Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Endovascular abdominal aortic aneurysm repair (EVAR) is predicated on complete exclusion of the aneurysm from the arterial circulation. An endoleak, or continued arterial perfusion of the aneurysm sac after endovascular treatment, can compromise the effectiveness of EVAR.
There are five major categories of endoleaks ( Table 1 ). Some appear to be an unavoidable consequence of placing a stent graft inside an aneurysm sac with patent outflow vessels, some are the result of poor seal at the proximal or distal fixation sites or between the graft components, and others occur as a result of graft material failure. Endoleaks are associated with a variable increase in intrasac pressure that depends on the type of endoleak, which determines its severity and clinical significance.
| Endoleak Type | Source of Perigraft Flow |
|---|---|
| I | Attachment site |
| Ia | Proximal, aortic end |
| Ib | Distal, iliac end |
| Ic | Iliac occluder |
| II | Branch leaks |
| IIa | Simple: one patent branch |
| IIb | Complex: two or more patent branches |
| III | Stent graft defect |
| IIIa | Junctional leak or modular disconnect |
| IIIb | Fabric holes |
| IV | Stent graft porosity <30 days after implantation |
| Primary endoleak | Present from the time of EVAR |
| Secondary endoleak | Diagnosed after a prior negative CTA |
| Endotension | AAA enlargement with increased intrasac pressure after EVAR with no endoleak on CTA |
Type I endoleak continues to be a major cause of rupture after EVAR and should be considered a failure of the treatment. They are best prevented by proper patient and device selection. The incidence of type I endoleak increases with difficult anatomic situations, typically when devices are used outside the manufacturer’s instructions for use, such as short or angulated necks and landing zones with heavy calcifications. Type I endoleak is associated with significant pressure elevation in the aneurysm sac and has been linked to a continued risk of rupture, with a high of 22% mortality from rupture reported in earlier series. The risk of rupture from an untreated type I endoleak has been reported to be 3.4% at 15 months in the EUROSTAR (EUROpean Collaboration on Stent/graft Techniques for Aortic aneurysm Repair) registry, similar to the risk of rupture of an untreated abdominal aortic aneurysm (AAA). Whenever feasible, all type I endoleaks should be corrected promptly because spontaneous resolution, though possible, is not typical, and treatment can be simple with endovascular means. The initial treatment of procedural type I endoleak typically involves reballooning of the fixation sites, although additional aortic cuffs or iliac limb extensions, or placement of a balloon-expandable Palmaz stent (Cordis, Johnson & Johnson, Warren, NJ) are sometimes required.
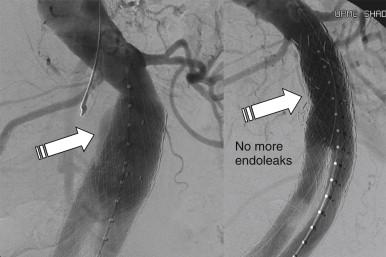
Late type I endoleaks can occur as a result of graft migration, aneurysmal degeneration of the aortic neck, enlargement of the iliac arteries, or severe angulation at the fixation site that can disengage the stent graft from the aortic wall as the sac starts to shrink. The treatment of late type I endoleaks can be more challenging, but it usually also involves ballooning, stent graft extension ( Figure 1 ), or use of Palmaz stent to increase the graft radial force and apposition to the aortic wall.
In situations where visceral branches preclude graft extension, glue or coil deposition in the track between the stent graft and the aortic wall may be successful. At the proximal attachment site, the edge of the graft can be probed with a reverse or simple-curve catheter, depending on the approach. Unless the leak is a result of gross undersizing or severe neck angulation, it often consists of a small channel alongside the graft leading to the perigraft space. A microcatheter can be advanced into this channel and embolization can be performed with microcoils, glue, or other embolic agents. It is essential to initially perform angiography of the aneurysm sac to rule out a combined type I and type II endoleak, which is not uncommon. In the case of a combined endoleak, the feeding vessel should be embolized with microcoils before the attachment site leak is treated, in order to optimize the seal and prevent adverse events from end organ damage from embolization to the colon or spinal cord. Embolization is less often required for distal type I endoleaks because a distal seal can be achieved with graft extension, and a variety of surgical or endovascular maneuvers are available to preserve hypogastric perfusion.
Open conversion is almost never required at the time of the initial EVAR, but it is sometimes required for delayed endoleak. It can be associated with increased morbidity and mortality, although several series report results that are comparable to de novo open AAA repair. This can be performed by way of a transperitoneal or retroperitoneal approach, with the initial proximal aortic control often at the supraceliac or suprarenal location, depending on the graft location and the presence of suprarenal fixation. Stepwise distal clamping is performed to reduce ischemic time, with complete or partial endograft removal. Partial explantation with in situ replacement can be performed in the absence of graft infection, with the proximal suture line incorporating the suprarenal stents, and the distal suture line of a tube or an aortoiliac graft incorporating the iliac limbs.
In one series reporting on the outcomes of reinterventions after EVAR, 51 delayed type I endoleaks with and without stent graft migration were treated by proximal stent graft extensions in 19 patients, translumbar coil embolization in 20 patients, or open surgical conversion with stent graft explants and aortoiliac reconstruction in five patients. Placement of a balloon-expandable Palmaz stent at the aortic neck was required in 14 patients, and type I endoleaks in eight patients sealed spontaneously and did not require any further intervention. Two postoperative deaths (3.9%) were reported, one from an aortoenteric fistula that developed as a procedural complication after translumbar coil embolization, and one after graft explant with aortoiliac reconstruction in a patient with prior stent graft and a Palmaz stent. Most patients can therefore be managed by endovascular means, and open conversion is sometimes required with acceptable overall morbidity and mortality.
Type II endoleaks are procedure related and are caused by patent lumbar arteries or the inferior mesenteric artery (IMA). They represent the most common type of endoleak, and the incidence has been correlated with the number of patent aneurysm branches prior to exclusion. Increased pressure in the AAA sac from retrograde flow through collateral vessels has been linked to a potential risk of continued aneurysm expansion and rupture.
Type II endoleaks occur with all graft types in about 15% of patients (10%–25%) at 1 month, but the prevalence decreases to 5% to 15% at 1 to 3 years. It is debatable whether coil embolization of patent branches before endograft placement is cost-effective in reducing the number of type II endoleaks. The prevailing sentiment is that it is not, especially that rupture in the setting of a type II endoleak is very infrequent.
Management of type II endoleaks has undergone a significant change over the last decade, as their relatively benign natural history became more obvious. The early aggressive pursuit of interventions has given way to a more conservative approach, with the current recommendation to treat type II endoleaks only when they are associated with aneurysm sac enlargement. Up to two thirds of type II endoleaks can spontaneously resolve by 6 months from diagnosis, and resolution can be expected even several years later. In fact, shrinkage of the AAA sac can occur even in the presence of type II endoleak, and less than 10% of patients usually experience sac enlargement greater than 5 mm, supporting an expectant approach with selective intervention. However, although type II endoleaks usually have a benign course, they can occasionally result in AAA sac growth and rupture.
Diagnosis of type II endoleaks is often made by computed tomography angiography (CTA) with delayed phase imaging, although the exact source can be difficult to ascertain and often is better determined by color-flow duplex imaging. In patients with an enlarging AAA sac, the diagnosis is usually confirmed with angiography after selective injections of the superior mesenteric artery (SMA) and hypogastric arteries.
The approach to type II endoleaks ranges from observation to laparoscopic clipping of branches or surgical conversion. Endovascular approaches, however, are most common and include embolization of the nidus at the aneurysm sac and the feeding vessels. Proximal embolization of branches leading to the leak is ineffective and potentially hazardous, because reconstitution of retroperitoneal pathways to the leak is extremely likely, and colonic ischemia can result from embolization of the IMA if the IMA is not embolized close enough to its origin. Occluding agents include glue ( n -butyl cyanoacrylate), coils, or ethylene vinyl alcohol copolymer (Onyx, ev3 Endovascular, Plymouth, MN). The use of thrombin has been reported, but the risk of ischemic complications resulting from migration of the agent into outflow vessels is significant, with potential cord or visceral injury.
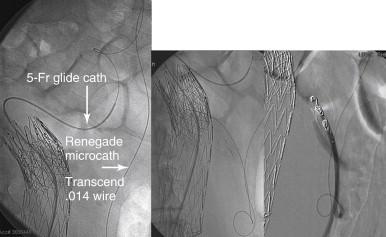
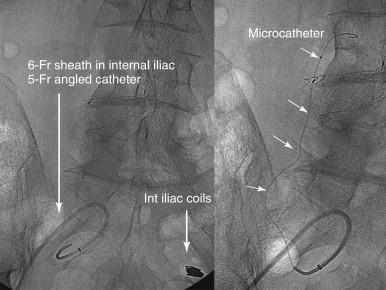
Transarterial catheterization can be more technically demanding but is potentially more effective. A superselective angiogram often demonstrates that the leak is much larger and more complex in terms of inflow and outflow vessels than was suggested on earlier imaging studies ( Figure 2 ). After the anatomy of the leak has been defined, embolization can be performed with coils or liquid agents. A coaxial system with microcatheters ( Figure 3 ) allows the safe delivery of the embolic agent. When coiling is performed, long coils are typically needed, especially for the nidus, and saline flush is preferred to coil pushers to avoid loss of access from an often tortuous and tedious route. On occasion a catheter can be introduced along the perigraft space in the iliac region to access the sac and perform the coiling procedure.
If a transvascular approach is not possible, the leak can be approached directly by direct sac puncture, which is usually performed from a prone left translumbar approach, although the transcaval approach has been described. Coils, glue, or ethylene vinyl alcohol copolymer have been used successfully as long as the nidus and the feeding vessel are directly accessed and embolized.
In a series of patients treated with coil embolization for persistent type II endoleak and an enlarging AAA sac, clinical success was achieved in 79% of patients but sometimes requires more than one intervention in the setting of complex anatomy. Some endoleaks originated from the lumbars and others from the IMA, and some had a combined source. The interventions can be performed with no procedural morbidity or mortality, can successfully obliterate the endoleak, and result in AAA sac stabilization or regression.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here