Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Despite multiple improvements in total elbow arthroplasty design, infection continues to be a potentially catastrophic complication, with reported rates of 5% to 11%. a
a References .
The incidence of infection is higher on the 5% to 11% spectrum when one is dealing with revision arthroplasty and in patients with rheumatoid arthritis. In the past few decades the infection rates have decreased since the introduction of disease-remitting agents to treat rheumatoid arthritis (see Chapter 77 ).
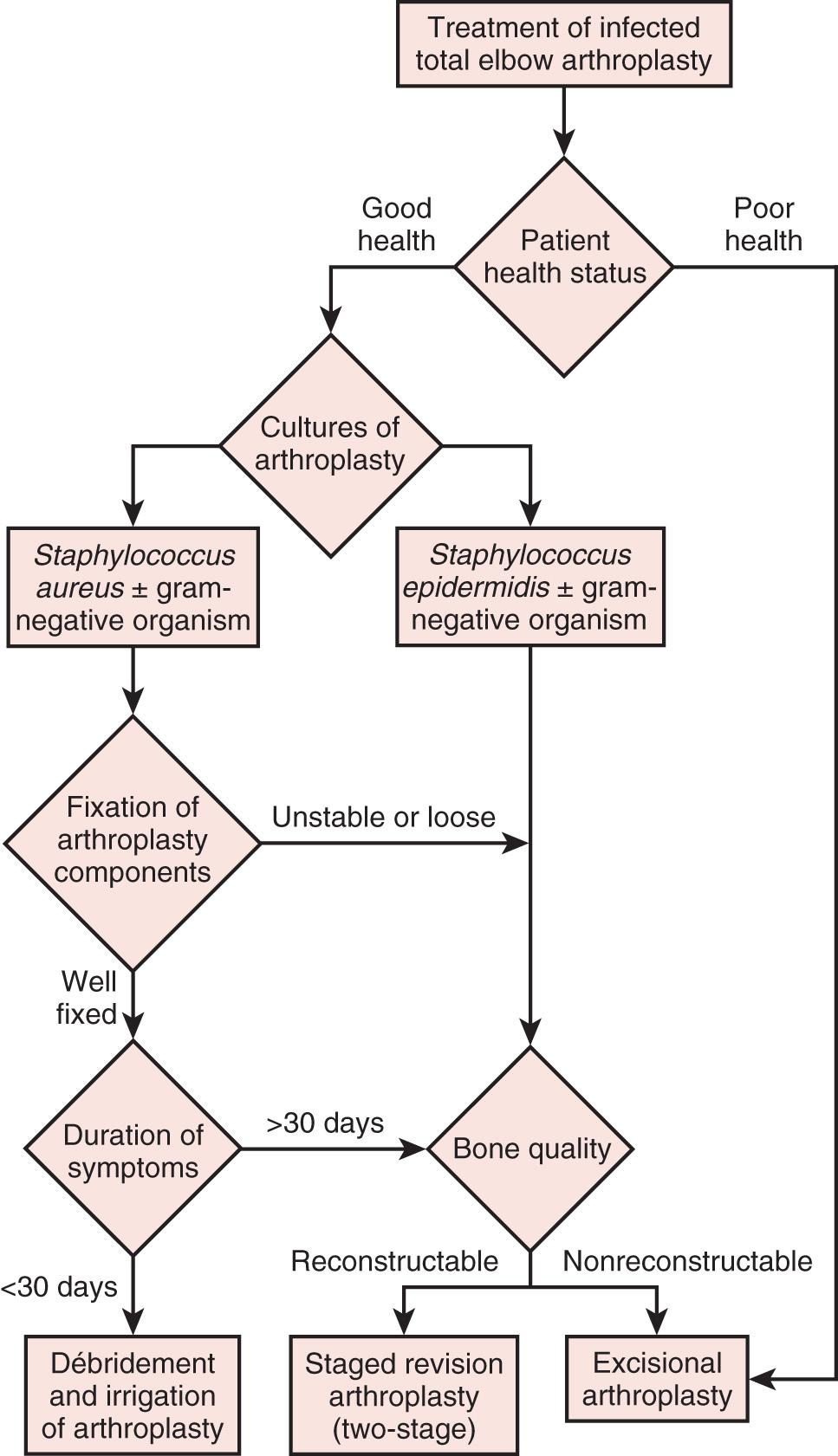
Periprosthetic infection can be addressed depending on a multitude of factors, such as the chronicity of symptoms, whether the implant is well fixed, the bone quality, the ability of the patient to withstand surgery or multiple surgical procedures, and the patient's overall health status. Treatment options include open irrigation and débridement with retention of the prosthesis, staged reimplantation, immediate exchange, and resection arthroplasty. In spite of evolving understanding of diagnosis and management, poorly functioning and sometimes painful resection arthroplasty was the definitive procedure of choice in the past, particularly in elderly patients who have relatively low demands on the elbow. Alternatively, open irrigation and débridement with retention of the prosthesis is a realistic option if the implants are well fixed. Removing a well-fixed cemented prosthesis in the elbow is often fraught with challenges associated with the fragile bone stock along the humerus and ulna. These factors affect surgical decision-making for the treatment of infected elbow arthroplasty ( Fig. 101.1 ).
Increased awareness of periprosthetic infection has led to a higher index of suspicion and earlier recognition. The rate of infection for elbow arthroplasties remains well above that for the lower extremity arthroplasties, in part because of the higher prevalence of severe rheumatoid arthritis or compromised soft tissues from failed surgical procedures such as in posttraumatic arthritis. Risk factors for total elbow infections include rheumatoid arthritis, previous surgical procedures, obesity, previous local infections and use of tumor necrosis factor antagonists. The elbow is a subcutaneous joint with a relatively thin soft tissue envelope, which increases its susceptibility to wound healing complications. Patients with rheumatoid arthritis are often immunocompromised and are taking disease-modifying antirheumatic medication, which may increase the incidence of periprosthetic infection. Patients with posttraumatic arthritis frequently have undergone multiple operations that compromise the vascularity of the soft tissues and thus increase the risk of wound healing complications. Delayed wound healing, wound drainage longer than 10 days postoperatively, and reoperation are factors associated with increased infection rates.
Posterior approaches to the elbow that involve detaching or reflection of the triceps mechanism off the olecranon may also affect wound healing. Dachs et al. reviewed 83 primary total elbow arthroplasties and found that the “triceps-off” technique versus the “triceps-on” technique was associated with a higher complication rate and included seven triceps ruptures. After attempted repair of the triceps rupture, three of seven patients developed deep infections requiring multiple surgical procedures. This highlights the importance of maintaining healthy soft tissue coverage about the posterior skin incision and keeping the triceps intact. Wound complications are often a precursor of infection.
Analogously to the previous study, persistent wound drainage is correlated with deep infection and subsequent implant removal as described by Jeon et al. They reviewed 1749 total elbow arthroplasties and found that the most common problems were delayed wound healing, drainage, and hematoma formation. Twenty-seven percent of these patients with such problems progressed to secondary deep infection. Therefore every effort should be made for meticulous wound closure and consideration of placement of a drain. Furthermore, patients with rheumatoid arthritis in that study represented 33% of the entire sample but 45.8% of those with septic complications. In one long-term series of total elbow arthroplasty, there were no reported infections after the routine use of antibiotic-impregnated cement.
The use of prophylactic antibiotics has recently been reviewed in detail. By protocol at our institutions, antibiotic cement is routinely used (1 g tobramycin per 40 g cement). We routinely implement a deep drain to prevent hematoma formation. Postoperatively, elbows are immobilized and elevated in a position of terminal extension for 24 to 36 hours to allow edema control and wound epithelialization, before we allow range-of-motion exercises. Clinically, we have found that placement of an incisional wound vacuum-assisted closure device for complex revision surgical procedures, in addition to immobilization of the elbow in terminal extension, has been helpful in the early wound healing process ( Fig. 101.2 ).

Additionally, we routinely ask patients to stop taking disease-modifying antirheumatic medication—that is, tumor necrosis factor antagonists (etanercept, infliximab, or adalimumab)—at least 2 weeks before surgery and until 2 weeks postoperatively. These medications have been associated with a higher incidence of periprosthetic infection.
Of recent interest, the application of topically administered vancomycin powder to surgical wounds has been used in spine surgery, with evidence demonstrating its efficacy and safety. It has also been shown anecdotally to reduce surgical site infection in the setting of trauma, foot and ankle surgery, and elbow surgery for capsular release. Vancomycin powder is relatively inexpensive ($10 to $12 per patient). However, given the lack of data on the efficacy of the powder in arthroplasty, the rates of allergic/adverse reactions, and the development of antibiotic resistance, it is difficult to draw definitive conclusions on the role of topical intrawound application of vancomycin powder at this time.
The most important consideration in treating a patient with an infected total elbow arthroplasty is the patient's overall health and wherewithal to endure further surgical procedures. One should consider the patient's medical condition and functional needs and expectations. Many patients with rheumatoid arthritis are medically debilitated owing to use of immunosuppressive medications, anemia of chronic disease, previous surgery, and poor nutrition.
For some low-demand patients, the only goal of surgery may be a noninfected, pain-free elbow. The most appropriate treatment for these patients may be component retention and long-term antibiotic suppression if the implant is well fixed. If the implant is loose and bone quality is severely compromised, resection arthroplasty may be a palliative operation. For patients in good health, resection is out of the question, and the preservation of function is paramount. Treatment of infection requires multiple surgical procedures and aggressive treatment associated with a high risk of complications. Thus any treatment plan should be placed in the context of the patient's needs and abilities to withstand this treatment.
The clinical presentation of an infected total elbow arthroplasty may be subtle and only recognized by one maintaining a high index of suspicion. Systemic signs of sepsis (fever and tachycardia) may be absent, with the patient reporting increased pain or pain at rest. Acute inflammation is usually detectable by local signs such as the presence of warmth, erythema, and tenderness. In some patients, there may be drainage from the wound or soft tissues.
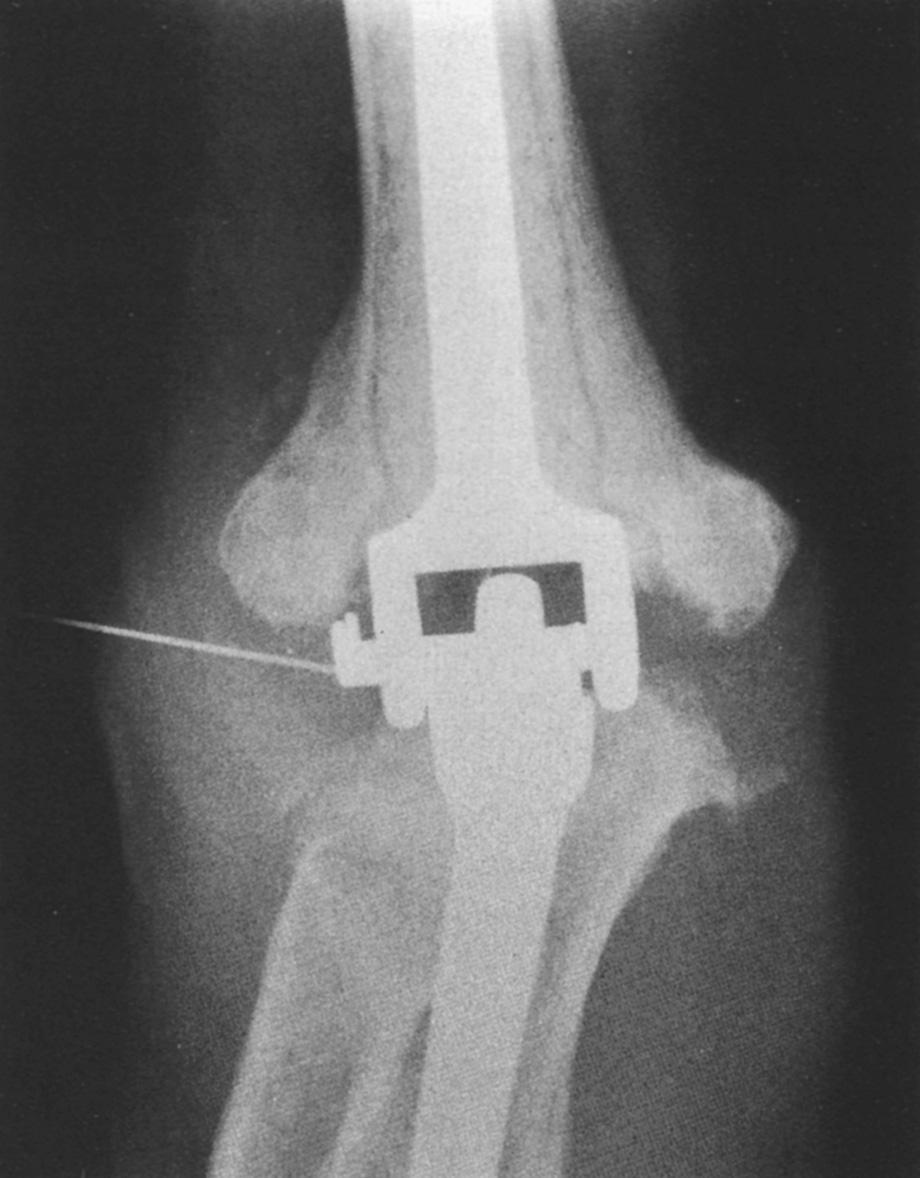
Preoperative evaluation is critical to establish range of motion, stability of the elbow, neurologic status, and function of the biceps and triceps muscles. Laboratory data may be of limited value, with most patients having a normal leukocyte count but an elevated neutrophil count on differential analysis. The erythrocyte sedimentation rate is often elevated but not specific, as many patients have systemic inflammatory disease. C-reactive protein is now routinely measured to aid in the sensitivity of detecting occult infection. The definite step is to aspirate the joint ( Fig. 101.3 ). Patients are considered infected when there are positive cultures or strong clinical suspicion (based on the presence of a draining sinus, high white blood cell count, erythrocyte sedimentation rate, C-reactive protein concentration, and operative observations) in the context of supportive microscopic pathology.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here