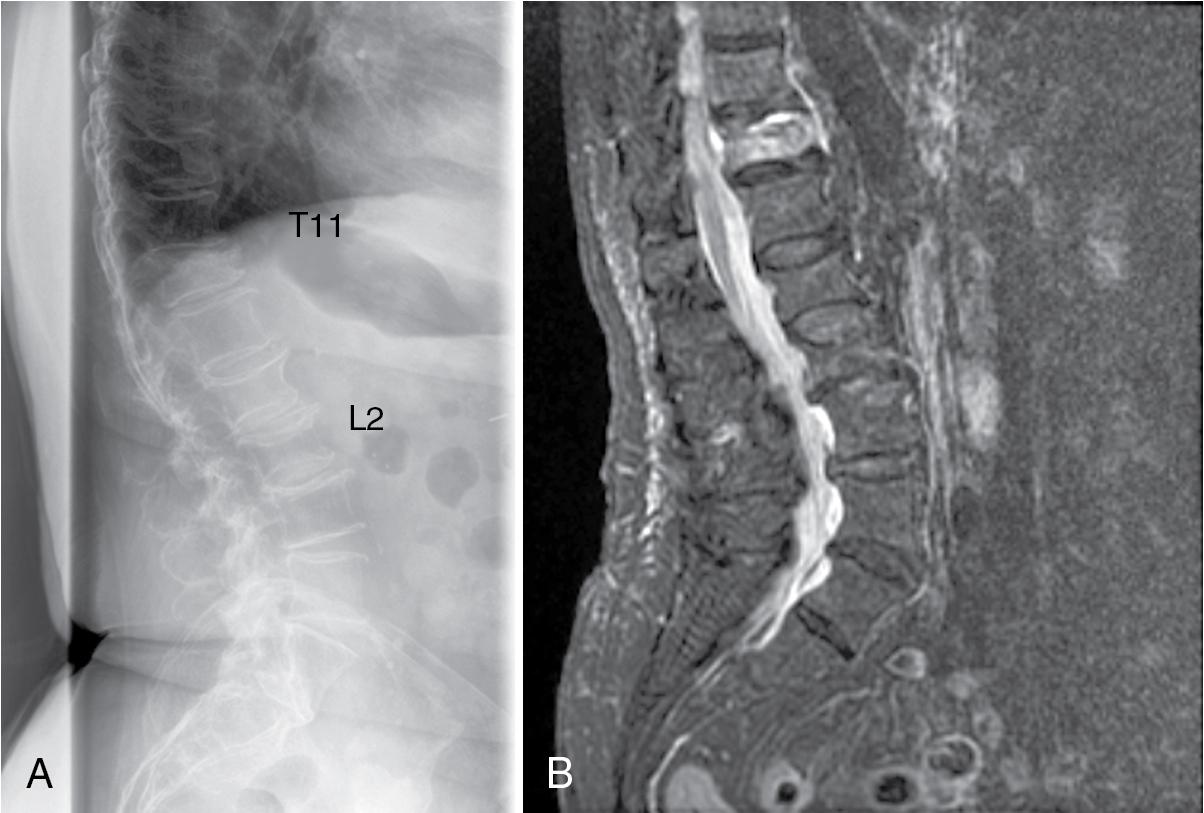
Plain radiographs of the spine are recommended as an initial imaging study and are evaluated for the characteristic loss of vertebral height associated with a fracture. Advanced imaging is helpful. Magnetic resonance imaging (MRI) or a combination of a computed tomography (CT) and technetium-99m bone scan are valuable when the acuity of the fracture is in question or when metastatic disease is a consideration ( Fig. 65.1 ). If CT is performed, bone mineral density can be estimated by measuring the Hounsfield units against established norms using software.
Dual-energy x-ray absorptiometry (DEXA) scanning to determine bone density is recommended for women aged ≥65 and men aged ≥70 years, men and postmenopausal women aged 50–69 years with clinical risk factors for fracture, adults with a fracture at age ≥50 years, as well as adults with a condition (e.g., rheumatoid arthritis) or taking a medication (e.g., glucocorticoids) associated with low bone mass or bone loss. The bone densitometer can also be used to perform a vertebral fracture assessment and screen the entire thoracic and lumbar spine for fractures.
Laboratory tests play a role when infection, malignancy, or metabolic bone disease is suspected. Tests to order include a complete blood count, comprehensive metabolic panel, C-reactive protein level, erythrocyte sedimentation rate, serum and urine protein electrophoresis, and 25-hydroxyvitamin D level.
Loss of vertebral height is assessed and described in terms of a percentage of normal height. Loss of height is described as mild (<25%), moderate (25%–40%), or severe (>40%). Vertebrae plana is a term used to describe extreme loss of vertebral body height that occurs when the vertebral body is reduced to a thin, flat shape.
Kyphotic deformity may be determined by measuring deformity at the level of the fractured vertebra or with reference to adjacent vertebrae: (1) vertebral wedge angle (angle between the superior and inferior endplates of the fractured vertebra) and (2) local kyphotic deformity (angle between the vertebral endplates above and below the level of fracture).
Vertebral body fracture morphology is described as a wedge (anterior height loss exceeds posterior height loss), crush (symmetric loss of height), or biconcave deformity. Wedge fractures are more common in the thoracic spine, while biconcave fractures are most common in the lumbar spine. Rarely, burst fractures may occur and result in retropulsion of bone into the spinal canal and may be associated with neurologic deficit.
Discontinuity of the posterior vertebral body wall is suspected in fractures with pedicle widening or loss of height exceeding 50%. CT and/or MRI are the best tests to assess integrity of the posterior vertebral body cortex.
Dynamic mobility is detected by comparing a supine cross-table lateral radiograph with a standing lateral radiograph centered at the level of fracture. Increased vertebral body height or decreased kyphotic deformity on a supine radiograph in comparison with findings on an upright radiograph suggest that vertebral height may be partially restored with a vertebral body augmentation procedure.
Intravertebral clefts (gas-filled cavities) within compression fractures may be present and represent fracture nonunion or ischemic necrosis of the vertebral body (Kümmell disease) and imply dynamic mobility at the level of fracture.
Fracture acuity is difficult to determine from a single plain radiograph. Change in fracture configuration over time with loss of height supports the diagnosis of an acute or subacute fracture. Acute fractures are often defined as less than 3 months of age, while chronic fractures are defined as greater than 3 months of age.
MRI is the single best imaging study for evaluating a vertebral body compression fracture. MRI is useful to distinguish between acute and chronic fractures when a patient presents with a spinal fracture on plain radiographs. An area of increased signal on T2 images or short-tau inversion recovery (STIR) sequences and low or isointense signal on T1 sequences is indicative of an acute fracture. MRI is helpful in determining the integrity of the posterior vertebral body wall. MRI is also helpful in evaluating the patency of the spinal canal, especially if there is retropulsion associated with the fracture or in patients with preexisting spinal stenosis. MRI can also identify atypical cases where a tumor or infection is the cause of the vertebral fracture.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here