Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
By the 2nd century CE, Galen had already described the cerebral ventricles, 7 of the 12 cranial nerves, and the cerebral convolutions. There was, however, little further interest in the anatomy and physiologic characteristics of the neurologic system until the 16th century. In 1543, Andreas Vesalius illustrated the basal ganglia, and in 1552, Bartolomeo Eustachius described the cerebellar peduncles and the pons.
In the 17th century, Thomas Willis published descriptions and illustrations of the cerebral circulation, the “striate body,” and the internal capsule. Caspar Bartholin and others thought that the function of the cerebral cortex was to protect the blood vessels, whereas other investigators believed that the cerebrum possessed higher functions. François Pourfour du Petit stressed that the cortex was responsible for motor activity. This concept lay dormant until the end of the 19th century.
Careful anatomic descriptions of the tracts, nuclei, and gyri were contained in the writings of scientists of the 18th and early 19th centuries. Johann Christian Reil and Karl Friedrich Burdach provided names for the many gross anatomic structures that had been illustrated by others in previous centuries. Reil has been credited with the naming of the insula, capsule, uncinate and cingulate fasciculi, and tapetum. The uncus, lenticular nucleus, pulvinar, and gyrus cinguli were named by Burdach. During this same period, Samuel von Soemmering, Felix Vicq d'Azyr, Franz Josef Gall, Louis Gratiolet, and Luigi Rolando made many detailed illustrations of the cerebral convolutional patterns.
In the early 19th century, the first descriptions of several disease states were published. In 1817, James Parkinson wrote an essay describing the “shaking palsy” that now bears his name. In 1829, Charles Bell wrote:
The next instance was in a man wounded by the horn of an ox. The point entered under the angle of the jaw and came out before the ear. … He remains now a singular proof of the effects of the loss of function in the muscles of the face by this nerve being divided. The forehead of the corresponding side is without motion, the eyelids remain open, the nostril has no motion in breathing, and the mouth is drawn to the opposite side.
This is the classic description of facial nerve (seventh cranial nerve) palsy, also known as Bell palsy.
In the mid-19th century, an interest in microscopic neuroanatomy developed. Jan Purkinje, Theodor Schwann, and Hermann von Helmholtz were a few of the many neuroanatomists who contributed valuable information about the intricacies of the nervous system. However, not until the late 19th century were specific staining techniques developed by Camillo Golgi, Vittorio Marchi, and Franz Nissl, which led to the current understanding of neuronal disease. The nerve cell had finally been discovered.
The 20th century was a period of further progress in the description of the cerebral cortex, anterior commissure, thalamus, and hypothalamus. A major advance came from the work of Santiago Ramón y Cajal in 1904. His histologic exploration clarified the complexities of the neuron. Not until 1925 were the hypophyseal-hypothalamic connections described, and even today, the function of the hypothalamus is not fully understood.
It has been suggested that more than 40% of patients who present to internists have symptoms referable to neurologic disease. The internist must be able to identify the early signs and symptoms of neurologic disease and initiate the appropriate therapy. All too often, subtle signs and symptoms may be ignored, and a diagnosis is not made until advanced disability is apparent.
Cerebrovascular disease is one of the most devastating diseases of our time. It remains the fifth leading cause of death in the United States. More than 795,000 Americans suffer a stroke yearly, and it is the number-one cause of disability; more than 3 million Americans currently live with permanent brain damage caused by such an event. On average, someone in the United States suffers a stroke every 40 seconds, and every 4 minutes, someone dies of one. The number of noninstitutionalized adults who have ever had a stroke is 6.2 million people. The debilitating consequences of stroke and the economic effect on society are enormous. The estimated direct and indirect costs of stroke care in the United States are $34 billion. 1
1 Benjamin EJ, Blaha MJ, Chiuve SE, et al. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation . 2017:135:e229.
It is the leading cause of serious long-term disability.
The generalist or internist holds an important position because a patient with a neurologic problem usually seeks help from that physician first. A thorough knowledge of basic neuroanatomy and physiology is the cornerstone of neurologic diagnosis.
The brain, which is enclosed in the cranium and surrounded by the meninges, is the center of the nervous system. The brain can be divided into paired cerebral hemispheres, basal ganglia, diencephalon (thalamus and hypothalamus), brain stem, and cerebellum.
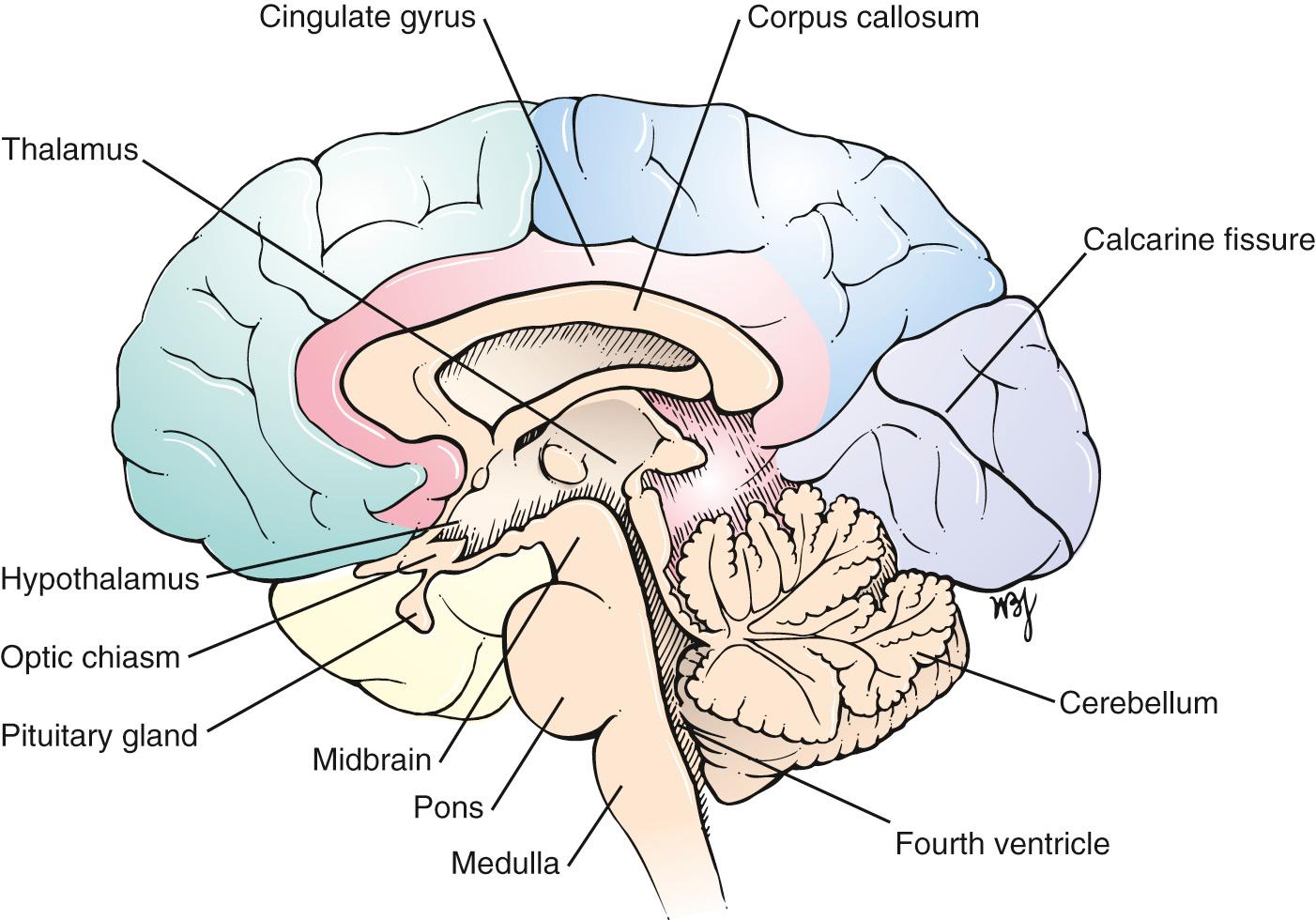
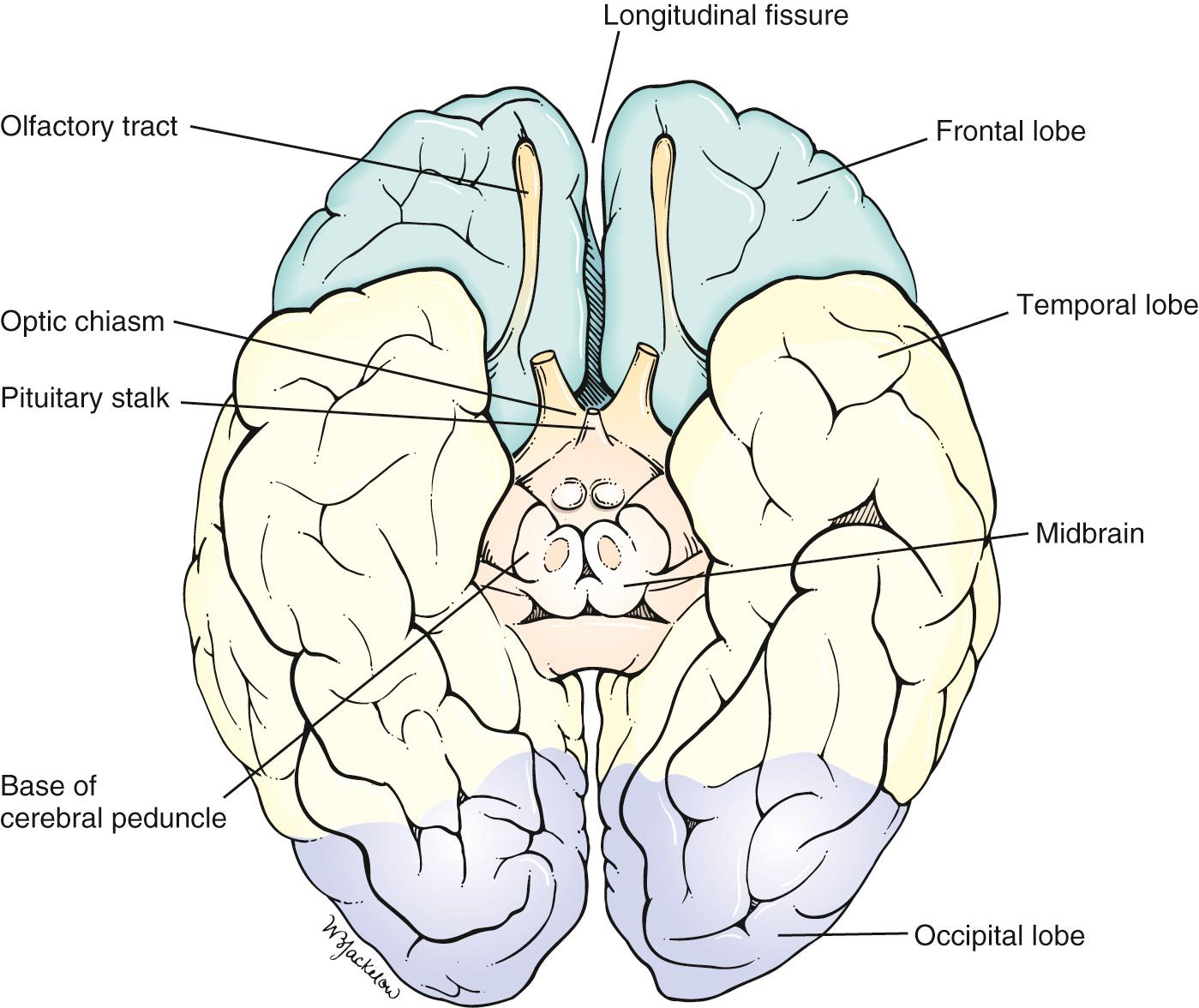
The two cerebral hemispheres make up the largest portion of the brain. Each hemisphere can be subdivided into four major lobes named for the cranial bones that overlie them: frontal, parietal, occipital, and temporal. The fissures and sulci divide the cerebral surface. A deep midline, longitudinal fissure separates the two hemispheres. The convolutions, or gyri, lie between the sulci. A lateral view of the left cerebral hemisphere is pictured in Fig. 21.1 . Fig. 21.2 is a medial view of the right cerebral hemisphere. A basal view of the cerebral hemispheres is pictured in Fig. 21.3 .
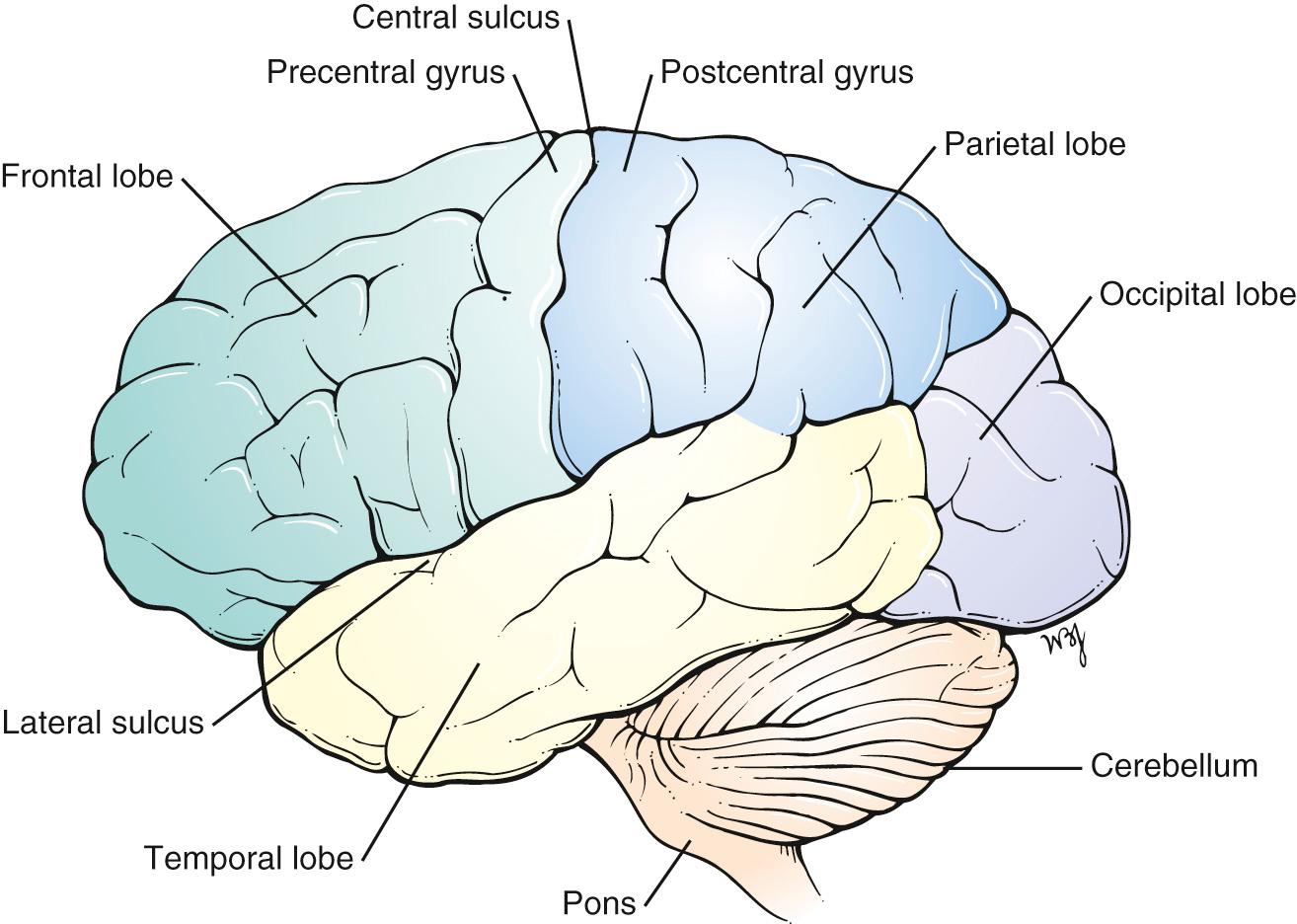
The cerebrum is responsible for motor, sensory, associative, and higher mental functions. The primary motor cortex is in the precentral gyrus. Neurons in this area control voluntary movements of the skeletal muscles on the opposite side of the body. An irritative lesion in this area may cause seizures or changes in consciousness. Destructive lesions in this area can produce contralateral flaccid paresis or paralysis.
The primary sensory cortex is in the postcentral gyrus. Irritative lesions in this area may produce paresthesias (“numbness” or a “pins-and-needles” sensation) on the opposite side. Destructive lesions produce an impairment in cutaneous sensation on the opposite side.
The primary visual cortex is located in the occipital lobe along the calcarine fissure, which divides the cuneus from the lingual gyri. Irritative lesions in this area produce visual symptoms such as flashes of light or rainbows. Destructive lesions cause homonymous hemianopsia on the contralateral side. Central macular vision is spared.
The primary auditory cortex is located in the temporal lobe along the transverse temporal gyrus. Irritative lesions in this area produce a buzzing or ringing in the ears. Destructive lesions almost never produce deafness.
The basal ganglia are situated deep within the cerebral hemispheres. The structures constituting the basal ganglia include the caudate and lenticular nuclei, as well as the amygdala. The amygdala is part of the limbic system and is concerned with emotion. All other components are important structures in the extrapyramidal system, which is concerned with modulating voluntary body movements, postural changes, and autonomic integration. The basal ganglia are especially involved with fine movements of the extremities. Disturbances of the basal ganglia can result in tremors and rigid movements.
The thalamus is a large nuclear mass located on each side of the third ventricle. The thalamus is the chief sensory and motor integrating mechanism of the neuraxis. All sensory impulses, except olfactory ones, and the major output from systems that modulate and modify motor function (i.e., the cerebellum and corpus striatum) terminate in the thalamus, from which they are projected to specific areas of the cerebral cortex. The thalamus is involved in certain emotional connotations that accompany most sensory experiences. Through its connections with the hypothalamus and striatum, the thalamus can influence visceral and somatic effectors serving primarily affective reactions. Through its control of the electrical excitability of the cerebral cortex, the thalamus plays a dominant role in the maintenance and regulation of the state of consciousness, alertness, and attention. The thalamus may be the critical structure for pain perception and thermal sense, which remain after complete destruction of the primary sensory cortex. Thermal sense endows sensation with discriminative faculties and is not concerned with the recognition of crude sensory modalities.
The hypothalamus is located below the thalamus. It includes the optic chiasm and the neurohypophysis. The hypothalamus is responsible for many regulatory mechanisms, such as temperature regulation; neuroendocrine control of catecholamines, thyroid-stimulating hormone, adrenocorticotropic hormone, follicle-stimulating and luteinizing hormones, prolactin, and growth hormones; thirst; appetite; water balance; and sexual behavior.
The brain stem consists of the midbrain, pons, and medulla. Fig. 21.4 shows the external anatomy of the brain stem. The brain stem is responsible for relaying all messages between the upper and lower levels of the central nervous system. Cranial nerves III to XII also arise from the brain stem. The brain stem contains the reticular formation, a network that provides for constant muscle stimulation to counteract the force of gravity. In addition to its antigravity effects, this area of the brain is essential for the control of consciousness. The neurons in the reticular activating system can wake and arouse the entire brain.
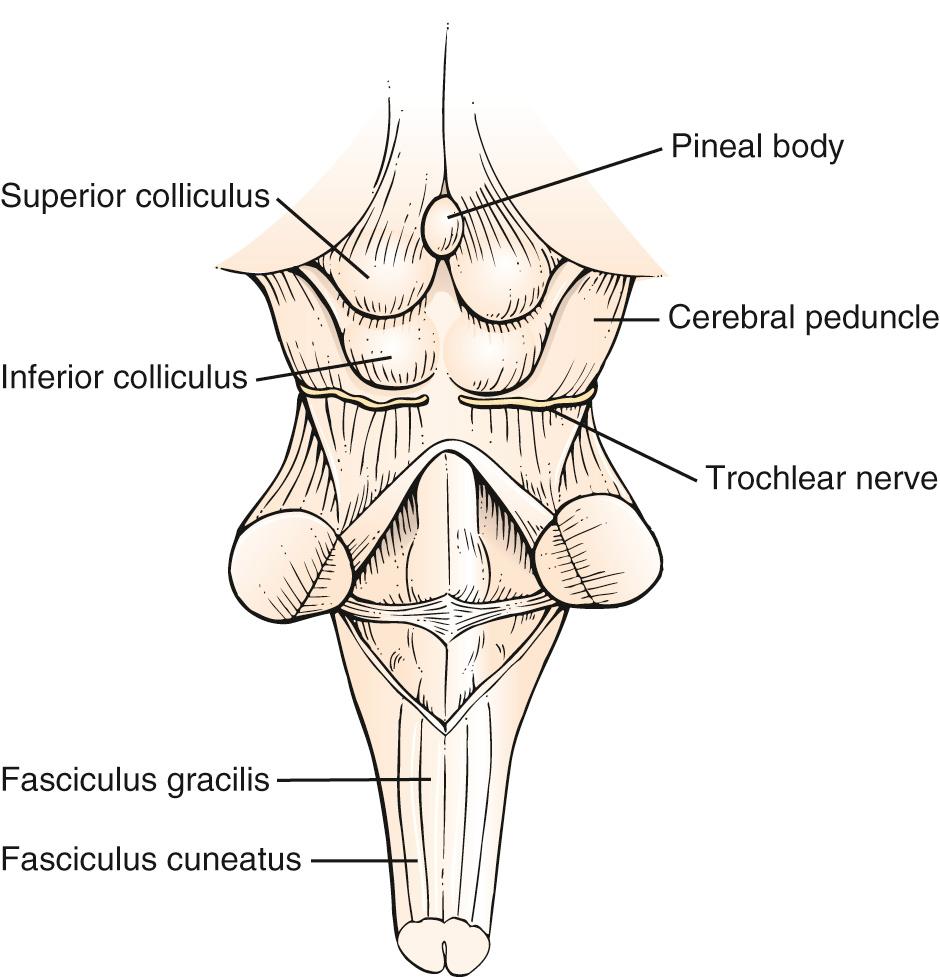
The midbrain contains the superior and inferior colliculi, the cerebral peduncles, and the motor nuclei of the trochlear (cranial nerve IV) and oculomotor (cranial nerve III) nerves. The superior colliculi are associated with the visual system, and the inferior colliculi are associated with the auditory system. The cerebral peduncles converge from the inferior aspect of the cerebral hemispheres and enter the pons. A destructive lesion of the superior colliculi causes paralysis of upward gaze. Destructive lesions of the cranial nerve nuclei produce paralysis of the affected nerve. A destructive lesion of the cerebral peduncle gives rise to spastic paralysis on the other side of the body. Destruction of other tracts in the midbrain results in rigidity and involuntary movements.
The pons lies ventral to the cerebellum and rostral to the medulla. The abducens, facial, and acoustic (and vestibular) nuclei are found in the pons, and their nerves exit through a groove that divides the pons from the medulla. The motor and sensory nuclei of the trigeminal nerve are also located in the pons. At this level, the corticospinal tracts (also known as the pyramidal tracts) have not yet crossed, and a lesion at this level produces loss of voluntary movement on the opposite side. Destructive lesions of the pons may produce a variety of clinical syndromes, such as the following:
Contralateral hemiplegia with ipsilateral trigeminal hemiplegia (paralysis of the jaw muscles and loss of sensation over the same side of the face)
Contralateral hemiplegia with ipsilateral facial palsy (Bell palsy)
Contralateral hemiplegia with ipsilateral facial palsy and ipsilateral abducens palsy (paralysis of the lateral rectus muscle on the same side of the face)
Contralateral hemiplegia with ipsilateral abducens palsy
Quadriplegia and nystagmus
The medulla is the portion of the brain stem between the pons and the spinal cord. The nuclei of the hypoglossal, vagus, glossopharyngeal, and spinal accessory nerves are in the medulla. It is within the medulla that most of the fibers in the corticospinal tracts cross to the opposite side. Destructive lesions in the medulla produce symptoms that are referable to the tracts interrupted by the lesion. Some clinical syndromes are as follows:
Contralateral hemiplegia with ipsilateral hypoglossal palsy 2
2 Paralysis of the tongue muscles on the same side as the lesion. The tongue deviates to the side of the lesion when the patient is asked to stick out the tongue.
Ipsilateral vagal palsy 3
3 Paralysis of the soft palate and difficulty speaking, termed dysarthria.
with contralateral loss of pain and temperature sense
Ipsilateral vagal palsy with ipsilateral spinal accessory palsy 4
4 Paralysis of the sternocleidomastoid or trapezius muscle, or both. This results in the inability to turn the head to the side opposite the lesion and to shrug the shoulder. There are many more clinical syndromes that are beyond the scope of this text. The reader is advised to review the neuroanatomy further to understand the complexities of these neurologic syndromes.
Ipsilateral vagal palsy with ipsilateral hypoglossal palsy
Ipsilateral vagal palsy, ipsilateral spinal accessory palsy, and ipsilateral hypoglossal palsy
The cerebellum is located in the posterior fossa of the skull and is composed of a small midline vermis and two large lateral hemispheres. The cerebellum acts to keep the individual oriented in space and to halt or check motions. The cerebellum is also responsible for the fine movements of the hands. Essentially, the cerebellum coordinates and refines the action of muscle groups to produce steady and precise movements. Destructive lesions of the cerebellum cause swaying, staggering, intention tremors, 5
5 Tremors that result when the individual moves the hands to do something but that may not be present at rest.
and inability to change movements rapidly.
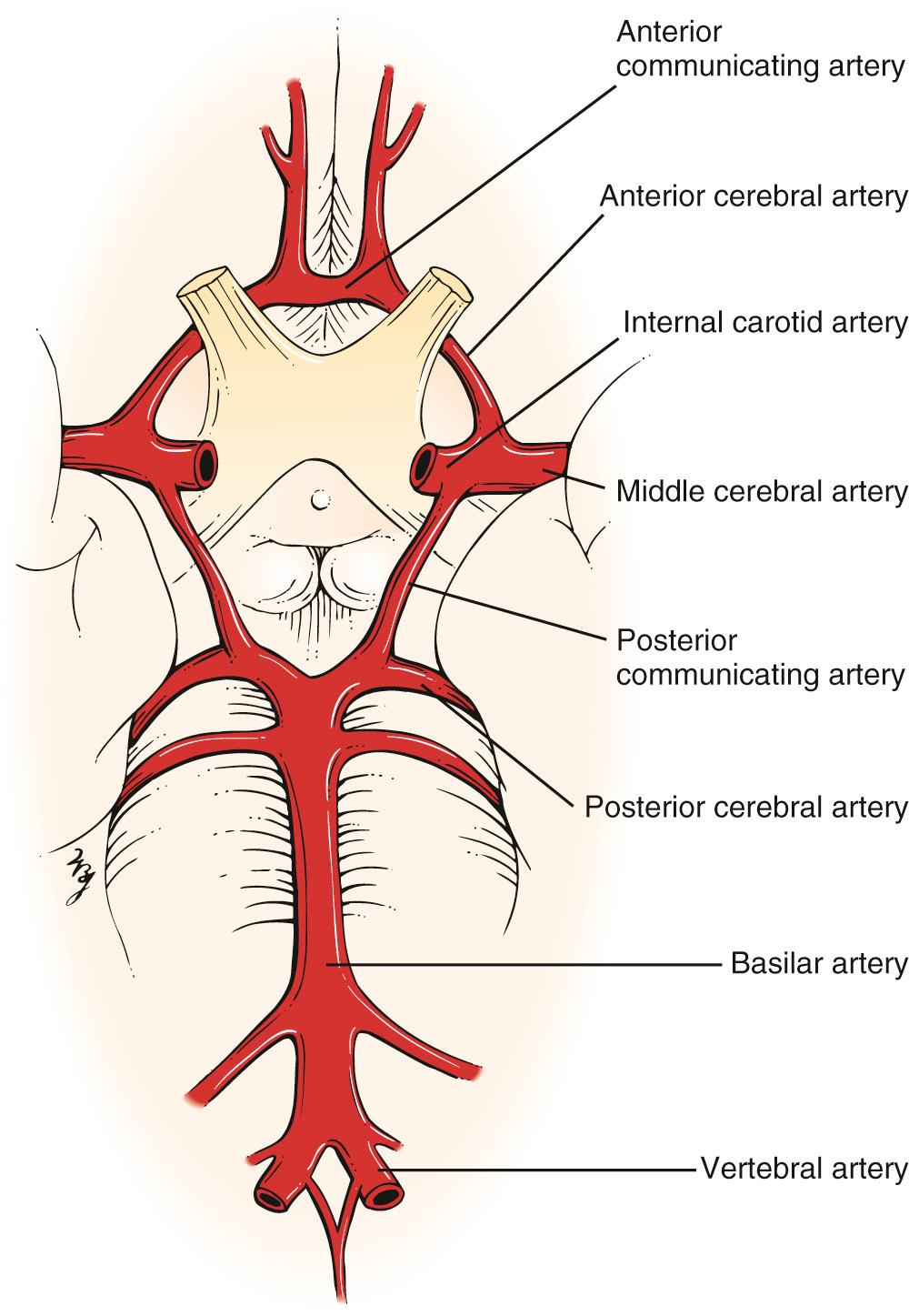
Of the blood supply to the brain, 80% is through the internal carotid arteries and 20% is through the vertebral basilar arteries. Each internal carotid artery terminates at the anterior cerebral and middle cerebral arteries. The posterior cerebral artery arises from the basilar artery, which joins with the posterior communicating artery, a branch of the internal carotid artery. The two anterior cerebral arteries are joined by the anterior communicating artery. This vascular network forms the circle of Willis, located at the base of the brain. This is illustrated in Fig. 21.5 .
Continuous with the medulla is the spinal cord, a cylindric mass of neuronal tissue measuring 40 to 50 cm in length in adults. Its distal end attaches to the first segment of the coccyx. The spinal cord is divided into two symmetric halves by the anterior median fissure and the posterior median sulcus. Each half contains white and gray matter, which can be further subdivided. This is illustrated in Fig. 21.6 .
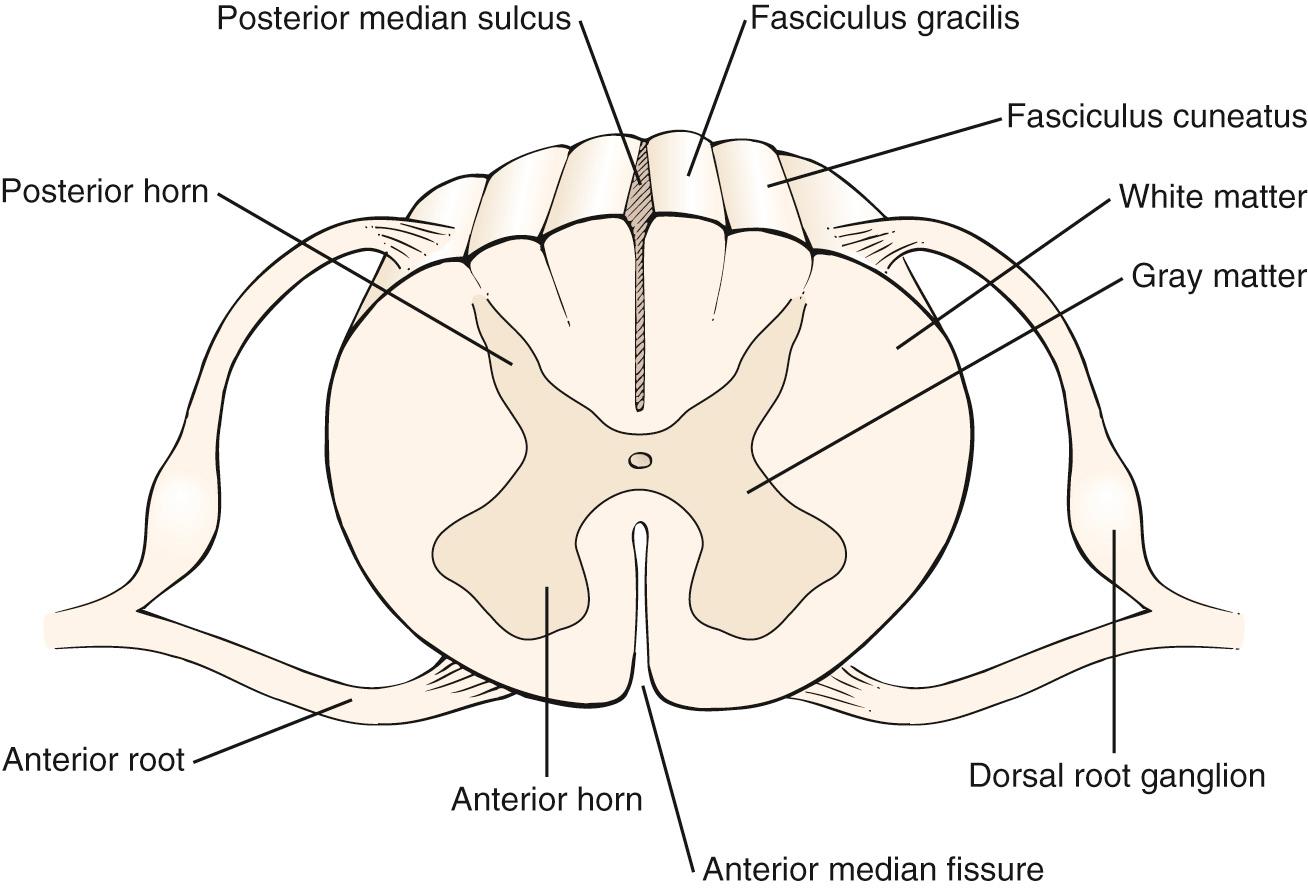
In the center of the spinal cord is the gray matter. The anterior gray matter, or the anterior horn, is the motor portion of the spinal cord and contains multipolar cells of origin of the anterior roots of the peripheral nerves. The lateral horn (sympathetic preganglionic neurons) is found at the T1 to L2 spinal levels. The posterior gray matter, or the posterior horn, is the receptor portion of the spinal cord.
The white matter of the spinal cord consists of tracts that link segments of the spinal cord and connect it to the brain. There are three main columns (funiculi). Between the anterior median fissure and the anterolateral sulcus is the anterior white column, which contains the descending fibers of the ventral corticospinal tract and the ascending fibers of the ventral spinothalamic tract. The ventral corticospinal tract is involved with voluntary motion, and the ventral spinothalamic tract carries impulses related to light touch.
The lateral white column is located between the anterolateral and posterolateral sulci and contains the descending fibers of the lateral corticospinal tract and the ascending spinocerebellar and lateral spinothalamic tracts. The lateral corticospinal tract is responsible for voluntary movement; the spinocerebellar tracts, for reflex proprioception; and the lateral spinothalamic tract, for pain and temperature sensation.
The posterior white column is located between the posterolateral and posterior median sulci. The most important fibers in this column are the ascending fibers of the fasciculus gracilis and fasciculus cuneatus. These tracts are involved with vibration sense, passive motion, joint position, and two-point discrimination.
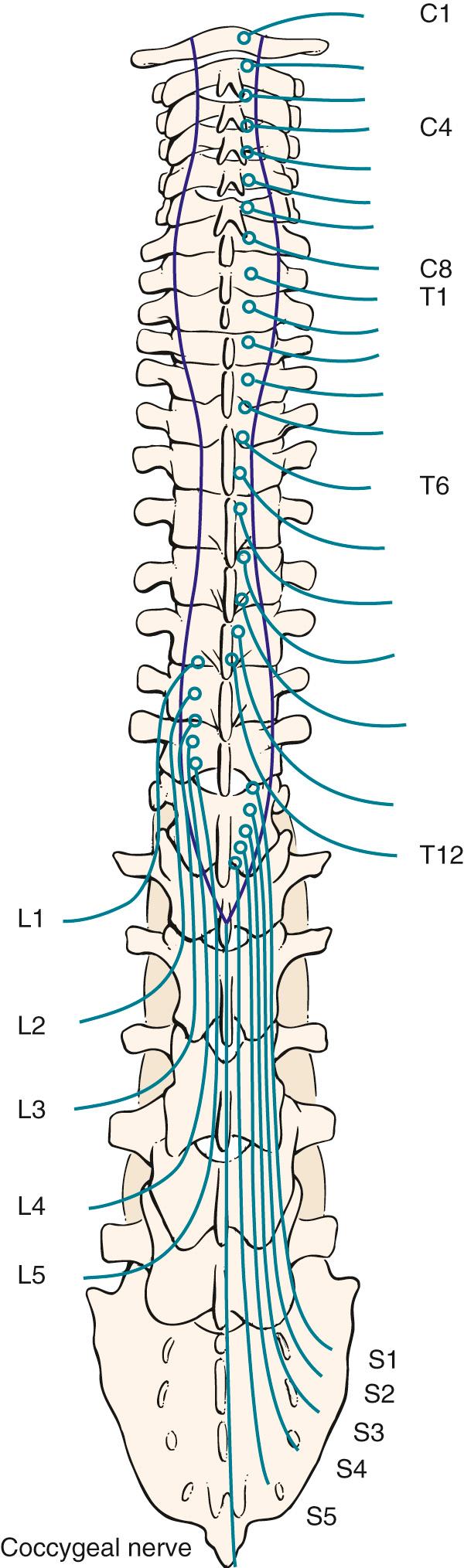
There are 31 pairs of spinal nerves, each with a ventral (motor) and dorsal (sensory) root. The ventral root consists of efferent nerve fibers, which originate in the anterior and lateral gray matter (T1 to T2 only) and travel to the peripheral nerve and muscle, which constitute the motor root. The dorsal root consists of afferent nerve fibers whose cell bodies are in the dorsal root ganglion , which is the sensory root.
The spinal nerves are grouped into 8 cervical (C1 to C8), 12 thoracic (T1 to T12), 5 lumbar (L1 to L5), 5 sacral (S1 to S5), and 1 coccygeal nerve. These nerves are illustrated in Fig. 21.7 .
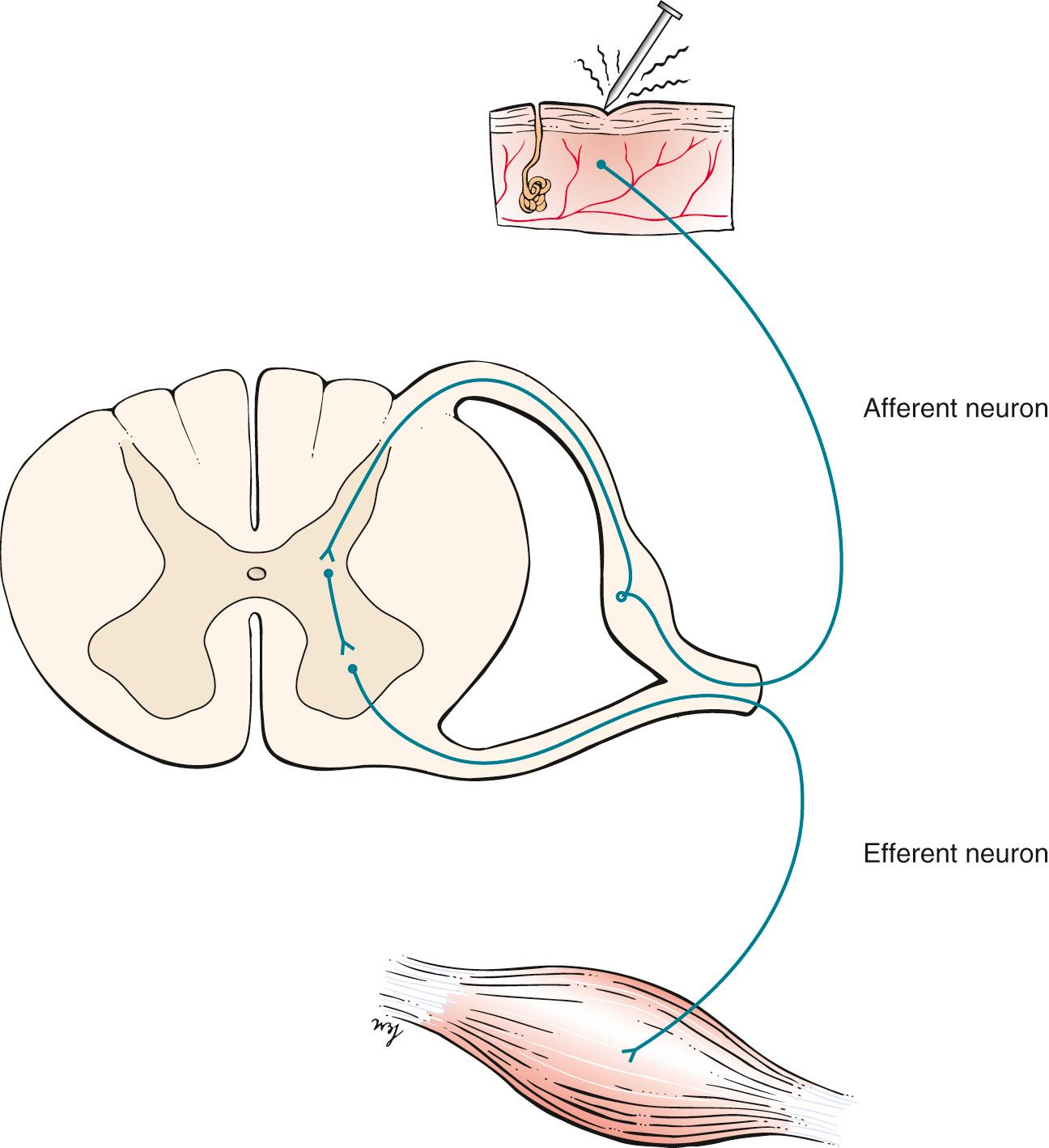
A spinal reflex involves an afferent neuron and an efferent neuron at the same level in the spinal cord. The basis for this reflex arc is an intact sensory limb, functional synapses in the spinal cord, an intact motor limb, and a muscle capable of responding. The afferent and efferent limbs travel together in the same spinal nerve. When a stretched muscle is suddenly stretched further, the afferent sensory limb sends impulses through its spinal nerve that travel to the dorsal root of that nerve. After reaching a synapse in the gray matter of the spinal cord, the impulse is transmitted to the ventral nerve root. These impulses are then conducted through the ventral root to the neuromuscular junction, where a brisk contraction of the muscle completes the reflex arc. Fig. 21.8 illustrates a reflex spinal arc.
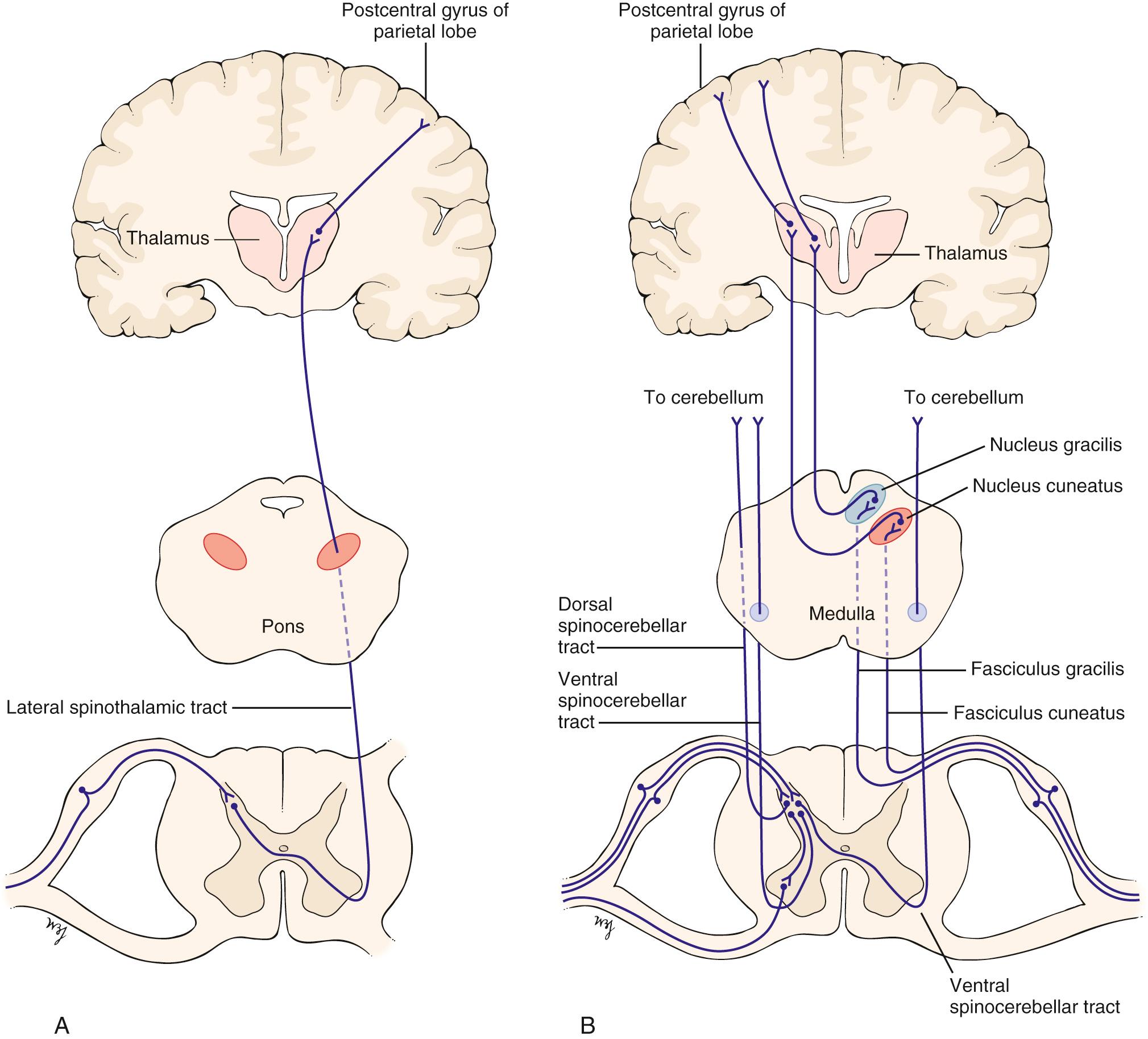
The afferent sensory limb is important not only in the reflex arc but also in the conscious appreciation of sensation. Nerve fibers carrying pain and temperature sensation enter the spinal cord and cross to the other side within one or two spinal segments. They ascend in the contralateral lateral spinothalamic tract, travel through the brain stem and the thalamus, and end in the postcentral gyrus of the parietal lobe, as illustrated in Fig. 21.9A . Fibers carrying proprioceptive sensation from muscles, joints, and tendons enter the dorsal root and participate in the reflex arc. Other fibers carrying proprioceptive sensation pass directly into the posterior columns and ascend in the fasciculi gracilis and cuneatus to their ipsilateral nuclei, cross in the medial lemniscus, reach a synapse in the thalamus, and end in the postcentral gyrus of the parietal lobe. Still other proprioceptive fibers ascend crossed and uncrossed in the spinocerebellar tracts to the cerebellum. These additional pathways are illustrated in Fig. 21.9B .
The most common symptoms of neurologic disease are as follows:
Headache
Loss of consciousness
“Dizziness”
Ataxia
Changes in consciousness
Visual disturbance
Dysphasia
Dementia
Cerebrovascular accident
Gait disturbance
Tremor
“Numbness”
“Weakness”
Pain
Headache is the most common neurologic symptom. It has been estimated that more than 35 million individuals in the United States suffer from recurrent headaches. Most of these patients have headaches that are related to migraine, muscle contraction, or tension. A headache pattern that is unchanged and has been present for several years is unlikely to be related to present illness of the patient. Several points must be clarified for any patient complaining of a recent change in the frequency or severity of headaches. Ask the following questions:
“How long have you been having headaches?”
“When did you notice a change in the pattern or severity of your headaches?”
“How has the pattern of your headaches changed?”
“How often do your headaches occur?”
“How long does each headache last?”
“Which part of your head aches?”
“What does the headache feel like?”
“How quickly does the headache reach its maximum?”
“When you get headaches, do you have any other symptoms?”
“Are you aware of anything that produces the headaches?”
“Are there any warning signs?”
“Does anything make the headaches worse?”
“What makes the headaches better?”
Patients complaining of a sudden onset of headache usually have more serious illnesses than patients with headaches of chronic duration. A continuous headache can be related to muscle spasm, whereas a recurrent headache may be a migraine or cluster headache. A throbbing headache often has a vascular cause. Certain headaches are associated with visual phenomena, nausea, or vomiting. In patients with increased intracranial pressure, any maneuver that increases the pressure, such as coughing or bending, may worsen the headache. In any patient who experiences a severe, sudden headache, stroke should be suspected.
Migraine is a biphasic type of headache associated with a prodromal phase, called the aura, followed by the headache phase. During the aura, one or more physiologic events may occur. These include transient experiences of autonomic, visual, motor, or sensory phenomena. Common visual symptoms are photophobia, blurred vision, and scotomata. As the aura fades, the headache begins. It is usually unilateral and is often described as pulsating; it can last for hours to days. Migraine headaches are often triggered by stress, anxiety, the use of birth control pills, and hormonal changes. Many patients experience migraine headaches after a period of excitement. Other important triggers are hunger and the ingestion of certain foods such as chocolate, cheese, cured meats, and highly spiced foods. There is often a family history of migraine.
Cluster headaches are associated with oculosympathetic disturbances. The typical patient is a middle-aged man complaining of recurrent episodes of pain around the eye that last for up to 1 hour. Classically, cluster headaches awaken the patient from sleep on successive nights for 2 to 4 weeks. There is ipsilateral miosis, ptosis, conjunctival edema, tearing, and nasal stuffiness during the headache. It is thought that alcohol may precipitate such attacks.
Headache may be the result of referred pain from sinus infections, ocular disease, or dental disease. Systemic conditions such as viral infections, chronic obstructive pulmonary disease, and poisoning may produce headaches. Determine whether the patient is taking any medications that may be producing the head pain. (See Table 21.2 at the end of this chapter, which provides an approach to patients with the symptom of headache.)
Loss of consciousness—syncope—may result from cardiovascular or neurologic causes. The cardiovascular causes are discussed in Chapter 14 , The Heart, and Chapter 15 , The Peripheral Vascular System. The term blackout is commonly used, but it may mean different conditions to the patient and the interviewer. Any patient who uses this term should be asked to clarify its meaning. The patient may be referring to an actual loss of consciousness, a dimming of vision, or a decreased awareness of the environment without an actual loss of consciousness.
A useful way to clarify the symptom of loss of consciousness is to ask the patient, “Have you ever lost consciousness, fainted, or felt that you were not aware of your surroundings?” If the patient answers in the affirmative, identify the cause of the loss of consciousness. Ask the following questions:
“Can you describe the attack to me—every event as it occurred until you lost consciousness?”
“Did anyone witness the attack?” 6
6 Document a history with an observer, if possible.
“Were there any symptoms that preceded the attack?”
“Were you told that there were body movements?”
“Can you describe everything you remember after the attack until you felt completely normal?”
“Was there a period of sleepiness that followed?” If yes, “For how long did this period last?”
“How did you feel after the attack? Were you confused?”
“Did you notice afterward that you had urinated or had a bowel movement during the attack?”
Epileptic seizures may produce a loss of consciousness and are caused by the sudden, excessive, disorderly discharge of neurons. The first step in approaching the symptom of seizure is to identify its type. If the discharge is focal, the clinical seizure reflects the effect of the excessive discharge in that area of the body. For example, if the discharge occurs in the inferior precentral gyrus, involved with hand and arm motion, the seizure is characterized by involuntary motion of the hand and arm. A generalized seizure results from a discharge in the subcortical structures, such as the thalamocortical radiations. These have widespread bilateral cortical connections. There are three main types of generalized seizures:
Petit mal (absence seizure)
Grand mal (generalized tonic-clonic)
Myoclonic
A petit mal seizure is characterized by a sudden attack of unconsciousness lasting only about 10 seconds, usually without any warning. During the petit mal seizure, the patient appears to be staring or daydreaming. There is no associated falling or involuntary limb motion. The patient rapidly returns to normal activity without being aware of the attack. These seizures are most common in children 5 to 15 years of age. On occasion, they may persist into adulthood.
A grand mal seizure is a generalized major motor convulsion. Affected patients lose consciousness, and many fall down rigidly. In 50% of patients with grand mal seizures, there is an aura of giddiness, involuntary twitching, change in mood, confusion, or epigastric discomfort as the seizure begins. Some patients may cry out initially. During this tonic phase, there is an increase in muscle tone, resulting in a rigid, flexed posture and then a rigid, extended posture. The patient may become apneic and cyanotic. The eyes may open and stare or may be deviated to one side. The clonic phase follows, with involuntary movements of the body. These are often associated with salivation, eye rolling, and incontinence. Biting the tongue is common. After the clonic phase, the individual passes into a phase resembling sleep from which she or he cannot be easily awakened. Postictally, or after the seizure, the patient may be confused and often falls into a deep sleep that lasts for hours. Accompanying muscle pain and headache are common.
A myoclonic seizure is a minor motor seizure characterized by sudden muscle contractions of the face and upper extremities. The eyelids and forearms are commonly affected. There is no detectable loss of consciousness.
Febrile convulsions are common in children from 6 months to 6 years of age and are similar to grand mal seizures. When a child has a high fever, a seizure lasting less than 10 minutes may occur. The younger the child is at the time of the first febrile seizure, the greater is the likelihood that seizures will recur.
Dizziness is a term used frequently by patients and should be avoided by the interviewer. “Dizziness” may be the patient's description of vertigo, ataxia, or lightheadedness. Any time the patient uses this term, it must be clarified by additional questioning, because different pathophysiologic mechanisms may be responsible. The interviewer needs to differentiate vertigo from ataxia. If the patient complains of “dizziness,” it is important to ask these questions:
“Would you describe the dizziness as a strange spinning sensation in your head?”
“Did the room spin, or did it feel as if you were spinning?”
“Were you unsteady while walking?”
Vertigo is partially discussed in Chapter 11 , The Ear and Nose. Vertigo is the hallucination of movement. Acute vertigo may be associated with nausea, vomiting, perspiration, and a sense of anxiety. Ask patients whether they have the sensation that objects are moving around them or that they are spinning or moving. In addition to the questions in Chapter 11 , ask the following:
“During the attack, did you experience any nausea or vomiting?”
“Have you noticed any problem with your hearing or ringing in your ears?”
“Have you ever been given an antibiotic called gentamicin?”
Ménière disease can result in protracted attacks of severe vertigo associated with vomiting. Many patients with Ménière disease also have the symptoms of tinnitus and hearing loss. During the attack, the patient is unsteady, with horizontal nystagmus directed away from the affected ear. Certain drugs (such as gentamicin) are associated with changes in the labyrinth of the ear and can cause vertigo and deafness.
Dizziness and stumbling are commonly associated with a stroke.
Disruption of the vestibular-ocular-cerebellar control mechanism produces ataxia. Ataxia is persistent unsteadiness in the upright position. Any patient complaining of dizziness must be evaluated for abnormal function of the vestibular, visual, proprioceptive, and cerebellar systems. Equilibrium requires the integration of sensory input and motor output, acting primarily at a reflex level for the maintenance of balance. The ears and eyes and their central connections in the brain stem and the cerebellum are intimately involved in balance. Any patient with ataxia should be asked the following questions:
“Are you unsteady when you walk?”
“Have you noticed that the dizziness is worse when your eyes are open or closed?”
“What does your diet consist of? What did you eat yesterday?”
“Have you ever had syphilis?”
Abnormal proprioceptive input from the lower extremities can cause ataxia. Severe posterior column damage from syphilis, vitamin B 12 deficiency, or multiple sclerosis may produce a “sensory” ataxia, resulting in a wide-based, high-stepping gait. The gait is worsened by having the patient close the eyes and is improved by having the patient observe the feet. Vitamin B 12 deficiency may result from pernicious anemia or from inadequate intake, although poor nutrition is a rare cause. “Motor” ataxia results from an abnormality in the cerebellum and central vestibular pathways. It is characterized by wide-based, irregular placement of the feet and poor placement of the center of gravity, with a lurching to either side.
Changes in consciousness may be related to changes in attention span, perception, arousal, or a combination. In confusional states, the patient can receive information normally, but the processing is disturbed. In delirium, the individual perceives the information abnormally. Any patient, or member of the patient's family, who indicates that a change in consciousness has occurred should be asked the following:
“Did the change occur suddenly?”
“Have there been other symptoms associated with the change in consciousness?”
“Do you use any medications? Depressants? Insulin? Alcohol? Recreational drugs?”
“Is there a history of psychiatric illness?”
“Is there a history of kidney disease? Liver disease? Thyroid disease?”
“Have you ever had an injury to your head?”
Many factors can produce changes in consciousness. The acuteness of the change in consciousness is often helpful in making a diagnosis. Hemiparesis, paresthesia, hemianopsia, garbled speech, and arm and leg weakness are common associated symptoms of supratentorial lesions. Brainstem lesions are often associated with changes in consciousness and with nystagmus, vomiting, double vision, nausea, and excessive yawning. Drugs of any type can produce acute changes in consciousness. A history of earlier psychiatric illness is important. Toxic and metabolic changes are frequently associated with changes in consciousness. Liver or kidney failure, myxedema, and diabetic ketoacidosis are common causes of metabolic abnormalities. A history of head trauma may result in a subdural hematoma and produce a gradual change in consciousness.
Visual disturbances are common neurologic presenting symptoms. The most important symptoms are acute visual loss, chronic visual loss, and double vision. Ask any patient complaining of visual disturbances the following questions:
“How long have you noticed these visual changes?”
“Is the visual loss associated with pain?”
“Did it occur suddenly?”
“Do you have a history of glaucoma?”
“Have you ever been told that you had a thyroid problem?”
“Do you have diabetes?”
Acute painless visual loss is caused by either a vascular accident or a retinal detachment. Painless loss of vision over a longer period occurs with compression of the optic nerve or tract or radiation. Glaucoma is often the cause of chronic, insidious, painless loss of vision. Acute narrow-angle glaucoma, however, may be responsible for transient loss of vision in association with intense ocular pain. Episodes of migraine may produce transient episodes of visual loss before the development of the headache. Amaurosis fugax is transient visual loss lasting up to 3 minutes and is a feature of internal carotid artery disease.
Double vision, or diplopia, is discussed in Chapter 10 , The Eye. Ocular motor palsies, thyroid abnormalities, myasthenia gravis, and brainstem lesions are well-known causes of diplopia. Ocular motor palsies can occur in trauma, multiple sclerosis, myasthenia gravis, aneurysms of the circle of Willis, diabetes, and tumors. Ask the following questions of any patient complaining of diplopia:
“Are you diabetic?”
“In which field of gaze do you have double vision?”
“Did the double vision occur suddenly?”
“Was there any pain associated with the double vision?”
“Has there been any injury to your head or eye?”
“Have you ever been told that your blood pressure was elevated?”
“Does the double vision get worse when you are tired?”
“Have you been exposed to the AIDS (acquired immune deficiency syndrome) virus?”
When a cranial nerve is affected, resulting in an extraocular muscle palsy, the patient may complain of diplopia in one field of gaze when the affected eye is unable to move conjugately with the other. Ocular palsies involve the third, fourth, and sixth cranial nerves. A complete third (oculomotor) nerve palsy causes ptosis, mydriasis, and loss of all extraocular movements except abduction. Trauma, multiple sclerosis, tumors, and aneurysms are the most frequent causes. Aneurysms of the posterior communicating artery can involve the third nerve, which passes near the artery on its way to the cavernous sinus. Cavernous sinus thrombosis, not infrequently seen in patients with AIDS, may also produce a complete third nerve palsy. Pupil-sparing third nerve, fourth (trochlear) nerve, and sixth (abducens) nerve palsies are seen in diabetic patients and in patients with long-standing hypertension. Patients with myasthenia gravis often have diplopia in the later part of the day as the muscles tire and weaken.
Visual disturbances, including blocked vision or loss of vision in one eye, blurry vision, or “graying out” are seen frequently in patients suffering a stroke.
Speech abnormalities, or dysphasia, may be either nonfluent (expressive) or fluent (receptive). In expressive aphasia, the speech pattern is hesitant and labored, with poor articulation. The patient has no problem with comprehension. When asked to say, “no ifs, ands, or buts,” the patient has great difficulty. In receptive aphasia, the speech is rapid and appears fluent but is full of syntax errors, with the omission of many words. Handwriting changes are nonspecific but indicate an impairment of neuromuscular control. Ask the following questions:
“Have you noticed any recent change in your speech pattern, such as slurring of your words?”
“Do you have trouble understanding things that are said to you?”
“Have you had any difficulty finding the right word in conversation?”
“Has your handwriting changed recently?”
Language problems, as well as slurred speech, are found commonly in patients suffering a stroke.
An important symptom of neurologic disease is failing memory. Dementia can be defined as the progressive impairment of orientation, memory, judgment, and other aspects of intellectual function. Dementia is a symptom rather than a specific disease entity. The most common cause of dementia is Alzheimer disease . Other causes include Parkinson disease, vascular disorders, metabolic disorders, drugs, tumors, vitamin B 12 deficiency, tertiary syphilis, and normal-pressure hydrocephalus. It is common for patients with early dementia to recognize an increasing inability to comprehend written material. They are aware also of their cognitive impairment but fail to acknowledge it with friends and family. It is often so insidious that individuals with dementia may live with their family for years without the family recognizing the problem. In addition, family members and friends may not wish to acknowledge the failing mental capacities.
Ask the patient and his or her friends and family the following:
“Have you noticed any change in your memory lately?”
“Do you have difficulty reading or understanding what you have read?”
“What was the patient's personality like a few years ago?”
“When was the last time the patient seemed normal?”
“What does the patient's diet consist of? Does he or she eat well?”
“Can the patient live alone?”
Strokes, or cerebrovascular accidents, are common. Most are thromboembolic (80%), but some are hemorrhagic (20%). Thirty percent of patients who sustain a stroke die within the first month. Most patients with strokes have paresis of at least one limb. Transient ischemic attacks (TIAs) are short episodes manifested by focal neurologic dysfunction. They usually last only a few minutes, after which complete recovery occurs. The importance of TIAs is that, in 30% of affected patients, a stroke occurs within 4 to 5 years.
Gait disturbances may occur for a variety of reasons. Gait may be changed by local pain in the foot, pain in a joint, claudication of the hip or leg, bone disease, vestibular problems, and extrapyramidal disorders. Interruption of the corticospinal tracts in the cerebrum after a stroke produces a spastic weakness in the contralateral leg. The foot is dragged, and the whole leg appears stiff and extended. Lesions in the spinal cord may produce a spastic paralysis affecting both legs. The gait is slow and stiff, with small steps. Patients with Parkinson disease walk stooped over, with short, quick, shuffling steps. Any patient with a gait disturbance should be asked the following:
“Do you have pain in your leg or hip when you walk?”
“Do you have diabetes?”
“Have you ever had syphilis?”
“What do you eat? Tell me everything you ate yesterday.”
Patients with vascular occlusive disease of the hip or leg may experience pain while walking and may alter their gait. Diabetes, syphilis, and pernicious anemia may produce a sensory loss, and each condition can result in gait abnormalities.
A tremor is a rhythmic motion of the distal parts of the limbs or head. A physiologic tremor has an oscillation of 10 to 12 cycles per second and is more obvious after exercise. A pathologic tremor is slower. Parkinson disease is the most frequently encountered extrapyramidal movement disorder. In this condition, the tremor is present at rest and is decreased with action. It has a frequency of 3 to 6 cycles per second and is worsened by anxiety. An intention, or ataxic, tremor is slow (2 to 4 cycles per second) and worsens on attempted movement. Multiple sclerosis is one of the many causes of intention tremor. Metabolic problems from liver or kidney failure are frequently responsible. Withdrawal from alcohol or caffeine is often a precipitating factor. Any patient with the symptom of tremor should be asked these questions:
“Does the tremor worsen when you try to do something?”
“Is there a history of thyroid disease?”
“Have you ever been told about any problems with your liver or kidneys?”
“What is your daily consumption of alcoholic beverages?”
“How much coffee or tea do you drink?”
“How much chocolate do you eat?”
Chorea is involuntary jerky motions of the face and limbs. A common cause is Huntington disease, in which chorea is accompanied by personality changes and progressive mental deterioration terminating in dementia.
Numbness is another term used by patients to indicate a variety of problems. “Numbness” can be used by patients to describe a “pins-and-needles” sensation, coolness, pain, or clumsiness. The interviewer should be sure to clarify the meaning. The examiner must be careful during the physical examination to palpate the distal pulses in any patient complaining of numbness, because arterial insufficiency is a possible cause. Diabetes mellitus is a common cause of lower extremity numbness. Multiple sclerosis may cause numbness in any extremity.
Weakness may be a symptom of the motor system. A patient with a proximal arm motor weakness complains of difficulty brushing hair, shaving, or reaching up to shelves. A patient with distal arm motor weakness complains of difficulty putting a button through a buttonhole, using keys, or writing with a pen or pencil. Proximal leg motor weakness is characterized by difficulty climbing stairs or getting into bed or the bathtub. Foot drop is a classic sign of distal leg motor weakness. Chapter 20 , The Musculoskeletal System, reviews some of the important questions related to weakness.
Face droop and weakness are common signs of a stroke, as is the presence of numbness or clumsiness in one arm or hand.
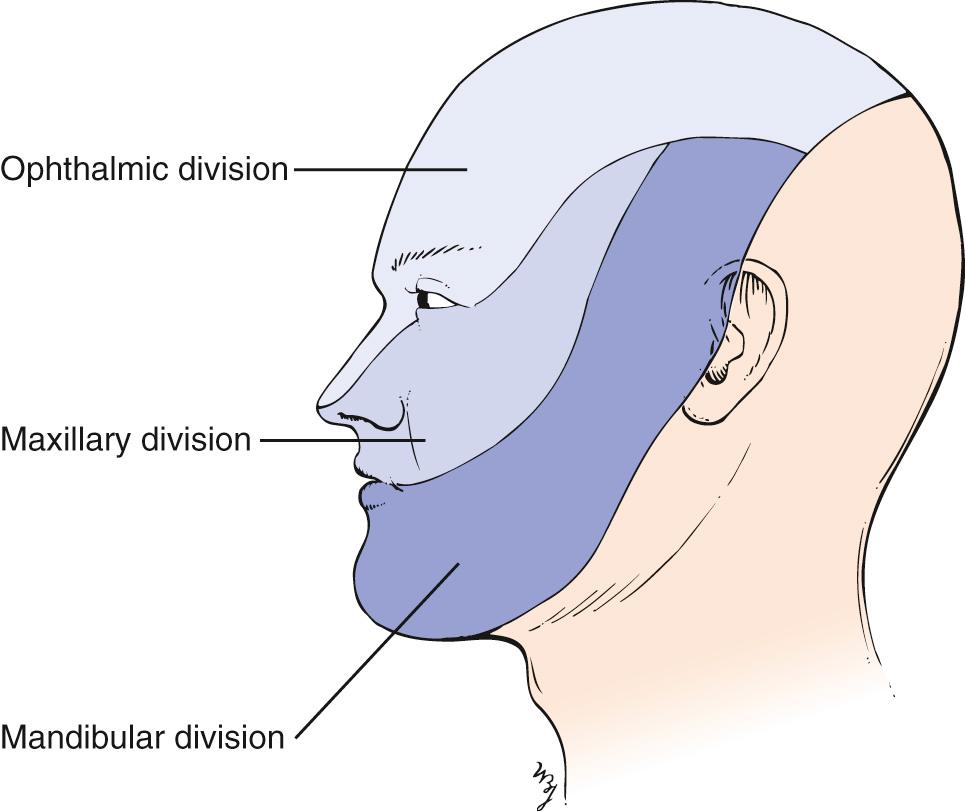
Pain is an infrequent symptom of neurologic disease, but it merits mention. Trigeminal neuralgia, also known as tic douloureux, is the occurrence of severe, jabbing pain lasting only seconds in the distribution of the maxillary or mandibular divisions of the trigeminal nerve ( Fig. 21.10 ). It is frequently provoked by motion, touch, eating, or exposure to cold temperatures. Another cause of facial pain is the cluster headache, already discussed. Herpes zoster infection of a sensory nerve root, also known as shingles, manifests with intense pain along the distribution of that nerve root. The classic linear, vesicular skin eruption develops 3 to 4 days later along the distribution of the nerve. Fig. 8.70 shows the classic dermatologic manifestations of herpes zoster infection of spinal nerve T3.
Sciatica is intense pain shooting down the leg in the distribution of the sciatic nerve. In this condition, there is impingement of portions of the sciatic nerve by the vertebrae. Arthritis of the lumbosacral spine is frequently the cause.
Sometimes the paresthesias associated with demyelinating diseases are so intense that the patient may describe them as pain.
Patients with inflammation of the meninges often complain of pain in the neck and a resistance to flexion of the neck. If meningitis is suspected, have the patient lie on his or her back. Place your hand behind the patient's neck and flex it until the chin touches the sternum. In patients with meningitis, there is neck pain and resistance to motion. This is called Brudzinski sign. There may also be flexion of the patient's hips and knees. Jósef Brudzinski described at least five different physical signs indicative of meningeal irritation. This sign is the best known and most reliable sign. Another sign of meningeal irritation can be elicited while the patient lies on the back and you flex one of the patient's legs at the hip and knee. If pain or resistance is elicited as the knee is extended, a positive Kernig sign is present.
The ramifications of chronic neurologic disease on the patient and his or her family are enormous. All family members experience emotional pain while observing the progressive clinical changes. The family bears an immense personal burden in assisting the patient to cope with disability.
One example of a progressive neurologic condition is Alzheimer disease. A devastating chronic disorder of unknown cause, Alzheimer disease is the most common diffuse brain degeneration causing brain failure. This condition is characterized by progressive and widespread brain degeneration with a hopeless prognosis.
Memory problems and impairment of intellectual function are the main symptoms of Alzheimer disease. Depression is common. Patients may have significant cognitive impairment, which ruins their ability to negotiate their environment. They may forget where they live. They may forget to turn off a gas burner on the stove or to put out a cigarette. They may wander aimlessly outdoors.
Manifestations of Alzheimer disease span a clinical spectrum from awareness of the disability to a vegetative state. Many patients lose touch with reality. During an interview with such a patient, it may become clear that even the ability to describe the patient's own medical history has been lost.
Early in the course of the disease, affected patients may use a number of circumlocutions, such as substituting words when they cannot find more appropriate ones. Another early change is disorientation about time and place. Visual hallucinations are common. Lack of interest in sex is almost universal. Motor behavior diminishes progressively as impairment of consciousness increases. An important characteristic is the development of bizarre thoughts and fantasies that come to dominate consciousness. Delusions, especially delusions of persecution, are common.
In the early stages of the disease—when patients are still aware of their environment but have experienced the symptom of memory loss—mild depression, anxiety, and irritability are common. As the disease progresses, apathy is the dominant feature. Patients may appear indifferent and emotionally withdrawn. In others in whom there is increased motor activity, anxiety and fear are common. In these individuals, terror and panic attacks are not uncommon. Hostility and paranoia develop rapidly. Regression and sudden displays of highly charged emotion are the responses to their frequent hallucinations.
In milder cases, depression, hypochondriasis, and phobic features abound. Hysterical conversion reactions, such as hysterical blindness, may occur. Social interaction is lost, and the patient may suddenly explode with anger, anxiety, or tears. As the disease progresses, suicide attempts are common. Emotional lability is often extreme, with periods of laughter followed by crying. With progressive disease, dullness of affect and lack of an emotional response occur as gross neurologic disability develops. In the terminal stages, patients with Alzheimer disease may show severe body wasting with profound brain failure.
The equipment necessary for the neurologic examination consists of safety pins, cotton-tipped applicators, a 128-Hz tuning fork for vibration sense, a 512-Hz tuning fork for hearing, gauze pads, familiar objects (coins and keys), and a reflex hammer.
The neurologic examination consists of assessment of the following:
Mental status
Cranial nerves
Motor function
Reflexes
Sensory function
Cerebellar function
See .
During the interview, the examiner has already gained much insight into the mental status of the patient. The interviewer may have already been able to assess the patient's remote memory, affect, and judgment. The formal mental status portion of the neurologic examination is introduced by saying to the patient, “I would like to ask you a few routine questions. Some of them you will find very easy. Others will be more difficult. Do the best you can.”
The mental status examination consists of evaluation of the following:
Level of consciousness
Speech
Orientation
Knowledge of current events
Judgment
Abstraction
Vocabulary
Emotional responses
Memory
Calculation ability
Object recognition
Praxis
The level of consciousness can be assessed as soon as you introduce yourself to the patient. Is the patient awake? Alert? Is the patient's sensorium clouded by exogenous or endogenous insults? Does the patient appear confused? If the patient does not respond to your introduction, hold the patient's hand and softly say, “Hello, Mr./Ms. ____. Can you hear me? If you hear me, squeeze my hand.” If there is no response, try gently shaking the patient. If there is still no response and the patient appears obtunded, squeezing the nipple or applying pressure with your thumb to the bony ridge under the eyebrow is a painful maneuver that may rouse the patient. If these maneuvers fail to awaken the patient, the patient is in coma. Patients who are in coma are completely unconscious and cannot be roused even by painful stimuli. If either painful stimulus is used, be careful not to pinch the skin or bruise the patient. If friends or relatives are present, make sure to explain to them what you are doing.
If the patient is awake and alert, you have already observed his or her speech. The patient should now be asked to recite short phrases such as “no ifs, ands, or buts.” Is dysarthria, dysphonia, dysphasia, or aphasia present? Dysarthria is difficulty in articulation. In general, lesions of the tongue and palate are responsible for dysarthria. Dysphonia is difficulty in phonation. The result is an alteration in the volume and tone of the voice. Lesions of the palate and vocal cords are often responsible. Dysphasia is difficulty comprehending or speaking as a result of cerebral dysfunction. Patients with a total loss of speech have aphasia. Different areas of the brain are responsible for the different types of aphasia. A motor, expressive, nonfluent aphasia is present when patients know what they want to say but have motor impairment and cannot articulate properly. They understand written and verbal commands but cannot repeat them. A frontal lobe lesion is often the cause. A sensory, receptive, fluent aphasia is present when the patient articulates spontaneously but uses words inappropriately. The patient has difficulty understanding written and verbal commands and cannot repeat them. A temporoparietal lesion is frequently the cause.
The patient's orientation to person, place, and time must be established. Orientation refers to the person's awareness of self in relation to other persons, places, and time. Disorientation occurs in association with impairment of memory and attention span. The patient should be asked these questions:
“What is today's date?”
“What is the day of the week?”
“What month is this?”
“What is the season now?”
“What is the name of this hospital (or building)?”
To evaluate orientation, do not ask if the patient knows his or her name or other questions that cannot be verified. Patients with an early cognitive impairment are cagey in providing answers if they do not know the correct answer; they hope that you will accept their answer and not pursue the question. As an example, if an examiner asks, “Where are you now?” and the patient does not remember the address, he or she might reply with an answer like, “I'm in your office.” You should then ask, “But where is my office?”
Knowledge of current events can be assessed by asking an American patient to name the last four presidents of the United States. Asking the patient the name of the local mayor or governor is also useful. If the patient is not American or is unfamiliar with American affairs, asking the patient about more general current events may be more useful. The ability to name current events requires an intact orientation, intact recent memory, and the ability to think abstractly.
Evaluation of judgment is performed by asking the patient to interpret a simple problem. Ask the patient the following:
“What would you do if you noticed an addressed envelope with an uncanceled stamp on it on the street near a mailbox?”
“What would you do if you were in a crowded movie theater and a fire started?”
A correct response to the first question would be to pick up the letter and mail it. An example of an incorrect response might be, “I'd throw it in the trash.” Judgment requires higher cerebral function.
Abstraction is a higher cerebral function that requires comprehension and judgment. Proverbs are commonly used to test abstract reasoning. The patient should be asked to interpret the following:
“People who live in glass houses shouldn't throw stones.”
“A rolling stone gathers no moss.”
A patient with an abnormality in abstract reasoning might respond to the first quotation with a concrete interpretation, such as, “The glass will break if you throw a stone through it.” A concrete interpretation of the second proverb might be “Moss grows only under rocks that don't move and not under a rolling stone.” Concrete responses are common in patients with mental retardation or brain failure. Schizophrenic patients often answer with concrete interpretations, but bizarre assessments are also common. Be careful when assessing abstraction in patients whose mother tongue is not English. They may also provide concrete answers as they literally translate the words of the proverb.
Another method of testing abstract reasoning is to ask the patient how two items are similar or dissimilar. You might ask, “What is similar about a dog and a cat?” “What is similar about a church and a synagogue?” or “What is dissimilar about an apple and a chicken?”
Vocabulary is often difficult to assess. It is based on many factors, which include the patient's education, background, work, environment, and cerebral function. It is, however, an important parameter in assessing intellectual capacity. Patients who are mentally challenged have a limited vocabulary, whereas those with mild brain failure have a well-preserved vocabulary. Patients should be asked to define words or use them in sentences. Any words can be used, but they should be asked in order of increasing level of difficulty. The following list is an example:
Car
Ability
Dominant
Voluntary
Telescope
Reticent
Enigma
Although emotional response has probably been informally observed already, inquire specifically whether the patient has noticed any sudden mood changes. It is appropriate to ask, “How are your spirits?” During the interview, the interviewer has already noticed the patient's affect, which is the emotional response to an event. The response may be appropriate, abnormal, or flat. An appropriate response to a loved one's death may be to cry. An inappropriate response is to laugh. A flat response shows little emotion. Patients with bilateral cerebral damage lose control of their emotions.
To test memory, have the patient recall the recent and the remote past. Recent memory is easily tested by presenting three words to the patient and asking them to repeat them 5 minutes later. For example, tell the patient, “Repeat these words after me and remember them. I will ask for them later: necklace, thirty-two, barn.” Continue with the mental status examination. Five minutes later, ask the patient, “What were those words I asked you to remember?”
A simpler test of memory is to have the patient recall as many elements in a category as possible. Request that the patient do one of the following:
“Name as many flowers as you can.”
“Name as many occupations as you can.”
“Name as many tools as you can.”
An abnormality in recent memory may be related to a lesion in the temporal lobe.
To test the remote past memory, ask the patient about well-known events in the past. Do not ask about events that you cannot verify.
The ability to calculate depends on the integrity of the dominant cerebral hemisphere, as well as on the patient's intelligence. Ask the patient to perform simple arithmetic problems, such as subtracting 7 from 100, then 7 from the result, then 7 from the result, and so forth. This is the serial sevens test. If there is difficulty with serial sevens, ask the patient to add or subtract several numbers, such as “How much is 5 plus 7? How much is 12 plus 9? How much is 27 minus 9?”
Object recognition is termed gnosia. Agnosia is the failure to recognize a sensory stimulus despite normal primary sensation. Show the patient a series of well-known objects, such as coins, pens, eyeglasses, or pieces of clothing, and ask the patient to name them. If the patient has normal vision and fails to recognize the object, visual agnosia is present. Tactile agnosia is the inability to recognize an object by palpation in the absence of a sensory deficit. This occurs with a lesion in the nondominant parietal lobe. Autotopagnosia is the term used to describe a patient's inability to recognize his or her own body part, such as the hand or leg.
Praxis is the ability to perform a motor activity. Apraxia is the inability to perform a voluntary movement in the absence of deficits in motor strength, sensation, or coordination. Dyspraxia is the decreased ability to perform the activity. The patient hears and understands the command but cannot integrate the motor activities that will complete the action. Ask a patient to pour water from the bedside pitcher into a glass and drink the water. A patient with dyspraxia may either drink the water from the pitcher or try to drink from the empty glass. A deep frontal lobe lesion is frequently responsible for this disorder.
Another type of apraxia is constructional apraxia. In this condition, the patient is unable to construct or draw simple designs. The examiner draws a shape and asks the patient to copy it. Alternatively, the patient can be asked to draw the face of a clock. Patients with constructional apraxia often have a lesion in the posterior portion of the parietal lobe.
The examination of the cranial nerves should be carried out in an orderly manner. Several of the cranial nerves have already been evaluated. Table 21.1 lists the cranial nerves, their functions, and the clinical findings when a lesion exists.
| Cranial Nerve | Function | Clinical Findings With Lesion |
|---|---|---|
| I: Olfactory | Smell | Anosmia |
| II: Optic | Vision | Amaurosis |
| III: Oculomotor | Eye movements, papillary constriction, accommodation | Diplopia, ptosis, mydriasis, loss of accommodation |
| IV: Trochlear | Eye movements | Diplopia |
| V: Trigeminal | General sensation of face, scalp, and teeth; chewing movements | “Numbness” of face; weakness of jaw muscles |
| VI: Abducens | Eye movements | Diplopia |
| VII: Facial | Taste; general sensation of palate and external ear; lacrimal gland and submandibular and sublingual gland secretion; facial expression | Loss of taste on anterior two thirds of tongue, dry mouth, loss of lacrimation, paralysis of facial muscles |
| VIII: Vestibulocochlear | Hearing; equilibrium | Deafness, tinnitus, vertigo, nystagmus |
| IX: Glossopharyngeal | Taste, general sensation of pharynx and ear, elevation of palate, parotid gland secretion | Loss of taste on posterior one third of tongue, anesthesia of pharynx, partially dry mouth |
| X: Vagus | Taste; general sensation of pharynx, larynx, and ear; swallowing; phonation; parasympathetic innervation to heart and abdominal viscera | Dysphagia, hoarseness, palatal paralysis |
| XI: Spinal accessory | Phonation; head, neck, and shoulder movements | Hoarseness; weakness of head, neck, and shoulder muscles |
| XII: Hypoglossal | Tongue movements | Weakness and wasting of tongue |
The olfactory nerve supplies nerve endings to the superior nasal concha and upper one third of the nasal septum. The olfactory nerve is not routinely tested. However, in any patient with a suspected frontal lobe disorder, the olfactory nerve should be evaluated.
The patient is asked to close the eyes and one nostril as the examiner brings a test substance close to the patient's other nostril. The patient is instructed to sniff the test substance. The substance must be volatile and nonirritating, such as cloves, vanilla beans, freshly ground coffee, or lavender. The use of an irritating agent such as alcohol would involve cranial nerve V, as well as cranial nerve I, and the test results would be inaccurate.
Each nostril is tested separately. The examiner asks the patient to identify the test material. A unilateral loss of smell, known as unilateral anosmia, is more important than a bilateral loss, because it indicates a lesion affecting the olfactory nerve or tract on that side.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here