Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
|
|
|
|
|
|
|
|
The anterior approach to the cervical spine is a well-established surgical dissection technique that has been used successfully for the treatment of pathologic conditions of the cervical spine, including traumatic conditions, degenerative abnormalities, deformities, infections, and neoplastic diseases. By virtue of the approach, it provides access to the anterior cervical spinal column and avoids the need for dissecting through the cervical posterior stabilizing elements, including the paraspinal muscles and ligamentum nuchae. However, with this approach, the anterior structures of the neck (e.g., the trachea and esophagus) are at risk for both direct injury (perforation) and indirect injury (traction or compression). This chapter reviews injuries to the tracheoesophageal structure during surgical procedures of the cervical spine.
The anterior cervical approach, championed by Robinson and Smith, uses the interval between the sternocleidomastoid muscle and the neck strap muscles. This approach requires dissection through the deep cervical fascia. The trachea and esophagus are then retracted medially, and the carotid sheath is retracted laterally. The deeper surgical plane poses risks of injuring vital structures, including nerves, blood vessels, and lymphatic vessels, and it risks perforating the trachea and esophagus. For patients who have undergone an anterior cervical approach, one of the most common problems encountered during the postoperative period is dysphagia. Some studies reported that during the postoperative period, these patients presented with dysphagia 47% of the time.
Based on the operative level, nervous structures that can be at risk during anterior cervical dissection are the hypoglossal nerve, the superior laryngeal nerve, and the recurrent laryngeal nerve. Palsy of these nerves can manifest in the following ways: as dysphagia, which is difficulty swallowing; as dysphonia, which is an impairment of sound production as the passive vocal cords interact with the exhaled airstream; and as hoarseness, which is a breathy or harsh voice ( Table 52-1 ).
| Vertebral Level | Structure(s) at Risk | Clinical Correlate |
|---|---|---|
| C2 | HN | Dysphagia, dysarthria, ipsliateral tongue deviation |
| C2–C3 | HN | Dysphagia, dysarthria, ipsliateral tongue deviation |
| C3 | HN, ISLN, STA, SLA | Dysphagia, dysarthria, ipsliateral tongue deviation, impaired cough reflex |
| C3–C4 | ISLN, STA, SLA | Impaired cough reflex |
| C4 | ISLN, ESLN, STA, SLA | Impaired cough reflex, hoarseness, voice fatigability, impaired high-pitch phonation |
| C4–C5 | ESLN, STA, SLA | Hoarseness, voice fatigability, impaired high-pitch phonation |
| C5 | ESLN, STA, SLA | Hoarseness, voice fatigability, impaired high-pitch phonation |
| C5–C6 | ESLN, STA | Hoarseness, voice fatigability, impaired high-pitch phonation |
| C6 | ESLN, STA | Hoarseness, voice fatigability, impaired high-pitch phonation |
At the C1 arch level or in the anterior triangle of the neck, the hypoglossal nerve is at risk as it exits the hypoglossal foramen and passes along the anterior aspect of the C1 arch. Except for the palatoglossus muscle, all motor innervation to the tongue muscles is provided by the hypoglossal nerve; therefore, palsy of the nerve causes ipsilateral tongue deviation with difficulty swallowing as the ability to move the food toward the back of the mouth is impaired.
At the C3-C4 level, the superior laryngeal nerve, along with closely associated structures (e.g., the carotid bifurcation, upper pole of the thyroid, and superior thyroid artery) are at risk. The superior laryngeal nerve is a branch of the vagus nerve (cranial nerve X) that originates in the carotid sheath before it splits into a sensory (internal) branch and a motor (external) branch. The sensory branch innervates both ipsilateral and contralateral larynges, thus preventing aspiration. The motor branch innervates the cricothyroid, a muscle that tenses the vocal cords to produce the high-pitched sounds of singing. Palsy of the motor (external) superior laryngeal nerve branch manifests as a monotonous voice, whereas palsy of the sensory (internal) superior laryngeal nerve may be silent because the pharynx has contralateral innervation. Therefore, patients undergoing revision surgical procedures of the cervical spine should have a preoperative evaluation with electromyography, strobovideolaryngoscopy, or both, to determine the status of the superior laryngeal nerve.
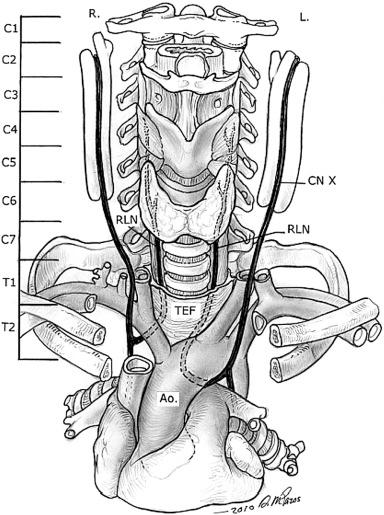
The recurrent laryngeal nerve is vulnerable to traction injury as it loops around the great vessels—the aorta on the left and the subclavian artery on the right—before ascending into the tracheoesophageal groove in the neck ( Fig. 52-1 ). Other postulated causes of recurrent laryngeal nerve injury include direct trauma, pressure neurapraxia from a fixed inflated endotracheal cuff, and stretch from aggressive retractor use; the right recurrent laryngeal nerve is suggested to be more vulnerable than the left because of its more lateral point of fixation on the brachiocephalic trunk.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here