Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
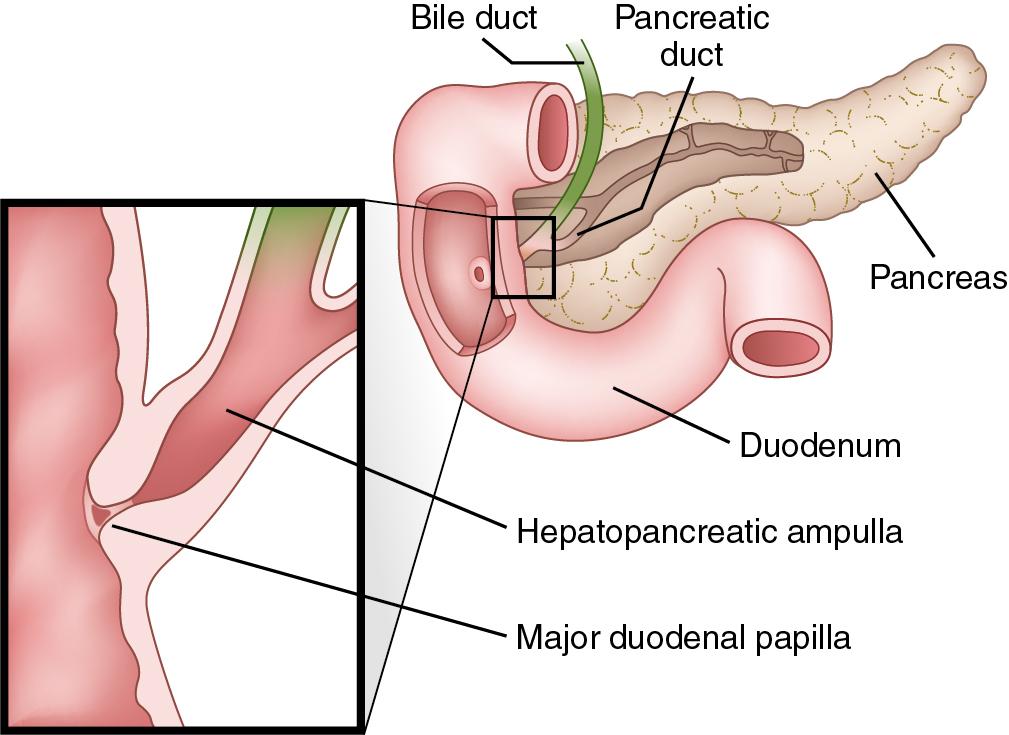
First described by Samuel Collins in 1685 and later by Abraham Vater in 1720, the ampulla of Vater is a papillary structure in the second portion of the duodenum in which the common bile duct and the pancreatic duct converge just before draining into the duodenal lumen ( Fig. 117D.1 ; see Chapter 2 ). The most common benign neoplasms of the ampulla of Vater are villous and tubulovillous adenomas (see Chapter 59 ). Autopsy studies in the 1930s and 1940s identified ampullary adenomas in 0.04% to 0.12% of individuals. , Although they are classified as benign tumors, they are truly premalignant lesions with the potential to transform into adenocarcinomas. In addition, ampullary adenomas harbor occult dysplasia or adenocarcinoma in as many as 60% of cases.
Patients with sporadic adenomas typically present later in life; however, patients with polyposis syndromes, such as familial adenomatous polyposis syndrome and MUTYH-associated polyposis syndrome, present much earlier in life. Approximately 30% to 50% of ampullary neoplasms present with painless jaundice, , , but increased use of screening protocols has identified an increasing number of patients with asymptomatic ampullary neoplasms. Duodenoscopy, endoscopic ultrasound (EUS), and endoscopic retrograde cholangiopancreatography (ERCP) remain the diagnostic modalities of choice but distinguishing between adenoma and adenocarcinoma is extremely unreliable because the false negative rate for ampullary biopsy ranges between 25% to 60%.
It is generally accepted that pancreaticoduodenectomy (PD) is the operation of choice for ampullary adenocarcinoma because of a higher margin negative resection rate and resultant lower recurrence rates, adequate lymph node staging, and the elimination of the need for surveillance endoscopy (see Chapters 62 and 117A ). Survival is better for ampullary adenocarcinoma than for any of the other periampullary adenocarcinomas and is largely dependent on lymph node status; five-year survival ranges from 64% to 80% for patients with node negative disease and 17% to 50% for patients with node positive disease. Rate of lymph node metastases are 6% to 10% in pT1 ampullary adenocarcinomas but approach 50% in pT2 and pT3 tumors. ,
Although PD remains the treatment of choice for ampullary adenocarcinoma, optimal management of benign ampullary neoplasms remains controversial. Complete resection remains the only way to ensure the absence of high-grade dysplasia or occult adenocarcinoma within an ampullary adenoma. Given this, some have argued that PD should be performed in all cases. Higher recurrence rates after local excision are also cited by those in favor of PD. Farnell et al. reported recurrence after transduodenal excision (TDE) of villous adenomas of 32% at 5 years and 43% at 10 years. This is comparable to the 46% recurrence rate after TDE reported by Galandiuk et al. Others have suggested, however, that TDE is an adequate form of treatment because it is associated with reduced operative time, reduced inpatient postoperative stay, and decreased morbidity and mortality rates when compared with PD. , Local recurrences, when benign, can typically be salvaged with re-excision. , ,
Over the past 30 years, endoscopic ampullectomy has had an increasing role not only in the diagnosis of but also in the management of ampullary adenomas (see Chapter 30 ). First reported in the literature in the 1980s, initial experiences with endoscopic ampullectomy reported periprocedural complication rates of approximately 25% and recurrence rates of approximately 25% to 50%. , More recent series have reported a periprocedural complication rate of approximately 20% with recurrence rates ranging from 10% to 30%. , Piecemeal excision is associated with a recurrence rate of 54.3% versus 26.2% for en-bloc resection. Much like recurrences after TDE, recurrences after endoscopic can typically be salvaged with repeat endoscopic resection.
Regardless of the chosen approach, the presence of high-grade dysplasia on pathology after TDE or surgical ampullectomy is associated with invasive adenocarcinoma in the final specimen in 50% to 60% of cases. , Although endoscopic findings such as induration and rigidity of the papilla on probing, ulceration, and a submucosal mass effect are suggestive of underlying malignancy, they are certainly not conclusive. Given this, PD should be considered if high-grade dysplasia or adenocarcinoma is identified.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here