Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The human microbiome has received considerable attention as a previously underappreciated factor in human health and disease. Alterations in the microbiome are associated with several clinical conditions, and restoration of a normal intestinal microbiome can be beneficial in selected situations.
The so-called normal flora of microbes that live in and on the human body are part of the normal human microbiome. Although most attention has been paid to bacteria, this term can also encompass the Archaea, yeast, and viruses. The term microbiota refers to the microbes themselves, whereas the term microbiome refers to a specific community of microbes (i.e., microbiota) and the specific environment that they inhabit. This distinction is important because the microbiome encompasses the microbiota and also the environment they inhabit. This environment is shaped not only by the microbes but also by the host and the external environment. For example, the intestinal microbiome is composed of the microbes that inhabit this organ as well as the intestinal contents, which includes compounds derived from food as well as from the human host, such as digestive enzymes, mucin, and bile acids.
The function of microbes in a specific environment can be ascertained by examining not only the community members but also determining the complete metabolic environment that these microbes inhabit. This metabolic environment is defined not only by the microbes but also by the host. A specific example is the metabolism of bile acids found in the intestinal tract. Synthesized in the liver and excreted in bile in the form of bile salts conjugated to the amino acids taurine and glycine, these primary conjugated bile salts are further metabolized by members of the intestinal microbiota, which can remove these conjugated amino acids and further alter the chemical structure through enzymatic activities such as dehydroxylation. Secondary bile acids, which result from the microbe-mediated conversion of primary bile acids, have different chemical properties and thus influence host physiology in a differential manner. Bile acid receptors are differentially stimulated by various secondary bile acids, so metabolism of bile acids by the microbiota will have a direct influence on host physiology.
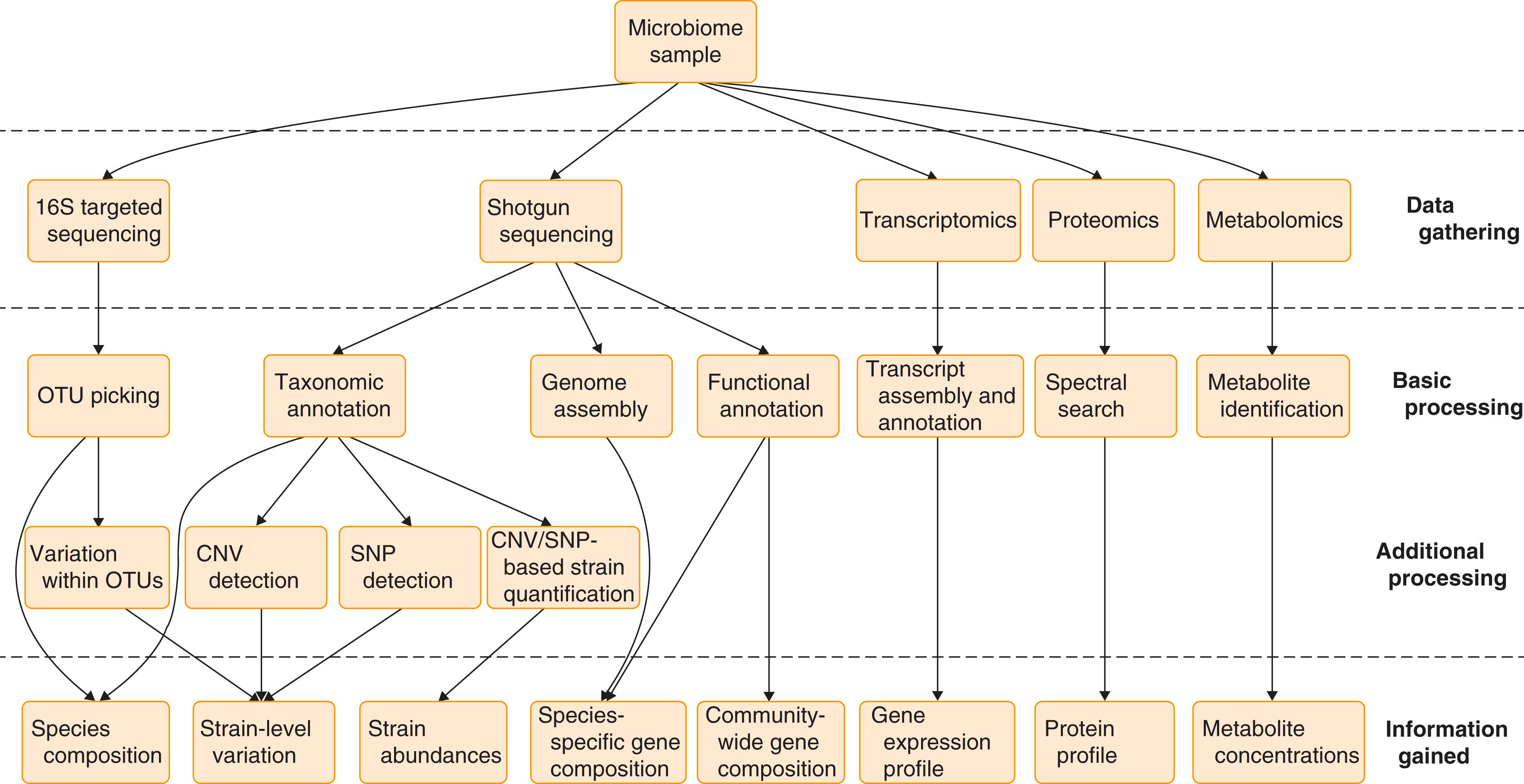
The microbiome is usually analyzed by nucleic acid sequencing–based techniques and mass spectrometry ( E-Fig. 257-1 ). In some cases the information is limited to the structure (anatomy) of a microbial community in terms of the species composition and relative abundance of the microbes that are present. Functional data (physiology) can be gained by assaying metabolic potential or direct measurement of functional output in terms of gene expression and a catalog of the metabolites that are present in the microbiome. A remaining question that often lingers in these studies is whether specific changes that are associated with a specific health state is positive or merely reflects the altered environment that is created by the presence of that state. Ongoing research is endeavoring to determine whether alterations in the microbiome truly have a causal role for associated disease.
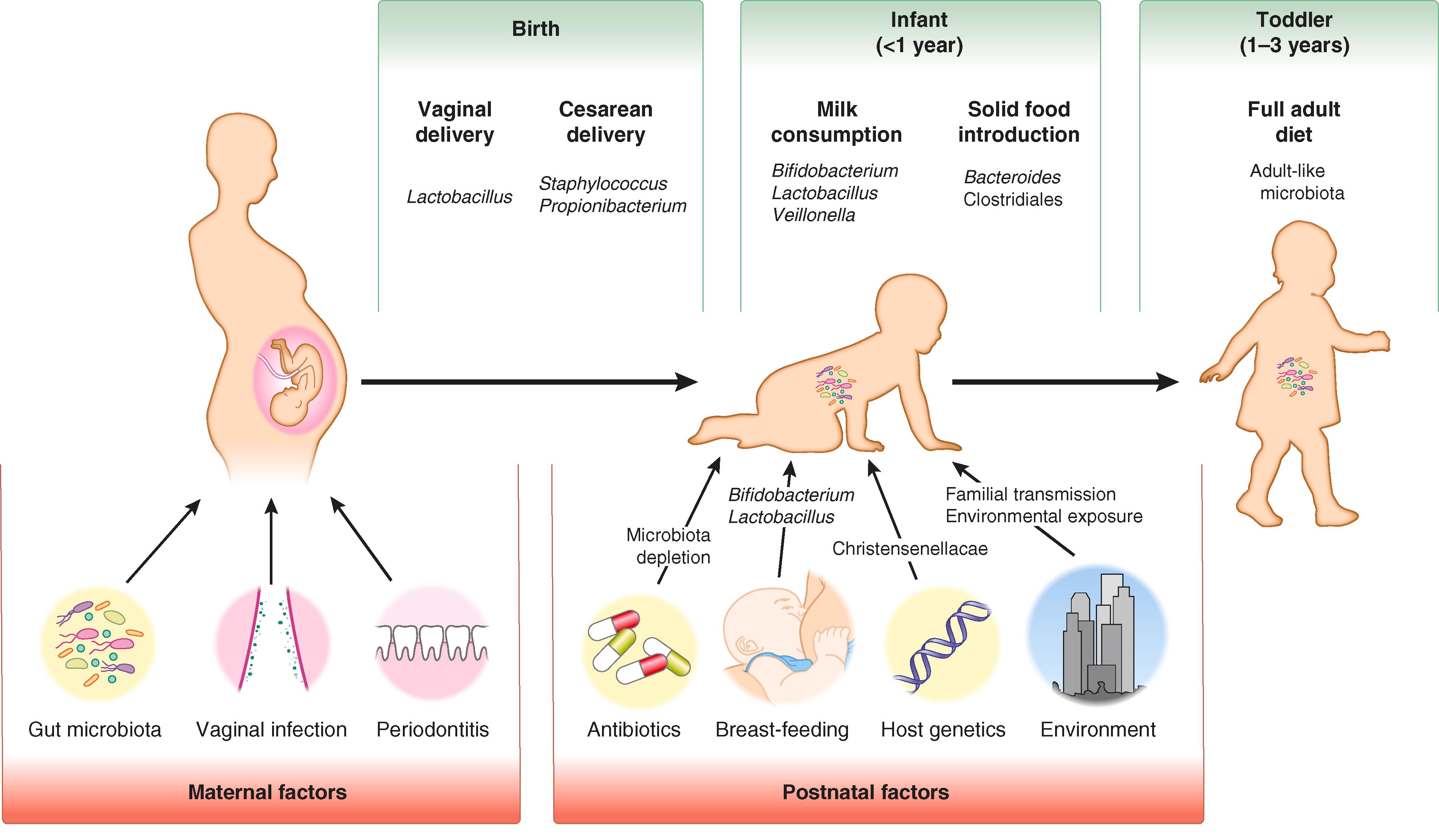
The birth mode can have at least a short-term effect on the composition of the microbiota of a newborn. Neonates who undergo vaginal birth have a distinct microbiome shortly after birth compared with children born by cesarean delivery. These distinctions resolve as the child grows older. What is unknown is whether these differences in early colonization have long-lasting effects on the health of the child. It is possible that these differences in initial microbiomes may underlie the known epidemiologic associations between cesarean birth and conditions such as asthma and allergies.
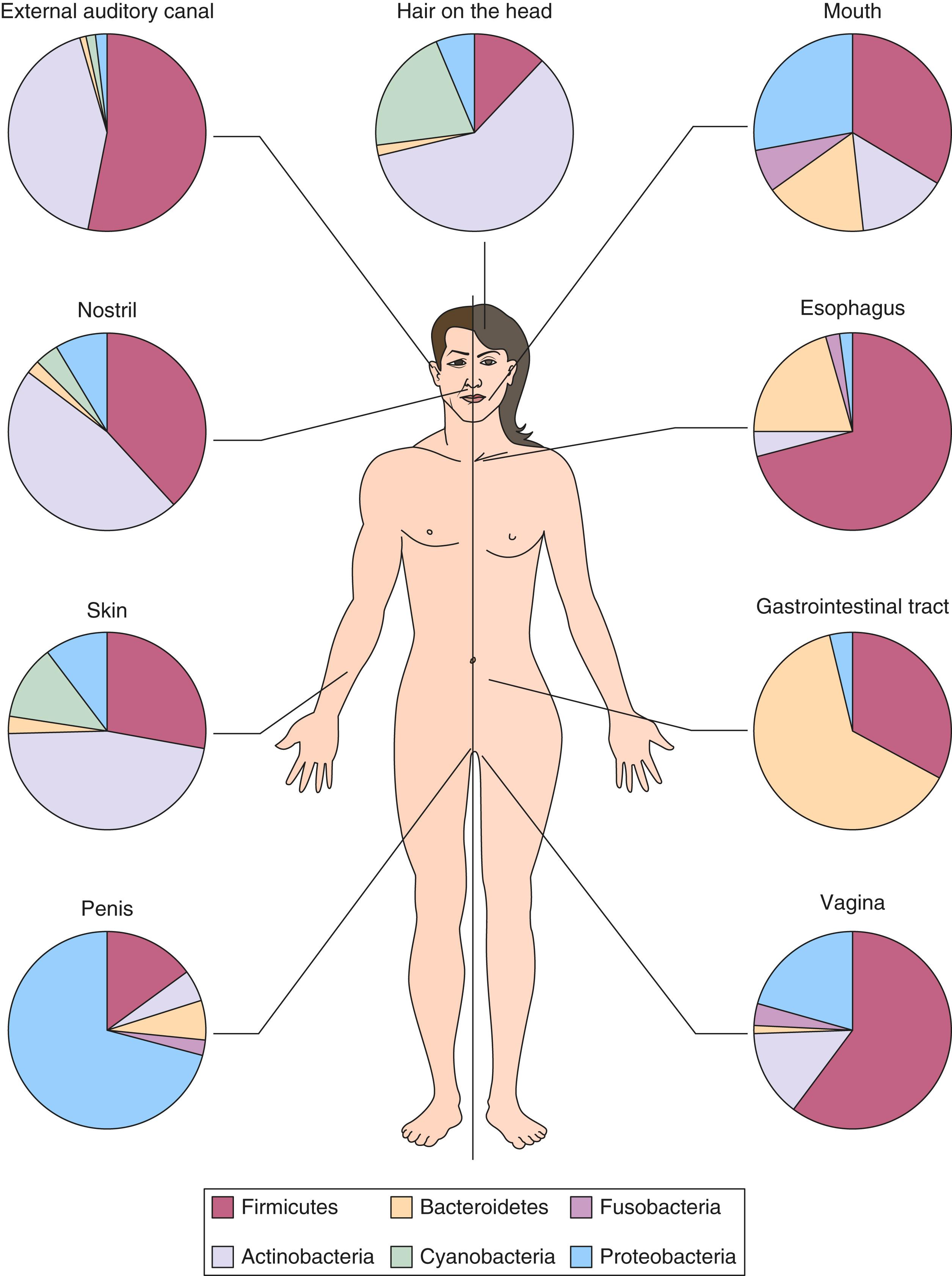
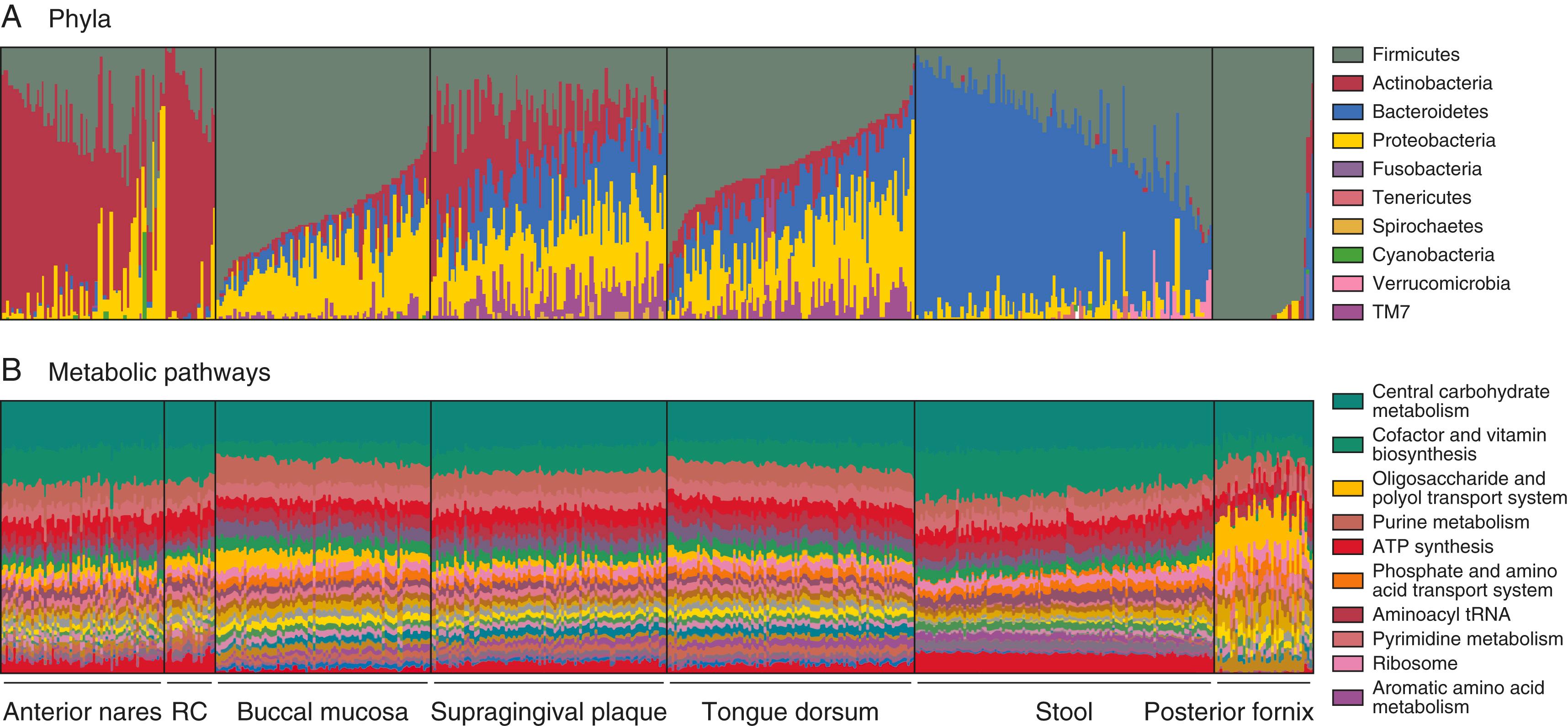
In addition to birth mode, a number of postnatal factors such as use of antibiotics, breast-feeding, diet, and host genetics are thought to affect the developing microbiota of the child ( E-Fig. 257-2 ). After an “adult-like” microbiota is established, the microbiota varies by body region ( Fig. 257-1 ) and among individuals, but the sum total of the microbial genes shows much less variation ( E-Fig. 257-3 ). The interpretation is that although the specific composition of the normal, healthy microbiota may vary from person to person, conserved functions are present in a healthy community.
Given the apparent conservation of microbiome function in healthy individuals, an extensive literature has evaluated alterations in the microbiota. However, a causal role by which the altered microbiota leads to disease has been demonstrated only for a few conditions.
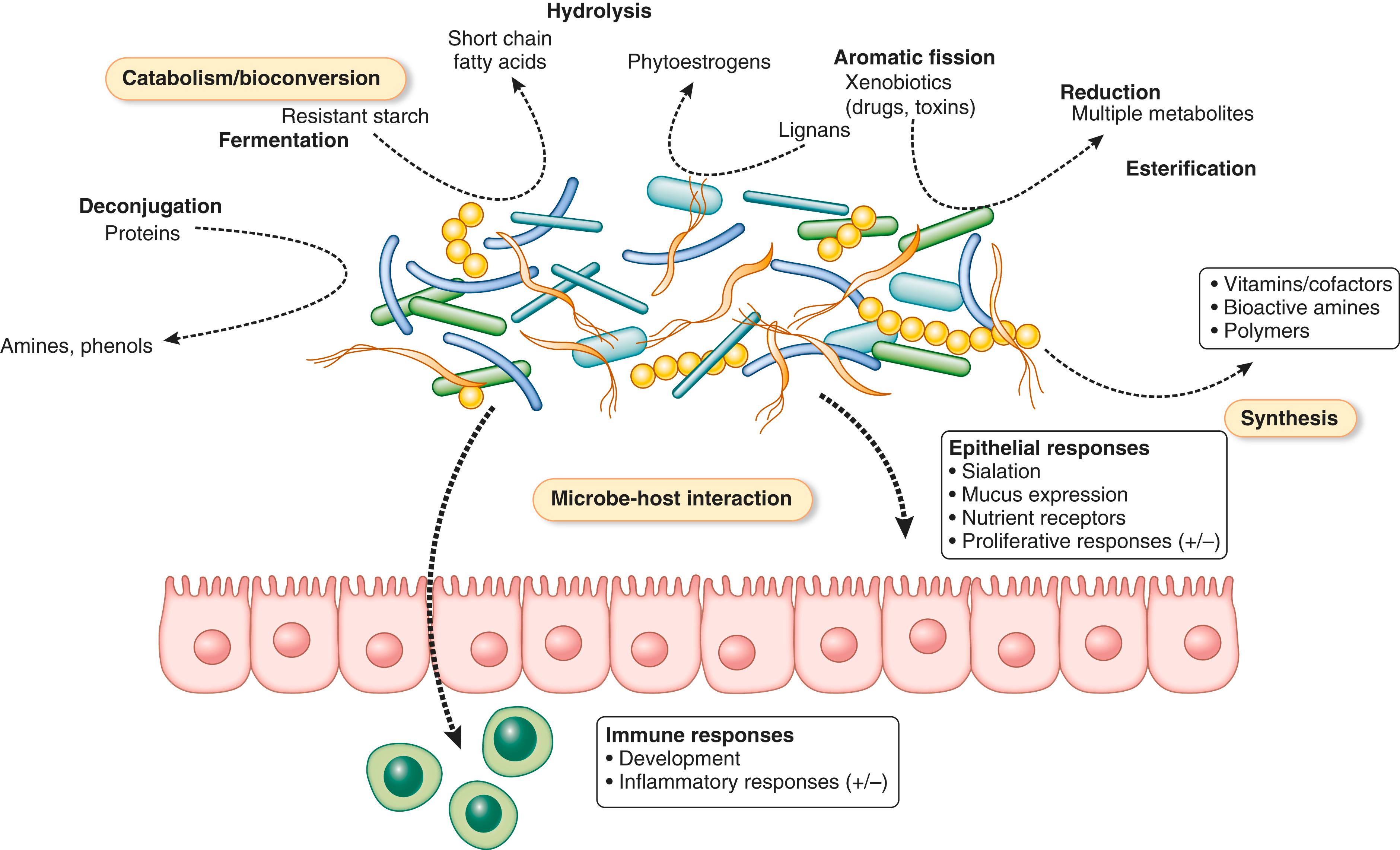
The microbiota possesses a wealth of metabolic potential for a wide range of catabolic and bioconversion activities ( Fig. 257-2 ). Dietary substances such as carbohydrates and proteins can be metabolized by the indigenous gut microbiota. Additionally, host-derived biomolecules, including bile acids and compounds such as mucous and mucosal secretions, can be substrates for microbial metabolism. Xenobiotics, such as drugs and environmental toxicants, also can be subject to microbe-mediated conversion. In addition to catabolism and bioconversion, microbes can synthesize vitamins and bioactive compounds, such as amines and neurotransmitters (e.g., levodopa). Finally, host-microbe contact can directly alter the function of host tissues. Microbial contact with the immune system and mucosal surfaces, during both postnatal development and maturity, can influence gene expression and thus function of the host.
Given the breadth of functions attributed to the indigenous microbiota, it is clear that alteration of a diverse microbiome can lead to disruption of homeostasis and reduced protection against pathogens. This disruption can be due to loss of a given function, inappropriate expression of a function in time or space, or introduction of maladaptive functions ( Table 257-1 ). These mechanisms can involve the host, microbes (both resident and invasive), and environmental factors. The latter can include factors such as medications, notably antibiotics, and surgical procedures that can alter anatomy or introduce foreign material.
| HOST FACTORS |
| Birth mode Genetics Gender Immune status Age Preexisting disease Anatomic disruption (e.g., gastrointestinal surgery, implantation of medical devices) |
| ENVIRONMENTAL/IATROGENIC FACTORS |
| Diet Residence (urban vs. rural) Animal exposure (including pets) Environmental toxicants (naturally occurring or humanmade) Antibiotics Other drugs (e.g., chemotherapy, proton pump inhibitors, anti-inflammatory drugs) |
| MICROBIAL FACTORS |
| Infections (viral, bacterial, fungal, helminthic) Ingestion of fermented foods (e.g., yogurt, kimchee, kefir) Use of probiotic organisms |
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here