Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Diagnosis and confirmation of pregnancy is one of the common reasons that women come to visit health care providers. At some point in their reproductive years, the vast majority of women will be pregnant and give birth. The percentage of women in the United States who have ever given birth has been increasing. In 2016, 86% of women have given birth over their lifetime compared to 80% in 2006. The average number of children born to each woman in the United States is also increasing, to 2.07 from 1.86 in 2006. In 2011, 45% of pregnancies in the United States were unintended. While this is down from 51% in 2008, this still represents a high rate of unintended pregnancies. Because of this high rate of unplanned pregnancy, many women will not have had any preconception care. Ideally, female patients planning a pregnancy will visit with their primary care doctor or obstetrician/gynecologist prior to conceiving to optimize their health and chance of a good pregnancy outcome. More frequently women will seek medical care after they have already learned that they are pregnant or before they realize they are pregnant.
When interviewing a woman of reproductive age, always consider pregnancy. With any reproductive-aged woman who is sexually active, pregnancy should be always considered. Since up to 25% of women will bleed during their first trimester, pregnancy should be considered in any woman at risk for pregnancy even with a recent menses. “Think pregnancy” should be your motto in the evaluation of reproductive aged patients. This is extremely important because the diagnosis and treatment of a woman's medical or surgical problem may affect the developing fetus if she is pregnant. As discussed later in this chapter, many of the symptoms of pregnancy are nonspecific and can be interpreted erroneously if the pregnancy is not recognized. For example, the urinary frequency that is common in early pregnancy might easily be mistaken for cystitis. The patient might then receive an antibacterial agent such as a sulfonamide or a quinolone, which is not the best choice for the developing fetus. When the urinary symptoms fail to respond to the medication, the patient might then be referred for intravenous pyelography, which subjects the woman to unnecessary tests, contributes to wasteful health care spending, and adds the risk of radiation to an early pregnancy.
When discussing pregnancy and reproductive history, it is important to maintain the patient's privacy. Frequently women will bring their partner or other family member with them to prenatal appointments, but it is important to have time alone with the patient for the history and physical. The gynecologic and social history require privacy and trust between doctor and patient. Topics to be discussed include prior pregnancy histories and outcomes, possible history of sexually transmitted infections, abuse, mental health issues, and ambivalence about being pregnant. Because the history elicited from such a detailed and personal history can uncover complex, unresolved issues, resources for support such as social workers and therapists are crucial to have available.
The anatomy and the physiologic changes related to the menstrual cycle that occur in the nonpregnant woman have already been discussed. This chapter reviews the physiologic alterations resulting from pregnancy and the functional pelvic anatomy.
When semen is deposited in the vagina, sperm travel through the cervix and uterus and into the fallopian tubes, where fertilization may occur if an ovum is present. The majority of sperm deposited in the vagina die within 1 to 2 hours because of the normal acidic environment. The sperm are aided in their travel into the fallopian tubes by uterine and tubal contractions and favorable mucous conditions.
The fertilized ovum, or zygote, remains in the fallopian tube for approximately 3 days. While in the tube, the fertilized ovum divides repeatedly to form a round mass of cells called the morula. If there is an obstruction in the fallopian tube, the fertilized ovum may become trapped in the tube and attach itself to the lining of the tube, giving rise to an ectopic, or tubal, pregnancy. In a normal pregnancy, approximately 6 to 8 days after fertilization, the morula becomes a blastocyst, which migrates through the tube into the uterus, where it attaches itself to the endometrium ( implantation ), with the inner cell mass adjacent to the endometrial surface. Substances that destroy the surface epithelial cells are released, allowing the blastocyst to burrow into the endometrium. The endometrium then grows over the invading blastocyst.
The primitive chorion, the combination of trophoblast and primitive mesoderm, secretes a luteinizing hormone known as human chorionic gonadotropin (hCG), which controls the corpus luteum and inhibits pituitary gonadotropic activity. Quickly thereafter, as the invasion proceeds, maternal venous blood vessels are tapped to form lakes of blood, and chorionic villi develop. These can be identified as early as the 12th day after fertilization. These villi develop a leafy appearance and are called the chorion frondosum. By the 15th day after fertilization, the maternal arterial vessels are tapped, and by the 17th to 18th day, a functioning placental circulation is established. At term, the uteroplacental blood flow is estimated to be approximately 550 to 705 mL/minute. Fig. 23.1A illustrates the path of sperm, fertilization, and implantation.
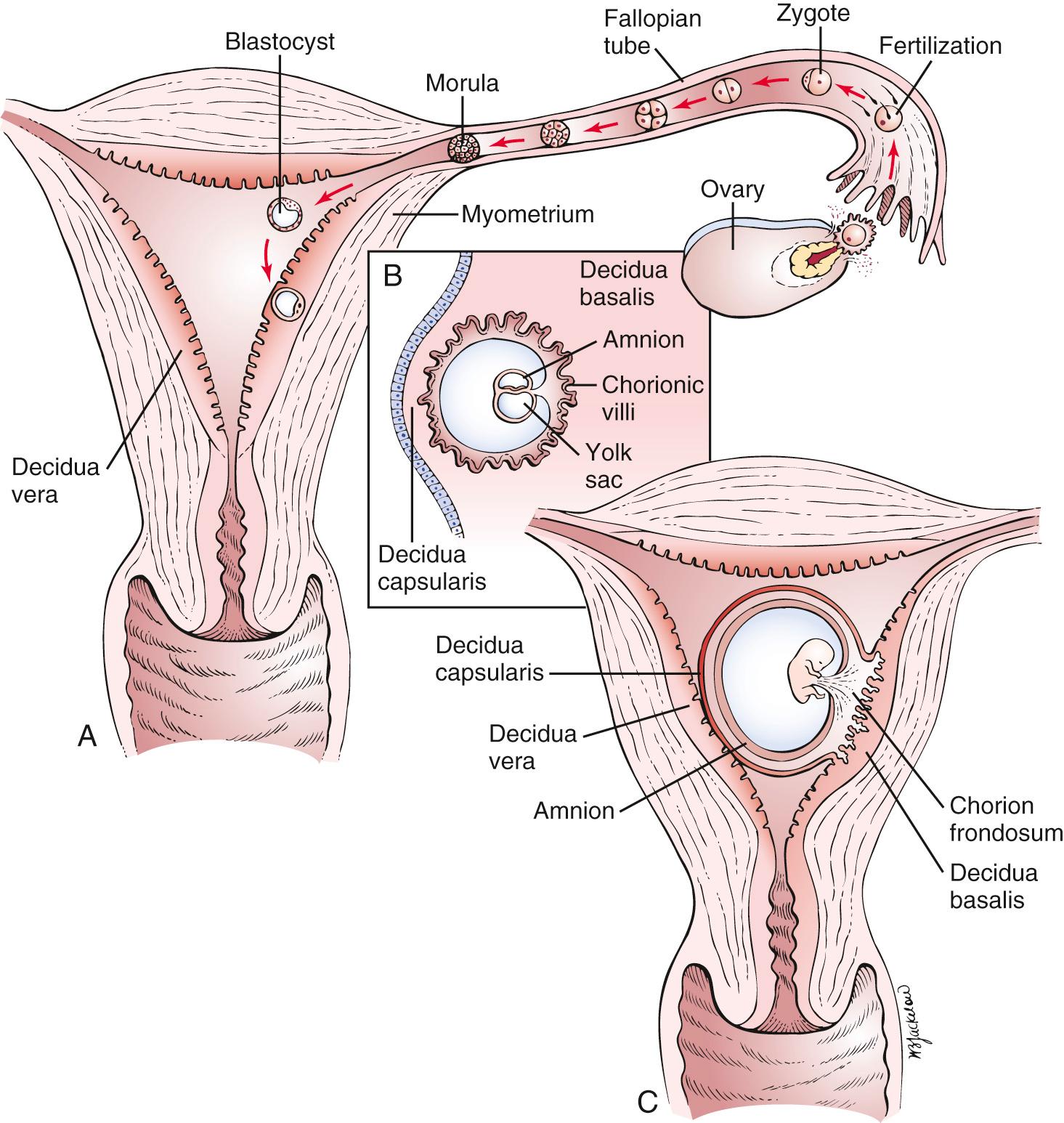
Decidua is the name given to the endometrium of pregnancy. There are three types, distinguished by location with regard to the growing embryo. The decidua capsularis is the overlying endothelium that covers the conceptus, and the decidua basalis is the decidual tissue lying between the blastocyst and the myometrium. The decidua of the remainder of the endometrial cavity is the decidua vera. A cross section through the uterus of a pregnant woman and the different types of decidua in early pregnancy are illustrated in Fig. 23.1B and C .
One of the first placental hormones produced by the developing trophoblastic tissue is hCG . This hormone is present as early as the 8th day after fertilization has taken place. The titers increase to a maximal level by about the 60th to 70th days after fertilization and then decrease. The primary function of hCG is to maintain the corpus luteum during the first 2 months of pregnancy until the placenta can produce enough progesterone by itself. Other hormones, such as human placental lactogen, human chorionic thyrotropin, and adrenocorticotropic hormone, and estrogens are also produced by the placenta. It is beyond the scope of this book to discuss the actions of these hormones; the reader is referred to the references for this chapter for further information.
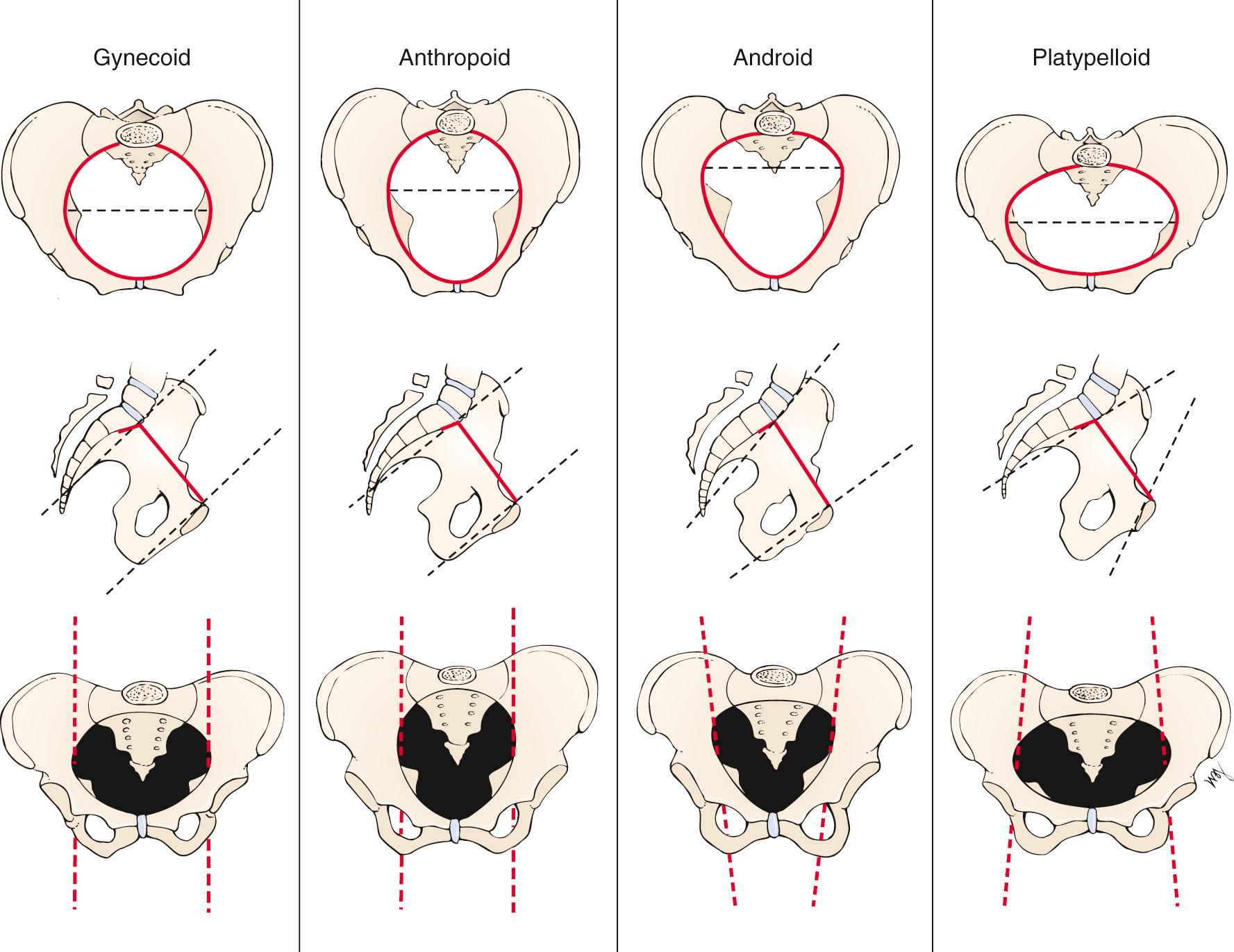
The pelvic cavity is bounded above by the plane of the brim (the inner sacral promontory to the upper and inner borders of the symphysis pubis), below by the plane of the outlet (the lower and inner borders of the symphysis pubis to the end of the sacrum or coccyx), posteriorly by the sacrum, laterally by the sacrosciatic ligaments and ischial bones, and anteriorly by the pubic rami.
The birth canal, through which the infant is delivered, may be thought of as a cylindrical passage with walls composed partially of hard parts (the bony pelvis) and partially of soft parts (the muscles of the pelvic floor and the pelvic ligaments). The cross section of the cylinder is oval, rather than circular, to accommodate the oval cross section of the entering fetal part (e.g., the head) as it descends through the pelvis as a result of the expulsive effect of uterine contractions.
This mechanism for delivery and its corresponding anatomy would be easily understood were it not for the fact that the long axis of the schematic oval, which lies transversely at the entrance to the pelvis, comes to lie in the anteroposterior axis in the midpelvis. The entering fetal part must therefore descend in a spiral path as it progresses through the birth canal.
The process of birth varies greatly, depending on the relationships—lie, presentation, attitude, and position—of the fetus to the maternal anatomy. It is important to define these relationships accurately to understand the birth process.
The term lie refers to the relation of the long axis of the fetus to that of the mother. In more than 99% of full-term pregnancies, the lie is in the same plane as or parallel to the long axis of the mother; this is called a longitudinal lie. In rare instances, the long axis of the fetus is perpendicular to the maternal pelvis; this is called a transverse lie.
The term presentation refers to the part of the fetus in the lower pole of the uterus overlying the pelvic brim (e.g., cephalic or vertex, breech, shoulder) that can be felt through the cervix. The fetus is in the cephalic or vertex presentation (head first) in approximately 95% of all labors. In most cases, the occipital fontanelle is the presenting part.
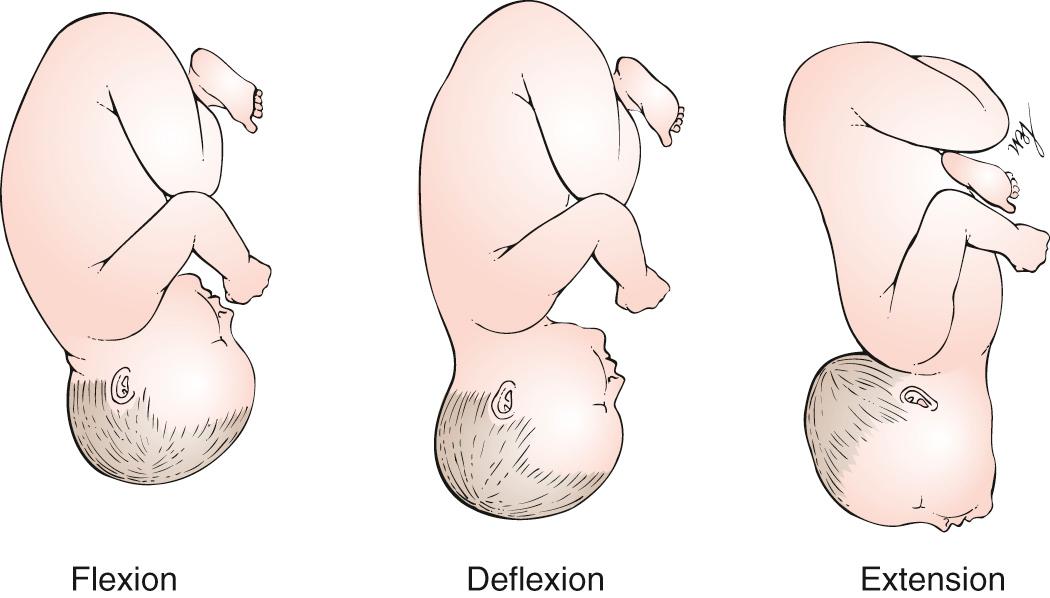
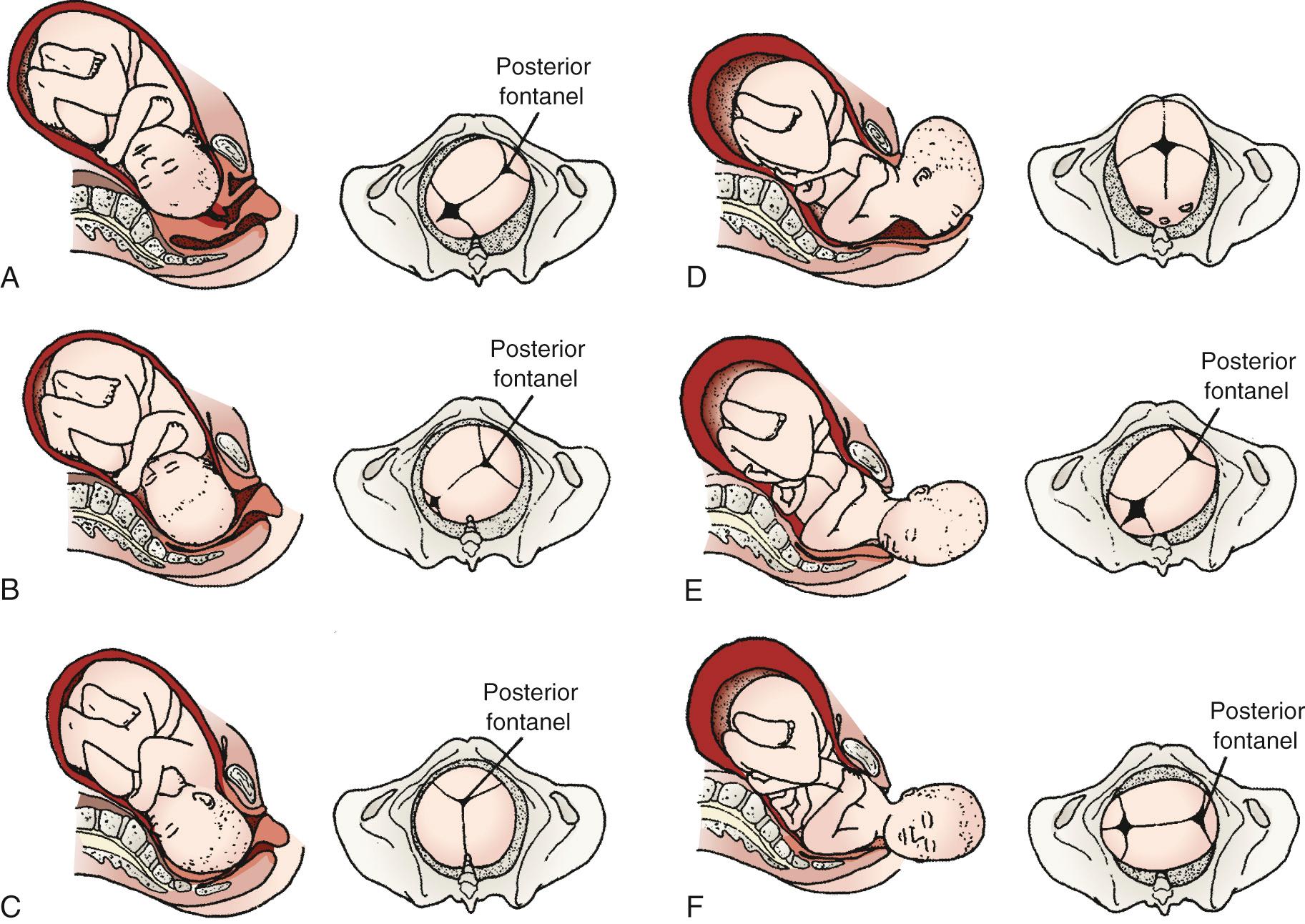
The attitude of the fetus is the posture of the fetus: flexion, deflexion, or extension. Fig. 23.2 illustrates these postures. In most cases, the fetus becomes bent over so that the back is convex, the head is sharply flexed on the chest, the thighs are flexed over the abdomen, and the legs are bent at the knees. This is the description of the fetal attitude of flexion.
The position is the relationship of an arbitrarily chosen portion of the presenting part of the fetus to the maternal pelvis. For example, in a vertex presentation, the chosen portion is the fetal occiput; in a breech presentation, it is the sacrum; and in a face presentation, it is the chin, termed the mentum. The maternal pelvis is divided into eight parts for the purpose of further defining position. These divisions are shown in Fig. 23.3 .
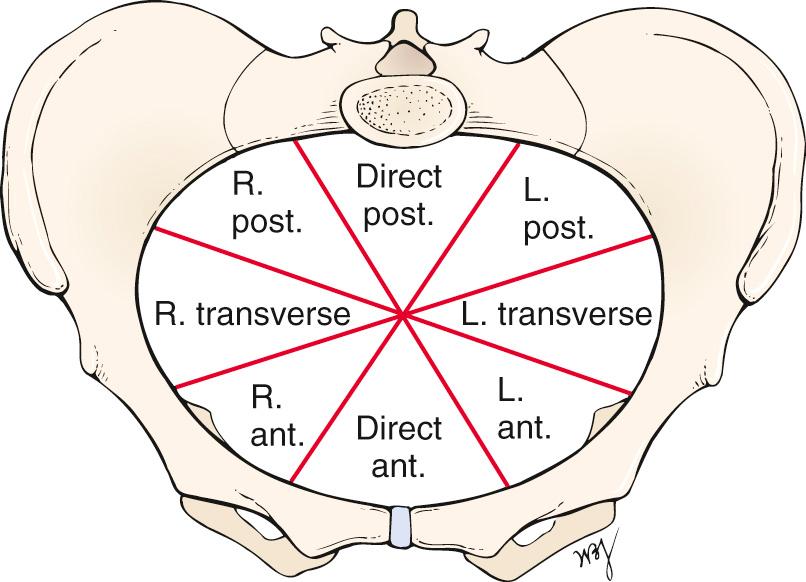
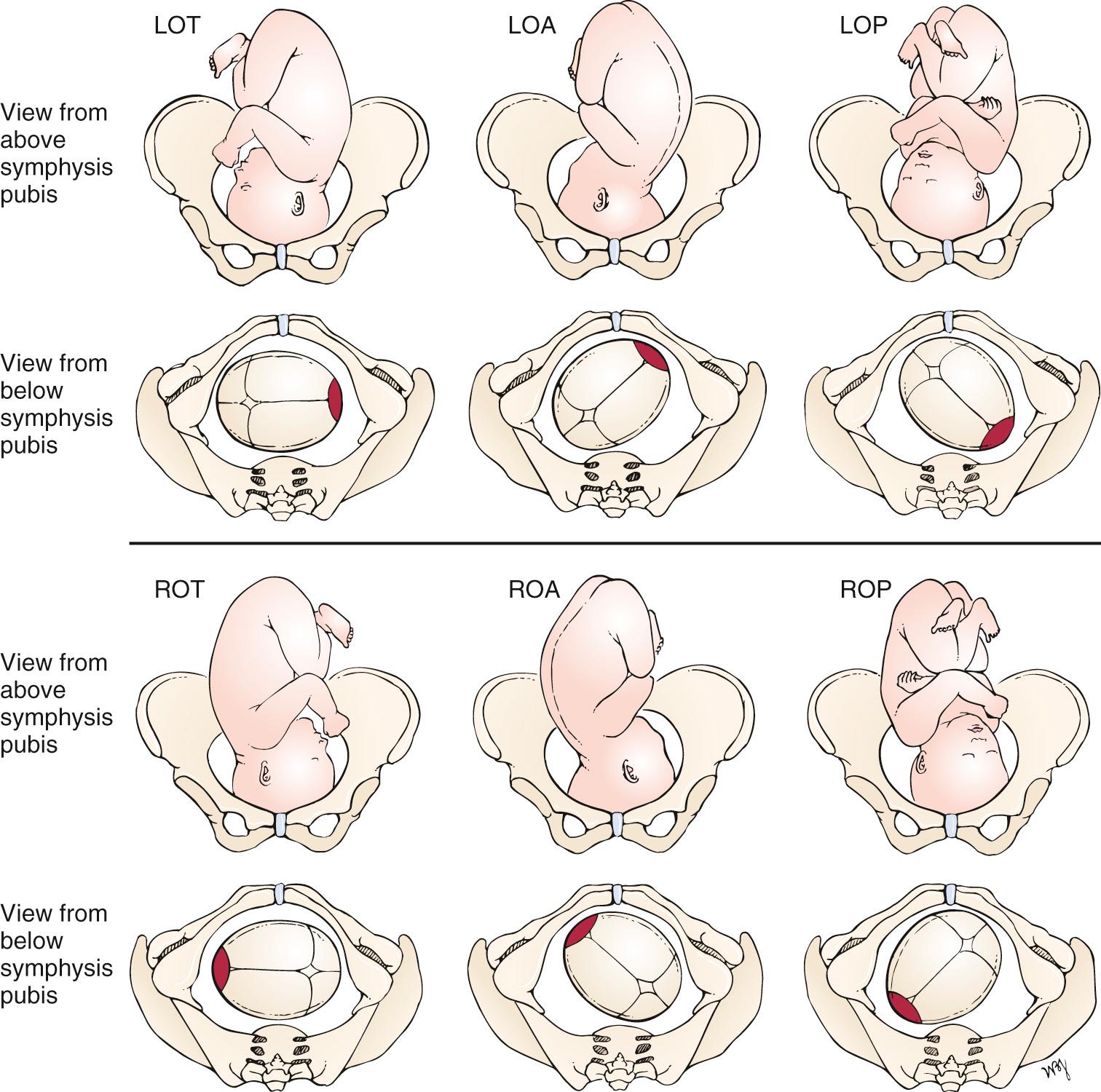
Because the arbitrarily chosen portion of the presenting part may be either left or right, the portion can be described as left occiput (LO), right occiput (RO), left sacral (LS), right sacral (RS), left mental (LM), or right mental (RM). This part is also directed anteriorly (A), posteriorly (P), or transversely (T). For each of the three presentations (vertex, breech, and face), there are therefore six varieties of position. For example, in a vertex presentation, if the occiput is in the left anterior segment of the maternal pelvis, the position is described as left occiput anterior (LOA), which is the most common of all vertex presentations. The common clinical vertex positions are illustrated in Fig. 23.4 . Left and right always denote the side of the mother. Likewise, anterior, posterior, and transverse refer to the mother's pelvis.
The term station characterizes the level of descent of the presenting part of the fetus; “0 station” signifies that the fetal occiput has reached the level of the maternal ischial spines and that the widest transverse part of the infant's head ( biparietal diameter ) is at the level of the pelvic brim. This is also known as engagement . If the vertex is at “−1 station,” it means that the fetal occiput is at a plane 1 cm above the level of the maternal ischial spines (and that the biparietal diameter is therefore 1 cm above the pelvic brim), and the infant's head is therefore not engaged.
The cardinal movements of labor are engagement, descent, flexion, internal rotation, extension, external rotation, and expulsion. These cardinal movements are illustrated in Fig. 23.5 .
There are four basic pelvic configurations: gynecoid, anthropoid, android, and platypelloid. These are based on the shape of the brim, midpelvis, and outlet. Any pelvis is likely to combine features of more than one configuration. Fig. 23.6 illustrates these basic types and summarizes the differences in pelvic anatomy.
The most common symptoms of pregnancy are the following:
Amenorrhea
Nausea
Breast changes
Heartburn
Backache
Abdominal enlargement
Quickening
Skin changes
Changes in urination
Vaginal discharge
Fatigue
Amenorrhea, or absence of menses, results from the high levels of estrogen, progesterone, and hCG, which increase and alter ( decidualize ) the uterine endometrium and do not allow the endometrium to slough as in menstrual bleeding.
Nausea, with or without vomiting, is the so-called morning sickness of pregnancy. As the name implies, the symptom is usually worse during the early part of the day and usually passes in a few hours, although it may last longer. More than 50% of pregnant women in their first trimester have gastrointestinal symptoms. Although the cause is unknown, high levels of estrogen and hCG have been implicated in its development. Pregnant women are also hypersensitive to odors, and they may experience alterations in taste. Morning sickness usually improves after 12 to 16 weeks, when the hCG levels fall. Severe vomiting may occur, resulting in dehydration and ketosis, but this is uncommon, occurring in fewer than 2% of pregnancies.
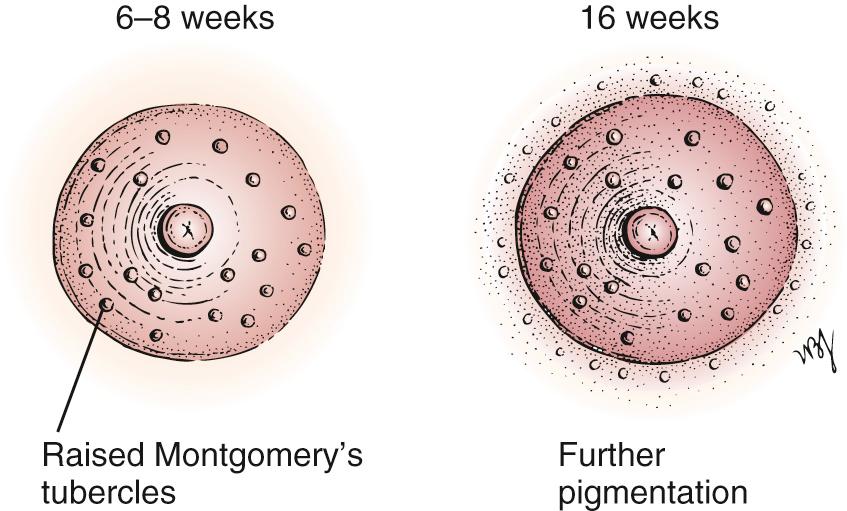
Several changes in the breast occur with pregnancy. One of the earliest symptoms is an increase in the vascularity of the breast, associated with a sensation of heaviness, almost pain. This occurs at approximately the 6th week. By the 8th week, the nipple and areola have become more pigmented, and the nipple becomes more erectile. The Montgomery tubercles become prominent as raised pinkish-red nodules on the areola. By the 16th week, a clear fluid called colostrum is secreted and may be expressed from the nipple. By the 20th week, further pigmentation and mottling of the areola have developed. Fig. 23.7 illustrates the changes in the nipple and areola.
Heartburn in pregnancy occurs because progesterone causes relaxation of the gastroesophageal sphincter. Another cause of heartburn in the third trimester is the upward pressure of the enlarged uterus. This upward displacement exerts pressure on the stomach. There is also a decrease in gastric motility, as well as a decrease in gastric acid secretion, which delays digestion.
As a result of secretion of estrogen and progesterone, the pelvic joints relax, and the increased uterine weight accentuates lordosis. The abdominal muscles stretch and lose tone.
The uterus rises out of the pelvis and into the abdomen by the 12th week of gestation, and an increase in abdominal girth is usually apparent by the 15th week. This enlargement is usually more apparent earlier in multiparous women, whose abdominal muscles have lost some of their tone during previous pregnancies.
Quickening is the sensation of fetal movement. It is a faint sensation initially. Quickening usually begins at approximately 20 weeks in the first pregnancy but is usually felt 2 to 3 weeks earlier in the multiparous woman.
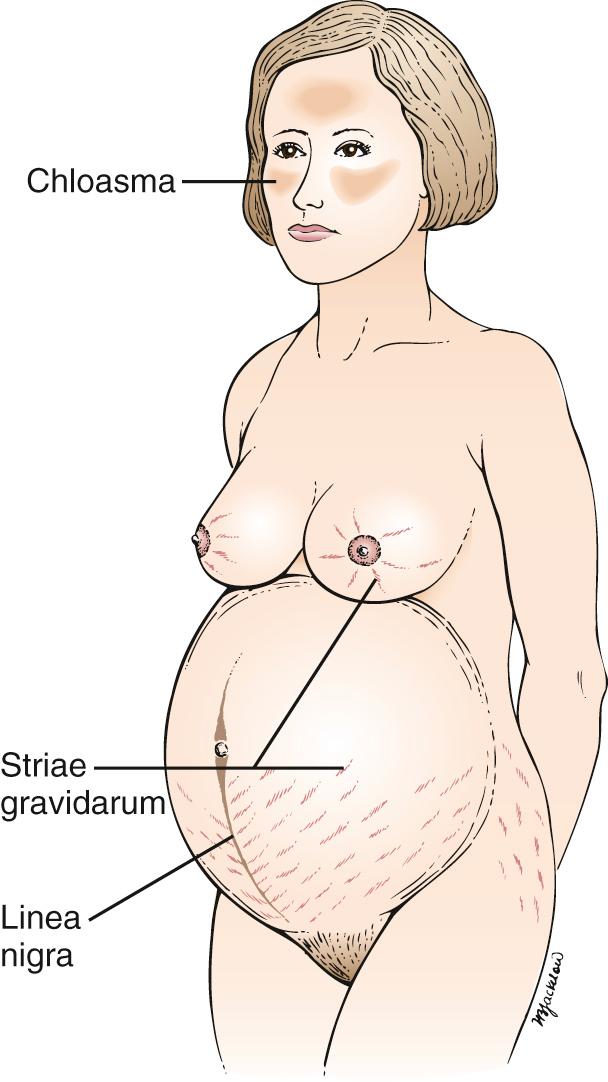
In addition to the skin changes of the breast already discussed, hyperpigmentation is common, especially in women with dark hair and a dark complexion. The linea alba darkens to become the linea nigra, as shown in Fig. 23.8A . Areas prone to friction (e.g., medial thighs, axilla) also tend to darken. New pigmentation on the face, called chloasma, also commonly develops on the cheeks, forehead, nose, and chin. These skin changes are caused by the presence of high levels of ovarian, placental, and pituitary hormones. A woman with chloasma appears in Fig. 23.8B .

“Stretch marks,” or striae gravidarum, are irregular, linear, pinkish-purple lesions that develop on the abdomen, breasts, upper arms, buttocks, and thighs. They are caused by tears in the connective tissue below the stratum corneum. Figs. 23.9 and 23.10 show striae gravidarum of the abdomen and breasts, respectively. The linea nigra is present also on the patient in Fig. 23.8A . Fig. 23.11 illustrates the common skin changes seen in pregnancy.


Transverse grooving, as well as increased brittleness or softening, of the nails may occur. Eccrine sweating progressively increases throughout pregnancy, whereas apocrine gland activity decreases. Hirsutism, caused by increased androgen secretion, may also occur on the face, arms, legs, and back.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here