Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
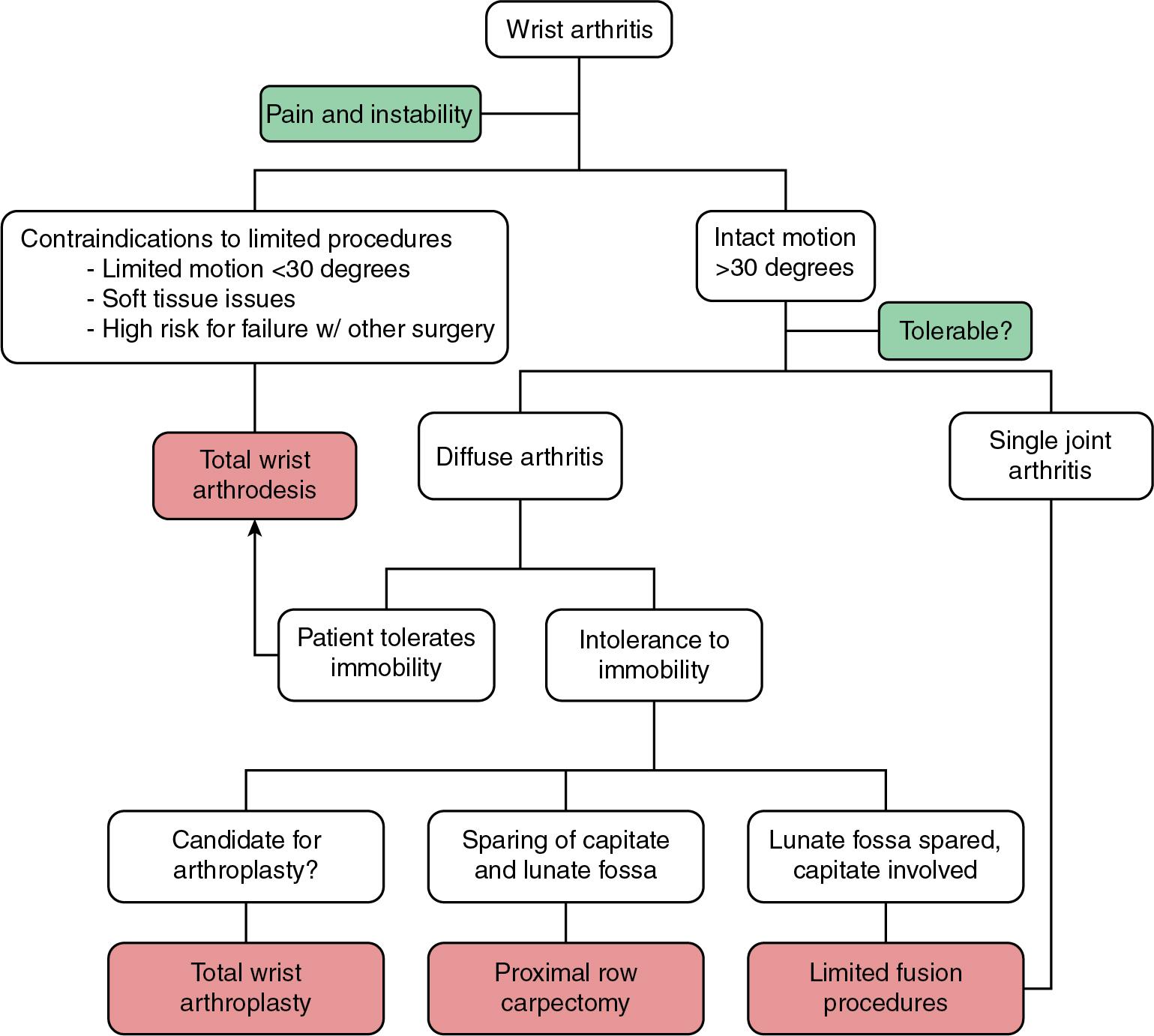
Total wrist fusion is indicated in patients with pain or instability after failure of nonoperative management and motion-preserving procedures.
Wrist fusion is preferred when multiple joints (i.e., the radiocarpal and midcarpal joints) are involved. If disease is isolated to a single joint, motion-preserving procedures, such as a proximal row carpectomy or partial wrist arthrodesis, can be considered ( Fig. 53.1 ).
Total wrist fusion is a treatment option for patients with osteoarthritis (OA), posttraumatic arthritis, inflammatory arthritis, Keinböck disease, scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist, and ligamentous instability. It is a salvage for failed partial fusions or arthroplasty.
Other indications include traumatic segmental bone loss of the distal radius and carpus, reconstruction after segmental tumor resection, and paralysis of the wrist.
Pain relief and stability are prioritized at the expense of wrist motion. A detailed history of the patient’s functional demands, activities, occupation, hobbies, and home circumstances is mandatory. A preoperative trial of splinting to simulate loss of motion can help set patient expectations.
Arthrodesis is contraindicated in patients with active infection or uncontrolled inflammation.
The hand and wrist are examined for previous scars and areas of tenderness, edema, and deformity ( Fig. 53.2 ).

The carpus and distal radioulnar joint (DRUJ) are assessed for subluxation and dislocation, which suggest inherent wrist instability.
Range of motion (ROM) is evaluated and documented for individual joints.
A thorough nerve examination is performed to rule out concomitant carpal tunnel or Guyon canal syndrome, which can occur because of synovitis within the carpal canal or with dislocation of the carpus.
Standard, three-view radiographs of the wrist are mandatory to evaluate the joint surfaces, carpal alignment, and bone quality. SLAC and SNAC patterns are often seen in patients with posttraumatic arthritis and should be noted preoperatively ( Fig. 53.3 ).

Well-controlled rheumatoid patients typically have localized joint erosions with maintained joint spaces. As the disease progresses, radiocarpal arthrosis develops and the carpus translates ulnarly and subluxes volarly. If the midcarpal joint is preserved, radiolunate or radioscapholunate fusion can be considered. Patients with advanced rheumatoid disease have pancarpal arthrosis and significant bone loss. Total wrist fusion is the only predictable surgery for these patients ( Fig. 53.4 ).

Computed tomography (CT) scans provide detailed information on the radiocarpal, midcarpal, and intercarpal joints and are indicated when the extent of arthrosis is unclear on plain films.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here