Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Understanding the surface anatomy of the lungs ( Fig. 5.1 ) and their relation to adjacent structures is essential for the practice of respiratory medicine. At the end of tidal expiration, the dome of the diaphragm extends high into the thorax, level with the anterior end of the fifth rib, slightly lower on the left. The lower lateral ribs therefore overlie the liver on the right and the stomach and spleen on the left, with the parietal pleura extending lower than the lungs on the lateral chest wall. Posteriorly, the lungs extend much lower, approaching the 12th rib on full inspiration.
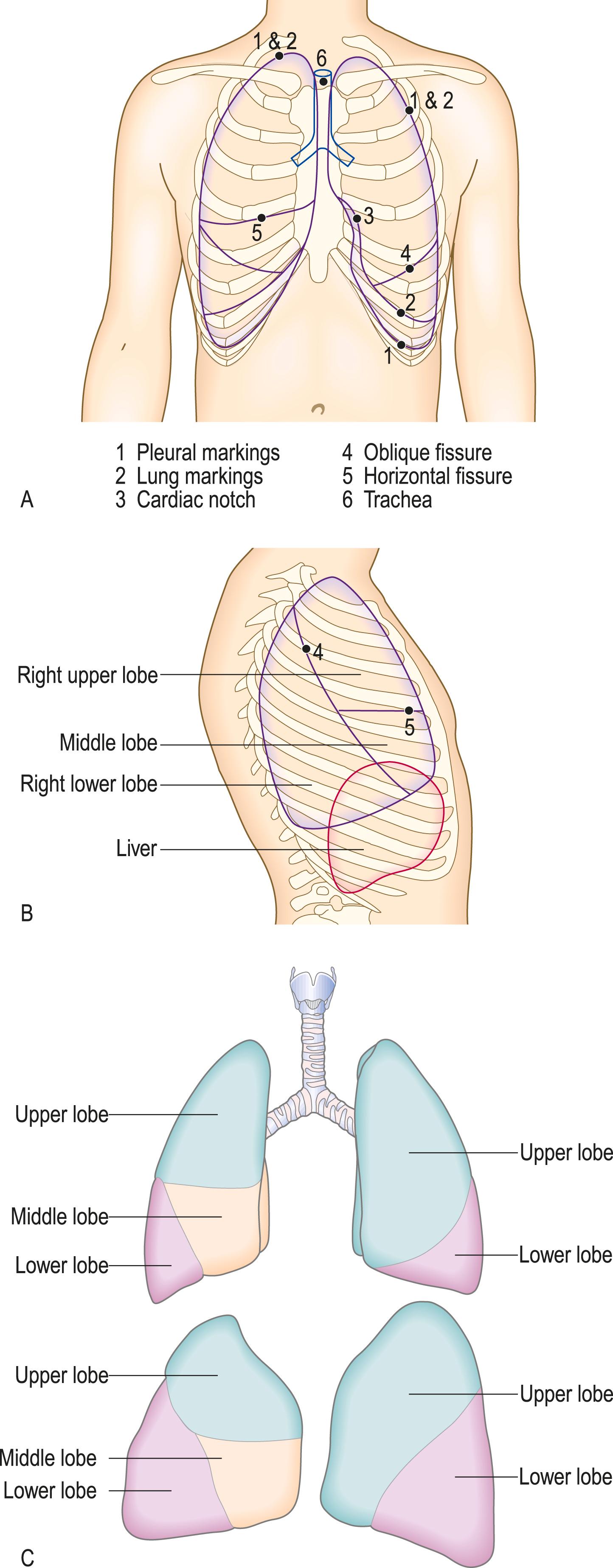
The lung apex lies immediately beneath the brachial plexus, so apical lung tumours commonly disrupt T1 root fibres, causing pain and numbness in the inner aspect of the upper arm and wasting of the small hand muscles. The upper thoracic sympathetic outflow to the eye may also be compromised, leading to a constricted pupil and ptosis. In the mid and lower mediastinum, tumours can invade and compromise the pericardium, atria and oesophagus.
In health, the lungs optimise gas exchange by close matching of regional ventilation and perfusion. Airway and parenchymal lung diseases disrupt this matching, causing hypoxia and cyanosis, and commonly stimulate breathing through lung afferent nerves, leading to a history of breathlessness and tachypnoea upon examination.
The key features of the history are summarised in Box 5.1 .
Breathlessness
Wheeze
Cough
Sputum/haemoptysis
Chest pain
Fever/rigors/night sweats
Weight loss
Sleepiness
Respiratory disease
Other illness/hospital encounters
Drugs causing or relieving respiratory symptoms
Allergies to pollens/pets/dust; anaphylaxis
Family history of respiratory disease
Home circumstances/effect of and on disease
Smoking
Occupational history
Systemic diseases involving the lung
Risk factors for lung disease
Breathlessness (dyspnoea) denotes the feeling of an ‘uncomfortable need to breathe’ and is the most commonly reported respiratory symptom. It is also one of the most challenging to quantify, being inherently subjective. Breathlessness may be caused by respiratory or cardiac disease and also occurs in anaemia or as a manifestation of psychological distress.
Respiratory disease can cause breathlessness through a range of mechanisms:
stimulation of intrapulmonary afferent nerves by interstitial inflammation or thromboembolism
mechanical loading of respiratory muscles by airflow obstruction or reduced lung compliance in fibrosis
hypoxia due to ventilation/perfusion mismatch, stimulating chemoreceptors.
The Medical Research Council (MRC) breathlessness scale ( Box 5.2 ) is a useful and validated way to document formally the patient’s level of dyspnoea.
| Grade | Degree of breathlessness related to activities |
|---|---|
| 1 | Not troubled by breathlessness except on strenuous exercise |
| 2 | Short of breath when hurrying on the level or walking up a slight hill |
| 3 | Walks slower than most people on the level, stops after a mile or so, or stops after 15 minutes walking at own pace |
| 4 | Stops for breath after walking about 100 yds or after a few minutes on level ground |
| 5 | Too breathless to leave the house, or breathless when undressing |
Specific questions may help to distinguish the causes of breathlessness. Ask in particular:
How did the breathlessness start? If the onset was instantaneous, think of pneumothorax, pulmonary embolus or anaphylaxis. Paroxysmal nocturnal dyspnoea (p. 47) may wake a sleeping patient with breathlessness. Onset over hours is typical in asthma, acute pulmonary oedema, lobar pneumonia, or acute hypersensitivity pneumonitis, while an insidious onset is more typical of an evolving pleural effusion, chronic obstructive pulmonary disease (COPD), interstitial lung disease and lung tumours.
How is your breathing at rest and overnight? Asthma commonly wakes patients, while most patients with COPD are comfortable at rest and when asleep but struggle with exertion. Breathlessness provoked by lying down (orthopnoea) is a feature of heart failure (p. 47) but also occurs frequently in patients with severe airflow obstruction or diaphragmatic weakness because the weight of the abdomen displaces the diaphragm cranially on lying down, compromising the vital capacity.
Does your breathlessness vary from day to day or week to week? Variable breathlessness is typical of asthma, whereas patients with COPD or interstitial lung disease usually report consistent daily limitation.
Can you tell me something you do that would make you breathless? and How far can you walk on a good day? These questions reveal the disability caused by respiratory disease. Record restrictions on normal activity or work and the corresponding MRC breathlessness score. Enquiring about hobbies and daily activities reveals the time course of breathlessness; for example, ‘ When was the last time you could walk to the shops / play a full round of golf? ’
When does the breathlessness start? Asthma induced by exercise frequently appears only after exercise during early recovery, because sympathetic drive during exercise defends airway patency.
Certain phrases in the history strongly suggest a psychological aetiology of breathlessness, particularly ‘I feel I can’t get enough air (or oxygen) into my chest.’ In patients with hyperventilation due to anxiety, this symptom is frequently accompanied by a normal measured vital capacity. Associated symptoms induced by hypocapnia in hyperventilation include digital and perioral paraesthesia, light-headedness and chest tightness.
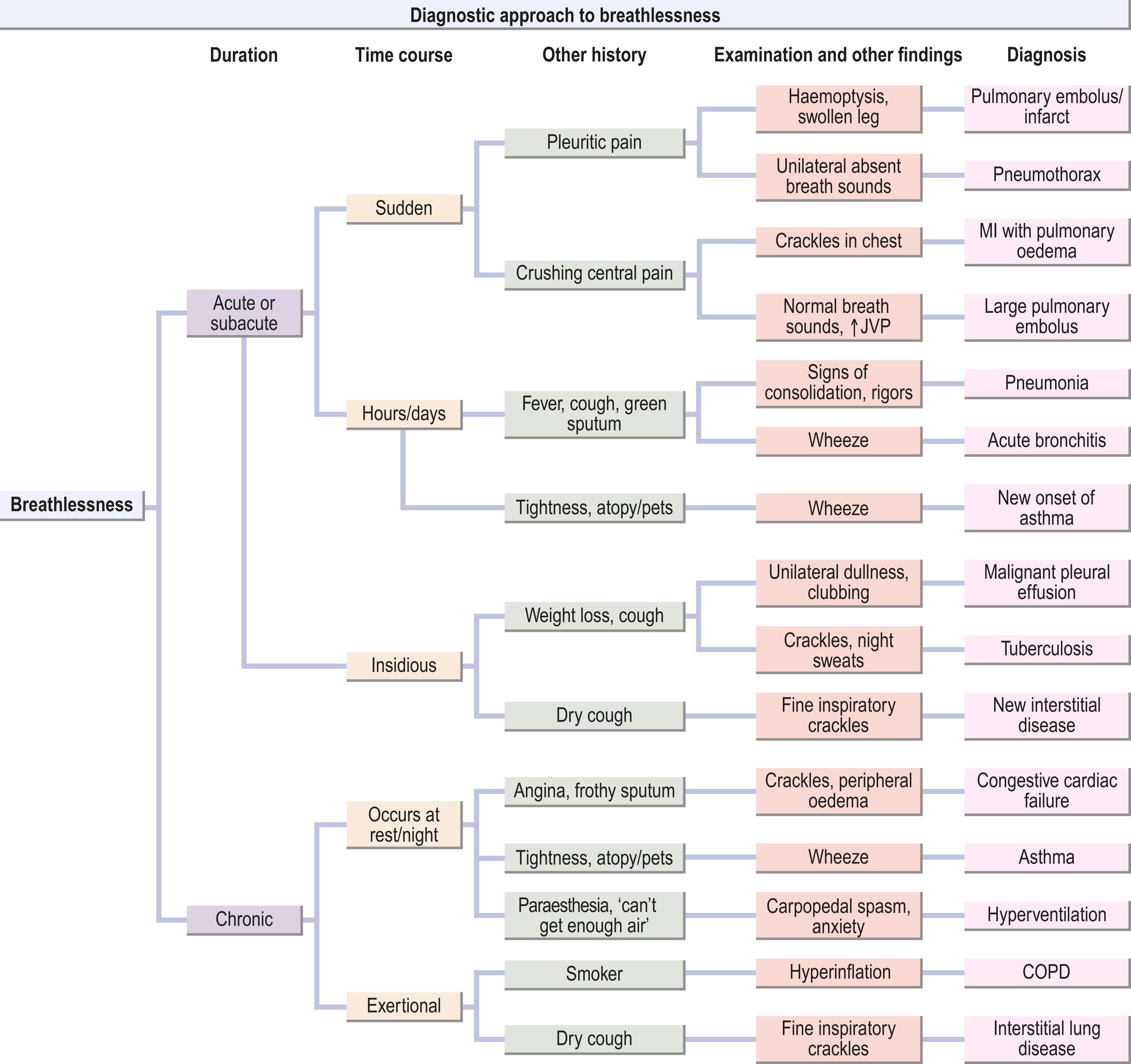
Fig. 5.2 summarises how to use the history and examination findings to distinguish some common causes of breathlessness. Remember that patients do not always report exactly what textbooks describe.
Wheeze describes the high-pitched musical or ‘whistling’ sounds produced by turbulent air flow through small airways narrowed by bronchospasm and/or airway secretions. It is heard mostly during expiration, which additionally narrows the airways. Wheeze must be distinguished from the rattling inspiratory and expiratory sounds caused by loose, mobile secretions in the upper airways, and from the louder, dramatic croak of stridor (see below) caused by obstruction in the trachea or large airways. Patients may be unaware of nocturnal wheeze, which may be noticed only by their bed partner.
Wheeze is most commonly associated with asthma and COPD but can also occur with acute bronchitis, exacerbations of bronchiectasis or congestive cardiac failure (‘cardiac wheeze’).
Ask:
Is the wheeze worse during or after exercise? If it occurs during exercise and limits it, this suggests COPD; in asthma, wheeze and tightness usually appear after exercise.
Do you wake with wheeze during the night? This suggests asthma.
Do you have hay fever or other allergies? Atopy is common in allergic asthma. A family history of wheeze or asthma is common.
Is it worse on waking in the morning and relieved by clearing sputum? This is common in COPD and bronchiectasis.
The cough reflex has evolved to dislodge foreign material and secretions from the central airways and may be triggered by pathology at any level of the bronchial tree. Inspiration is followed by an expiratory effort against a closed glottis. Subsequent sudden opening of the glottis with rapid expiratory flow produces the characteristic sound.
Cough is most commonly a symptom of acute viral bronchitis, which is usually self-limiting over days to weeks. A cough that fails to settle within 3 weeks should prompt consideration of underlying respiratory disease. Causes of chronic cough and features in the history that may indicate the underlying cause are summarised in Box 5.3 .
| Pathophysiology | Suggestive features in history/examination |
|---|---|
| Airways inflammation | |
|
Affects children and some adults Often present at night Associated wheezing, atopy |
|
History of smoking and intermittent sputum |
|
Cough persisting after recent infection |
|
Daily purulent sputum for long periods Pneumonia or whooping cough in childhood Recurrent haemoptysis |
| Lung cancer | Persistent cough, especially in smokers Any haemoptysis Pneumonia that fails to clear in 4–6 weeks |
| Rhinitis with postnasal drip | Chronic sneezing, nasal blockage/discharge |
| Oesophageal reflux | Heartburn or acid reflux after eating, bending or lying Nocturnal and daytime cough |
| Drug effects | Angiotensin-converting enzyme inhibitors |
| Interstitial lung diseases | Persistent dry cough Fine inspiratory crackles at bases |
| Idiopathic cough | Long history with no signs and negative investigations – diagnosis of exclusion |
Ask about:
Duration of the cough.
Whether it is present every day.
If it is intrusive/irresistible or whether the patient coughs deliberately to clear a perceived obstruction (throat clearing).
Whether it produces sputum. If so, how much, and what colour?
Any haemoptysis?
Any triggers (such as swallowing, cold air, during or after exercise, allergens).
Smoking. This increases the likelihood of chronic bronchitis or lung cancer.
Associated clinical features:
Wheeze: may signal cough-variant asthma.
Heartburn or reflux: gastro-oesophageal reflux commonly triggers cough.
Altered voice or swallowing: consider laryngeal causes.
Drug history, especially angiotensin-converting enzyme (ACE) inhibitors.
Cough that produces green or yellow sputum suggests bronchial infection. Large volumes of sputum over long periods suggest bronchiectasis.
In patients with malignancy at the left hilum, damage to the left recurrent laryngeal nerve may paralyse the left vocal cord, making it impossible for the patient to close the glottis and generate a normal explosive cough. The resulting hoarse forced expiration without the initial explosive glottal opening is called a ‘bovine cough.’
In health, the airway lining fluid coating the tracheobronchial tree ascends the mucociliary escalator to the larynx, where it mixes with upper respiratory tract secretions and saliva and is swallowed. In disease, the accumulation of inflammatory cells, mucus and proteinaceous secretions in the airways results in cough with expectoration of sputum. Ask the patient about the colour, volume and consistency of sputum. Direct examination of the sputum is useful to verify the account ( Fig. 5.3 ).
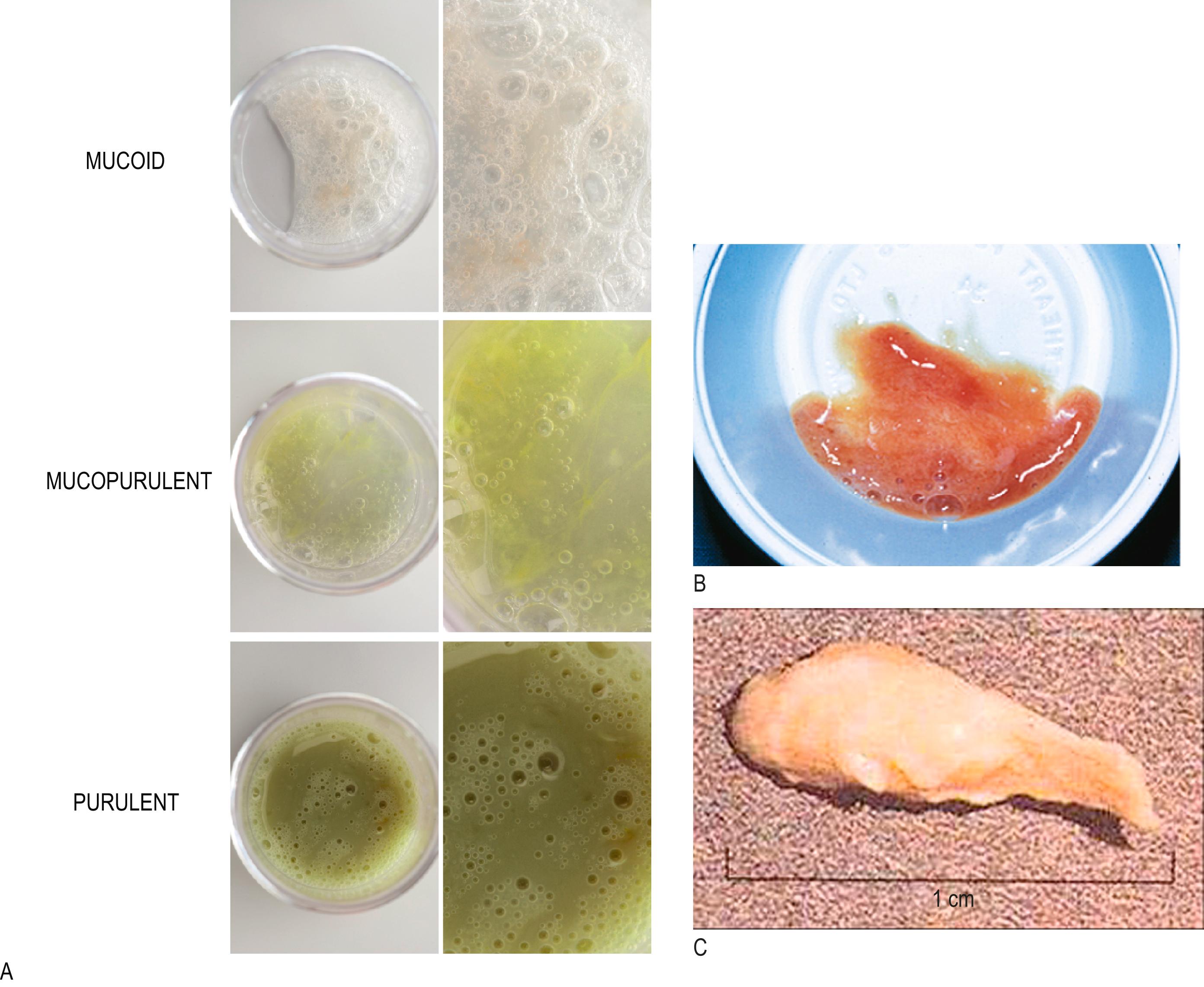
In acute or chronic airway infection, the characteristics of sputum help to clarify the pathology. A change in colour or consistency, or an increase in volume may indicate a new infection in chronic disease.
Clear (mucoid): COPD/bronchiectasis without current infection.
Yellow (mucopurulent): acute lower respiratory tract infection/asthma.
Green (purulent): current infection – acute disease or exacerbation of chronic disease, such as COPD. In bronchiectasis (and COPD), the colour and volume of sputum may be used to guide the need for antibiotics (see Fig. 5.3A ) whereas in asthma, mucopurulent sputum may be the result of sputum eosinophilia.
Red/brown (rusty): pneumococcal pneumonia (see Fig. 5.3B ). Try to distinguish between rusty and frank red blood (see below).
Pink (serous/frothy): acute pulmonary oedema.
Establish the volume produced over 24 hours: small amounts into a tissue or enough to fill a spoon(s), eggcup(s) or cup(s).
Compare the current volume with the patient’s baseline volume.
An increase in stickiness (viscosity) may indicate exacerbation in bronchiectasis.
Occasionally, sputum is produced as firm ‘plugs’ by patients with asthma (see Fig. 5.3C ), sometimes indicating underlying allergic bronchopulmonary aspergillosis.
Large volumes of frothy secretions over weeks/months are a feature of the uncommon bronchoalveolar cell carcinoma.
Haemoptysis means coughing up blood from the respiratory tract. Whilst it can complicate any severe forceful cough, never assume haemoptysis has a benign cause, particularly in a smoker, until underlying pathology has been excluded.
Enquire about these features:
Was the blood coughed up from the chest? Blood in the mouth may be vomited, may have come from the nose in epistaxis, or may appear on chewing or tooth brushing in patients with gum disease.
When did blood appear, how much blood, were there associated symptoms and over what time period was it present?
Any fever/symptoms of infection? Acute or chronic bronchial infections, including tuberculosis, often trigger haemoptysis.
Recurrent blood streaks in clear sputum should prompt a search for lung cancer.
Recurrent blood streaks in purulent sputum over years suggests bronchiectasis.
A sudden episode of haemoptysis with pleuritic pain and breathlessness suggests pulmonary embolism.
Large volumes of haemoptysis (> 20 mL) suggest specific causes:
lung cancer eroding a pulmonary vessel
bronchiectasis (such as in cystic fibrosis)
cavitary disease (e.g., complicating an aspergilloma or cavitary pulmonary tuberculosis).
pulmonary vasculitis
pulmonary arteriovenous malformation.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here