Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Gender dysphoria, quite often referred to as gender identity disorder, is defined by an individual’s persistent discomfort with his or her own assigned sex. Individuals with gender identity disorder have a desire to live as members of the opposite sex and therefore often modify their primary and secondary sexual characteristics. Today there are many surgical and medical options for transsexual patients to transition into their desired gender.
Transsexual females are persons who were born with male anatomy and assigned to be male sex at birth, but the gender they associate with is female and vice versa for transsexual males. These individuals often undergo hormonal therapy and sex reassignment surgery to transition and alter their appearance in a way that aligns with their gender identity. The term “trans” or transgender female refers to a transexual woman and “trans” male refers to a transexual man; wheras the term “cis” or cisgender are individuals who identify with their assigned gender at birth.
Before any of these procedures or starting hormone therapy, a mental health evaluation is required. A psychiatrist must diagnose the individual with gender identity disorder. This evaluation rules out any endocrine disorders, psychosis, and mental health disorders. Once the patient is cleared by the psychiatrist, hormone replacement therapy is initiated before surgical intervention.
Many transgender male-to-female patients see breast development after long-term hormone replacement therapy. However, for those who desire larger breasts, breast augmentation is an alternative or supplemental option. Breast augmentation is the enlargement of breast by using silicone or saline implants to enhance the size and shape of the chest ( Fig. 25.1 ). The prosthesis is chosen to fit the contour of the breast by the surgeon according to the patient’s desired appearance. In some male-to-female patients, consideration of a tissue expander as a first step to develop a breast mound may be considered. The use of breast implants requires a thorough discussion with the patient and informing the patient that implants are not lifetime devices and thus often require further operations over one’s lifetime.
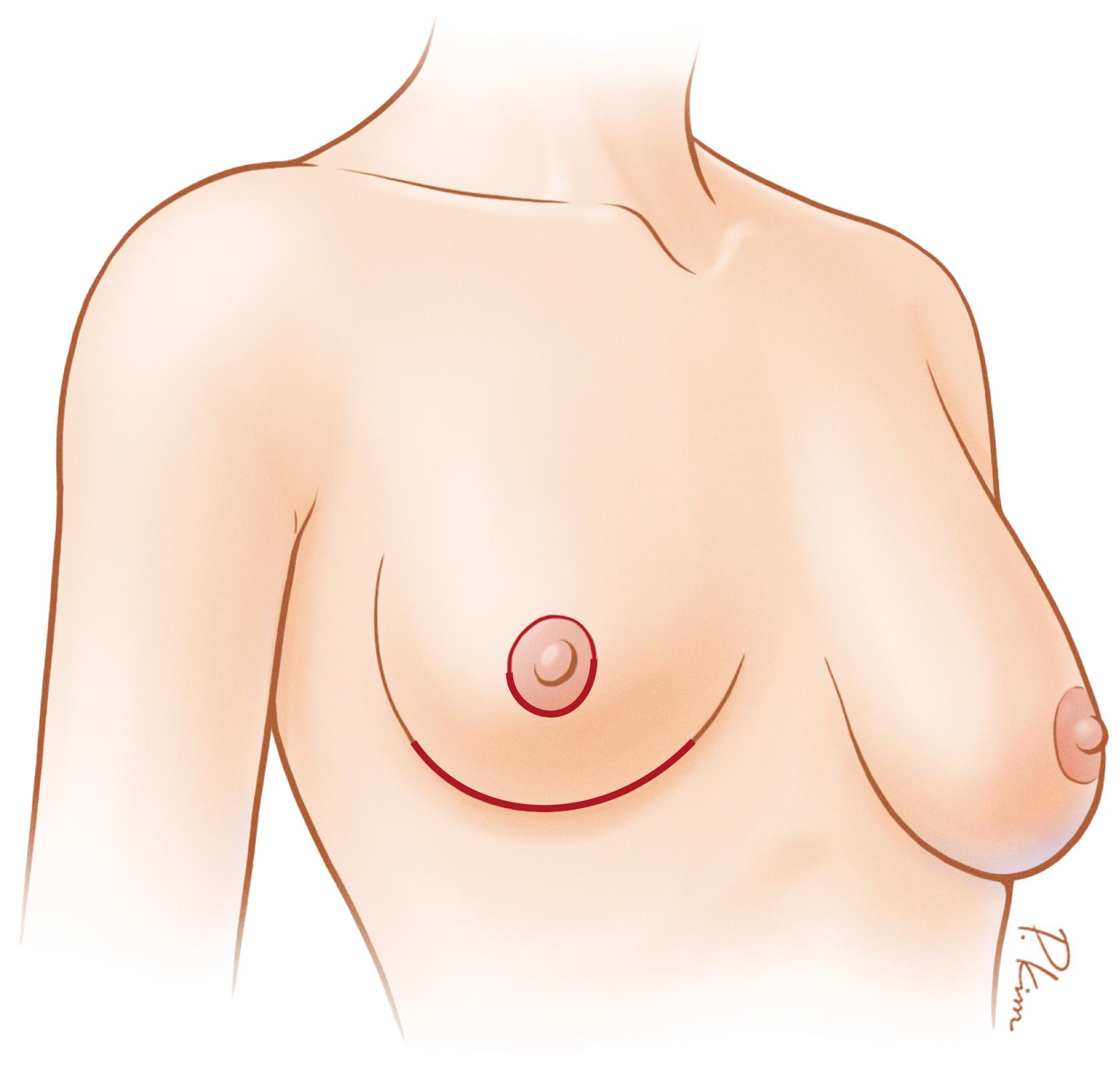
Transgender female-to-male patients usually seek bilateral mastectomy, which is the removal of the breast and the shaping of the male contoured chest. The technique chosen for this procedure depends on the amount of breast tissue present and the tissue elasticity. The breast parenchyma and fat can be removed through multiple incisions ranging from a periareolar incision to a double-incision mastectomy with free nipple graft.
Although hormone therapy is preferred for most gender reassignment procedures, it is not required for top surgery eligibility. Top surgery may be performed 6–12 months before bottom surgery, which includes vaginoplasty or metoidioplasty/phalloplasty; for some trans-individuals, top surgery may be the only surgical procedure throughout transition.
Augmentation mammaplasty for the transgender female patient is a commonly performed procedure. Despite the frequency with which the procedure is performed, there are very few articles that address this specifically in the published literature. For the transgender female patient seeking improvement of her chest appearance, it is incumbent on the treating physician to distinguish these operative indications from those of a cis-female patient seeking aesthetic or even reconstructive measures for breasts. Therefore, the treating physician should be knowledgeable of the World Professional Association for Transgender Health (WPATH) guidelines for top surgery in trans-female patients and should strictly adhere to the parameters outlined. The full extent of these guidelines exceeds the scope of this chapter; however, the surgeon should have a letter from a licensed mental health specialist who has an established relationship with the patient, and the patient should be on hormone therapy and living as the desired gender for at least 12 months. Adherence to these guidelines is important not only to ensure that the patient meets criteria from a gender dysphoric standpoint but also from a medico-legal standpoint for the surgeon.
Once the dysphoria is addressed and/or documented, surgical evaluation can proceed as standard for an augmentation mammaplasty. The indications for a subcutaneous mastectomy in transgender males follow the same guidelines as for trans-females with the exception of being on hormone therapy.
Most patients would have been on a feminizing hormone protocol before evaluation by a plastic surgeon for augmentation mammaplasty. These hormones generally result in some breast tissue growth, which is usually consistent with a Tanner stage 3 or 4 seen in adolescent girls. This development is usually not sufficient for the patient’s aesthetic desires and in our experience not sufficient for the patient to “pass” as the female gender, so it is important for the plastic surgeon to determine what are the patient’s aesthetic goals and expectations. Generally speaking, we have found that most trans-female patients desire a relatively larger appearance than most cis-females. The challenge with this, however, is that their tissue is usually less conducive to large volume (augmentations). We have found that virtual imaging has helped both the treating plastic surgeon and the patient come to a better understanding of the patient’s desired appearance. This also allows for better management of expectations preoperatively. After virtual imaging, we proceed with our routine breast/chest examination as we would for any patient desiring a change in appearance of the breasts, which includes assessing breast footprint (breast width), inframammary fold (IMF) level and symmetry, nipple-to-IMF distance both at rest and on stretch, sternal notch–to-nipple distance, nipple–areolar complex diameter, skin pinch, evaluation of underlying pectoralis muscle, and determination of preexisting ptosis. It is also important to evaluate for any abnormalities such as masses in the breast tissue and axilla, because, although rare, estrogen exposure in these patients can increase their risk for breast malignancy. There is limited literature regarding the risks and incidence of breast cancer in this population.
Depending on the patient’s body mass index, most differences are noted in the relatively less elasticity of the overlying skin envelope, as well as thinner superior pole tissue. The pectoralis major muscle is usually more developed in these patients as well. It is important to identify any asymmetry preoperatively, because it might be more pronounced postoperatively, leading to patient dissatisfaction.
The choice of prosthesis should be guided by patient preference after the risks and benefits of both silicone and saline are explained by the plastic surgeon. It has been our preference to proceed with silicone prostheses because of the softer postoperative texture ( Table 25.1 ). Textured implants have a risk of anaplastic large cell lymphoma (ALCL), so it is our practice to place smooth implants. Recent FDA recommendations are for ultrasound or MRI at 5-6 years postoperatively to look for a silent leak and then every 2-3 years in the asymptomatic patient.
| Saline filled | Silicone Gel | |
|---|---|---|
| FDA approval | Yes, must be >18 years old | Yes, must be >22 years old |
| Filling | Saline water solution | Silicone gel |
| Volume | Volume can be adjusted during surgery | Filled before surgery |
| Surface of shell | Smooth or textured | Smooth or textured |
| Warranty | Manufacturer dependent | Manufacturer dependent |
As mentioned earlier, the breast base width is important. This can be determined by applying pressure directly onto the nipple–areolar complex and determining the circular footprint created subcutaneously from the breast tissue that is present. The width of pectoralis muscle is also important, because some of these patients will undergo subpectoral prosthesis placement. This width is determined by measuring the horizontal distance from parasternal insertion of muscle fibers to the anterior axillary fold.
The underlying neurovascular supply to the breast tissue and nipple–areolar complex also should be taken into consideration. The innervation of the nipple–areolar complex comes from the lateral cutaneous branch of the fourth intercostal nerve. This is important when performing pocket dissection of the lateral-to-lateral pectoralis border. The blood supply to the breast and nipple–areolacomplex has been well documented in the past. Of importance, however, is that the second intercostal perforator from the internal mammary artery is frequently encountered when performing subpectoral pocket creation and can be a source for postoperative hematoma if not adequately controlled intraoperatively. The subpectoral pocket is the safest from a perfusion standpoint because the blood supply from the pectoral branch of the thoracoacromial artery is maintained.
We begin by marking the midline by drawing a line from the sternal notch to the umbilicus. We then mark the native IMFs bilaterally. The native breast footprint is usually demarcated and outlined as described earlier. Depending on the thickness of the pectoralis muscle, we might have the patient adduct the shoulders to delineate the pectoralis border for preoperative markings as well.
Our standard approach is to use an IMF incision, because the preoperative nipple–areolar complex width of trans-females is usually not sufficient to allow periareolar prosthetic insertion. Transaxillary approaches to breast augmentation are well documented in the literature; however, in our experience, we think that better final contour and symmetry are better attained via an IMF approach.
Because of the larger sized implants that most of these patients desire, if an IMF incision is placed directly within the IMF, the problem of postoperative scar migration onto the breast might result. Therefore, we generally place our IMF incision at least 1 cm inferior to the native IMF, depending on the size of the implant being placed.
Determination of the pocket placement is usually done preoperatively. For a very thick pectoralis muscle, a subglandular or subfascial approach might be more desirable, because the risk of postoperative animation deformities is minimized. Dual-plane III placement also can aid with prevention of that problem. Of note, the skin envelope is usually thinner in these patients, which conversely makes subglandular placement more tenuous from a post-operative standpoint. Because of this, it is our practice to perform subpectoral placement, with a dual-plane II release if necessary. We determine the need for dual-plane release depending on the extent of preoperative ptosis present.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here