Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Vagus nerve stimulation (VNS) is a treatment option for a number of disorders. It is most commonly used to treat medically intractable seizures but has also been approved by the United States Food and Drug Administration (FDA) to treat severe depression ( ). It has been suggested (but not approved by the FDA) that VNS may also be used to treat tremor, obesity, and some inflammatory or autoimmune disorders ( ). The potential effectiveness of any of these treatments cannot be fully achieved if the device is not implanted correctly. There have been a few previous reports that describe the technique of implantation ( ). Some of these articles were written soon after the device was approved for general use. This chapter is intended to describe this surgical technique in detail and includes some ideas learned from many years of experience with this technique.
It is important to note the statement from the manufacturer (LivaNova PLC, London, UK) that accompanies the device ( http://us.livanova.cyberonics.com/en/vns-therapy-for-epilepsy/healthcare-professionals/vns-therapy/manuals-page/ ) states that the vagal nerve stimulation therapy system is indicated for use as an adjunctive therapy in reducing the frequency of seizures in adults and adolescents over 12 years of age with partial onset seizures that are refractory to antiepileptic medications. Use of this device is also indicated for the adjunctive long-term treatment of chronic or recurrent depression for patients 18 years of age or older who are experiencing a major depressive episode and have not had an adequate response to four or more adequate antidepressant treatments. It cannot be used in patients after a bilateral or left cervical vagotomy.
The surgeon is mostly concerned about the left vagus nerve because this is the nerve that is most commonly implanted. Stimulation of either vagus nerve has antiseizure effects, but stimulation of the right vagus nerve has a greater likelihood of adverse cardiac effects. Therefore, surgery for implantation of stimulating electrodes on the right is only very rarely performed and is done only when the left vagus nerve is no longer available ( ).
A basic understanding of the anatomy of the neck is important for successful implantation of a vagal nerve stimulator. One should understand not only the routinely encountered structures but also the less commonly encountered structures and anatomic variants of the major structures. It is helpful to discuss these structures in the order that they are encountered during a typical surgical procedure for implantation of vagal nerve stimulator electrodes, but, first, one should begin with a description of the fascial planes of the neck (see Fig. 42.1 ).
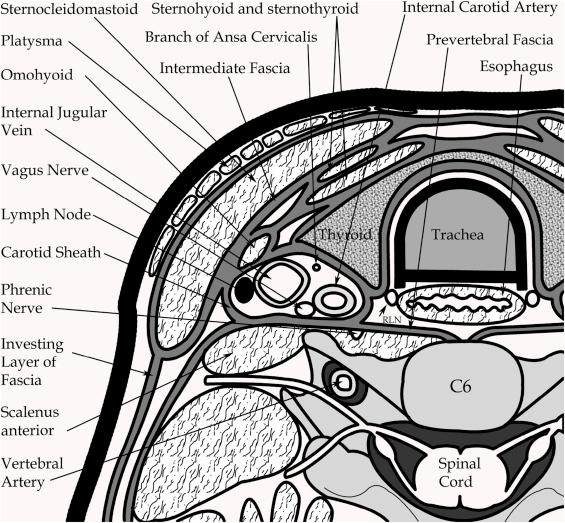
An understanding of the fascial planes in the neck is very important to a successful surgical exposure. The superficial fascia is the subcutaneous tissue containing the platysma and cutaneous nerves of the cervical plexus. This most superficial layer is also called the “investing layer” because it surrounds the sternocleidomastoid and trapezius muscles. This fascia attaches in the midline posterior to the spinous process. The next layer is the intermediate layer, which envelops the sternohyoid and sternothyroid muscles medially and the anterior and posterior bellies of the omohyoid muscle. Also included in this layer is a visceral layer that surrounds the thyroid gland, esophagus, and trachea.
The deepest layer of fascia is the prevertebral fascia. The carotid sheath is a condensation of deep fascia in which are embedded the common and internal carotid arteries, internal jugular vein, and vagus nerve. The carotid sheath blends in front with the pretracheal and investing layers of deep fascia and, behind, with the prevertebral layer of the fascia.
Most of the dissection for a vagal nerve stimulator electrode placement is in the anterior triangle of the neck. The anterior triangle is bounded anteriorly by the midline of the neck, posteriorly by the anterior border of the sternocleidomastoid, and superiorly by the lower margin of the body of the mandible. When one dissects in this area, one first encounters the skin, the subcutaneous fat, the platysma, and the investing layer of fascia. The platysma muscle fibers usually run vertically in the neck and are incomplete toward the midline. Branches of the transverse cutaneous nerve are found in the investing layer of cervical fascia, superficial to the sternocleidomastoid muscle.
The carotid triangle is bounded superiorly by the posterior belly of the digastric, inferiorly by the superior belly of the omohyoid, and posteriorly by the anterior border of the sternocleidomastoid muscle. This triangle is important for surgical access to the carotid sheath. The carotid sheath lies just deep to the inferior corner of the carotid triangle.
Within the carotid sheath lies the common carotid artery, the internal jugular vein, and the vagus nerve. Also within the carotid sheath are the nerves of the ansa cervicalis and the sympathetic plexus.
The internal jugular vein is usually first encountered during a dissection into the carotid sheath at this level. Occasionally, one will find a branch from the jugular vein in this region. This is usually a branch that crosses medially over the carotid artery and is a superior thyroid vein or middle thyroid vein. The common facial vein usually branches from the jugular vein at a more cephalad level, near the thyroid cartilage. The internal jugular vein is bluish and has a much thinner wall than the carotid artery. It is the largest structure in the carotid sheath and enlarges when the patient is in the supine position for surgery.
The common carotid artery is found deep and medial to the jugular vein. The carotid artery bifurcates into the internal carotid artery and external carotid artery, usually at the level of the upper border of the thyroid cartilage. In approximately 70% of cases, the common carotid artery divides into the internal and external carotid arteries at the level of the fourth cervical vertebra (C4). In approximately 20% of cases, the division is at the C3 level, and in 10%, it is at the C5 level ( ). There are usually no branches from the carotid artery inferior to the bifurcation, but a descending branch of the external carotid, the superior thyroid artery is often seen in a dissection of the common carotid. The common carotid artery is white and pulsates easily. It is distinguished by vasa vasorum, which mark the surface of the artery. The artery was also covered with loose areolar tissue. Often, the vagus nerve is adherent to the loose areolar tissue around the artery.
The vagus nerve is the largest nerve in the carotid sheath and at the C5-6 level should be the only nerve without any branches. It is composed of both motor and sensory fibers. It originates in the medulla oblongata and leaves the skull through the middle of the jugular foramen in the company with the 9th and 11th cranial nerves. The vagus nerve possesses two sensory ganglia, a rounded superior ganglion that is situated on the nerve within the jugular foramen and a cylindrical inferior ganglion that lies on the nerve just below the foramen. Below the inferior ganglion, the cranial root of the accessory nerve joins the vagus nerve and is distributed mainly in its pharyngeal and recurrent laryngeal branches.
The vagus nerve passes vertically down the neck within the carotid sheath, lying at first between the internal jugular vein and the internal carotid artery and then between the vein and the common carotid artery. Its position is usually deep between the internal jugular vein and the carotid artery. The vagus nerve is separated from the sympathetic trunk by the prevertebral layer of the cervical fascia.
There are several branches of the vagus nerve that are of surgical importance in the dissection in the neck. The pharyngeal branch arises from the inferior ganglion of the vagus nerve and passes between the internal and external carotid arteries to reach the pharyngeal wall. The superior laryngeal nerve arises from the inferior ganglion and runs downward and medially behind the internal carotid artery. It divides into internal and external laryngeal nerves. There are also two or three cardiac branches arising from the vagus nerve. These branches usually arise from the nerve, superior to the thyroid cartilage. On the left side, the recurrent laryngeal nerve arises from the vagus nerve as the vagus nerve crosses the arch of the aorta in the thorax. This nerve hooks around and beneath the arch behind the ligamentum arteriosum and ascends into the neck in the groove between the trachea and the esophagus. A nonrecurrent laryngeal nerve occurs in approximately 1% of patients on the right but is extremely rare on the left ( ).
The ansa cervicalis is a plexus of nerves that arises from the cervical plexus, formed by the anterior rami of the first four cervical nerves. The ansa cervicalis also lies within the carotid sheath but usually is anterior to the carotid artery and jugular vein. It is important to distinguish this nerve from the vagus nerve so as to avoid placing the stimulating electrodes on the wrong nerve. The ansa cervicalis supplies the sternohyoid muscle, the sternothyroid muscle, the omohyoid muscle, and the sternocleidomastoid muscle.
Deep to the carotid sheath is the prevertebral layer of fascia. This fascia covers not only the vertebral body and the longus coli muscles on the anterior vertebral bodies but also the scalenus anterior muscle. Within the prevertebral fascia and deep to the carotid sheath is the phrenic nerve.
The cervical part of the sympathetic trunk extends upward to the base of the skull and below to the neck of the first rib, where it becomes continuous with the thoracic part of the sympathetic trunk. It lies directly behind the internal and common carotid arteries (i.e., medial to the vagus) and is embedded in deep fascia between the carotid sheath and the prevertebral layer of deep fascia. There is a superior cardiac branch of the sympathetic trunk, which descends in the neck behind the common carotid artery. It ends in the cardiac plexus in the thorax.
At the most inferior end of the anterior neck exposure and deep to the prevertebral fascia is the thoracic duct. In the lowest part of the neck, the thoracic duct passes upward along the left margin of the esophagus. As it reaches the level of the transverse process of the seventh cervical vertebra, it bends laterally behind the carotid sheath and in front of the vertebral vessels. On reaching the medial border of the scalenus anterior, it turns downward in front of the left phrenic nerve and the first part of the subclavian artery.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here