Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Humans have never been immune from injury, and doubtless the practice of bonesetting was not unfamiliar to our most primitive forebears. Indeed, given the known skills of Neolithic humans at trepanning the skull, it would be surprising if techniques of similar sophistication had not been brought to bear in the care of injuries. However, no evidence of this remains.
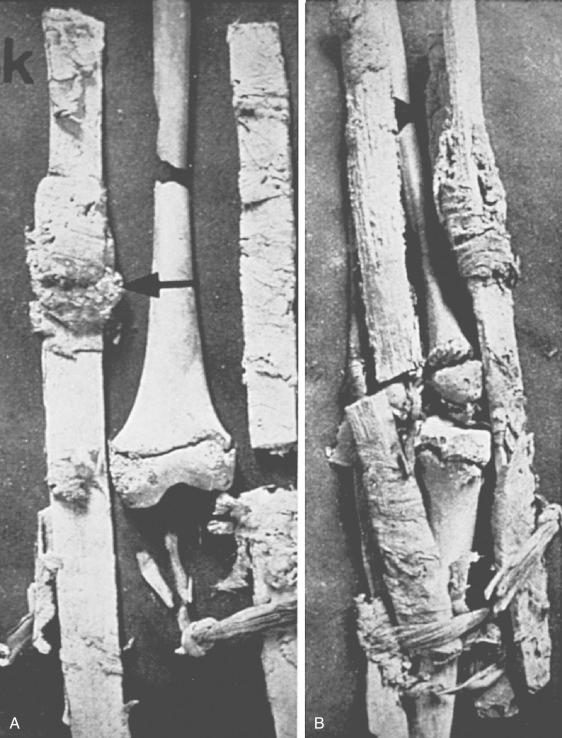
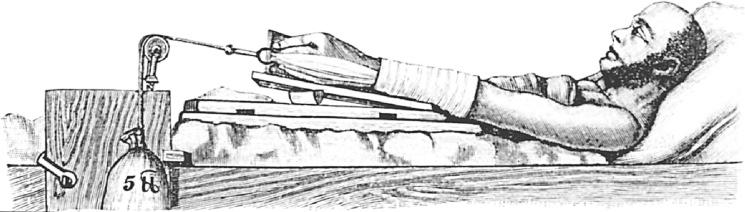
The earliest examples of the active management of fractures in humans were discovered at Naga-ed-Der (about 100 miles north of Luxor in Egypt) by Professor G. Elliott Smith during the Hearst Egyptian expedition of the University of California in 1903. Two specimens were found of splinted extremities. One was an adolescent femur with a compound, comminuted midshaft fracture that had been splinted with four longitudinal wooden boards, each wrapped in linen bandages. A dressing pad containing blood pigment was also found at approximately the level of the fracture site. The victim is judged to have died shortly after injury, as the bones show no evidence whatsoever of any healing reaction ( Fig. 74.1 ). The second specimen was of open fractures of a forearm, treated by similar splints, but in this case a pad of blood-stained vegetable fiber (probably obtained from the date palm) was found adherent to the upper fragment of the ulna, evidently having been pushed into the wound to stanch bleeding. Again, death appears to have occurred before any bone healing reaction had started. The Egyptians were known to be skilled at the management of fractures, and many healed specimens have been found. The majority of femoral fractures had united with shortening and deformity, but a number of well-healed forearm fractures have been discovered.
Some form of wooden splintage bandaged to the injured limb has been used from antiquity to the present day. Certainly, both Hippocrates and Celsus described in detail the splintage of fractures using wooden appliances, but a fascinating account of external splintage of fractures is to be found in the work of El Zahrawi ( ad 936–1013). This Arab surgeon, born in Al Zahra, the royal city 5 miles west of Cordova in Spain, was named Abu'l-Quasim Khalas Ibn'Abbas Al-Zahrawi, commonly shortened to Albucasis. In his 30th treatise, “The Surgery,” he described in detail the application of two layers of bandages, starting at the fracture site and extending both up and down the limb, after reduction of the fracture. He continued:
Then put between the bandages enough soft tow or soft rags to correct the curves of the fracture, if any, otherwise put nothing in. Then wind over it another bandage and at once lay over it strong splints if the part be not swollen or effused. But if there be swelling or effusion in the part, apply something to allay the swelling and disperse the effusion. Leave it on for several days and then bind on the splint. The splint should be made of broad halves of cane cut and shaped with skill, or the splints may be made of wood used for sieves, which are made of pine, or of palm branches, or of brier or giant fennel or the like, whatever wood be at hand. Then bind over the splints another bandage just as tightly as you did the first. Then over that tie it up with cords arranged in the way we have said, that is with the pressure greatest over the site of the fracture and lessened as you move away from it. Between the splints there should be a space of not less than a finger's breadth.
It is of interest that the brother of the celebrated French surgeon Bérenger Féraud, an interpreter with the French army in Algeria, wrote in 1868 that all Arab bonesetters ( tebibs [a tebib is an Arab medicine man, whence the modern French slang word toubib, meaning quack or doctor]) carried with them “sticks of kelar, a sort of fennel, well dried and of extreme lightness, which are used as splints.” Albucasis then went on to describe various forms of plaster that may be used as an alternative, particularly for women and children, recommending “mill dust, that is the fine flour that sticks to the walls of a mill as the grindstone moves. Pound it as it is, without sieving, with egg white to a medium consistency, then use.” He suggested as an alternative plaster a mixture of various gums, including gum mastic, acacia, and the root of mughath (Glossostemon bruguieri), pounded fine with clay of Armenia or Asia Minor and mixed with water of tamarisk or with egg white.
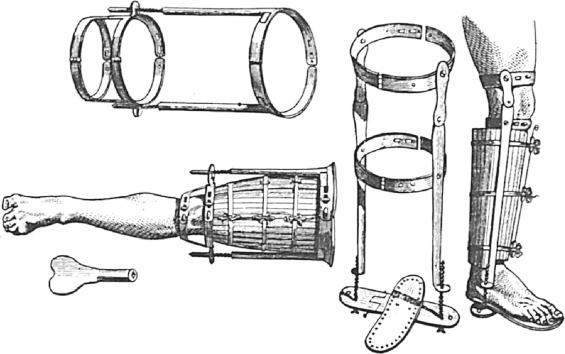
In 1517, Gersdorf beautifully illustrated a novel method of binding wooden splints, using ligatures around the assembled splint that are tightened by twisting them with cannulated wooden toggles, with a wire then passed down the hollow centers of the toggles to prevent them from untwisting ( Fig. 74.2 ). In this book, he also illustrated the use of an extension apparatus for overcoming overriding of the fractures of the bones, although similar machines had been in use for centuries according to the descriptions of Galen, Celsus, and Paulus Aegineta.

Gersdorf's technique of tightening a circumferential splint ligature was plagiarized by Benjamin Gooch, who in 1767 described what must be regarded as the first functional brace ( Fig. 74.3 ), designed as it was to return the worker to labor before the fracture had consolidated. Gooch fashioned shape splints for various anatomic sites; these consisted of longitudinal strips of wood stuck to an underlying sheet of leather that could then be wrapped around the limb and held in place with ligatures and cannulated toggles. I recollect Gooch splintage still being used for temporary immobilization of injured limbs by ambulance crews as late as the 1960s. Gooch's are perhaps the most sophisticated wooden splints ever devised. The 19th century literature abounds with descriptions of many types of wooden fracture apparatus, none of which is as carefully constructed or apparently efficient as those of Gooch.
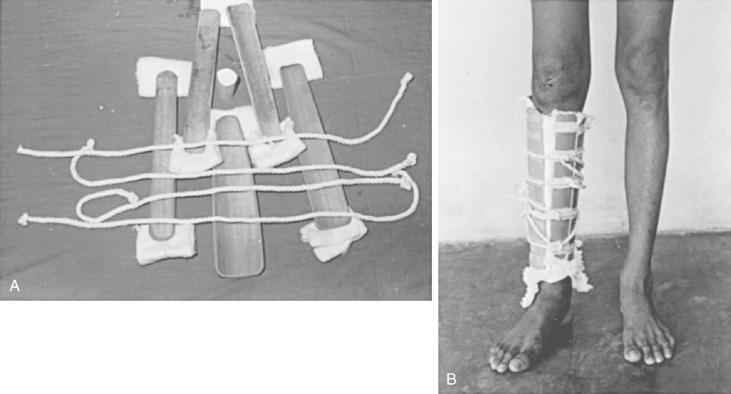
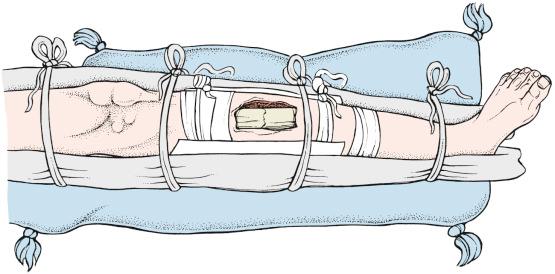
The use of willow board splints for the treatment of tibial shaft fractures and Colles’ fractures in modern times has been described in great detail by Shang T'ien-Yu and colleagues in a fascinating description of the integration of modern and traditional Chinese medicine in the treatment of fractures. Amerasinghe and Veerasingham continued to use shaped bamboo splints, held in place by circumferential rope ligatures, in the functional bracing of tibial fractures in Sri Lanka ( Fig. 74.4 ). They reported 88% of their patients to be weight bearing and freely mobile by 10 weeks, with a 95% union rate, and less than half an inch of shortening in 85% of patients. The Liston wooden board splint for fractures of the femoral shaft is currently in use in one institution in Scotland for the management of this injury in children.
As indicated previously, El Zahrawi, probably drawing from the work of Paulus Aegineta, described the use of both clay gum mixtures and flour and egg white for casting materials. In ad 860, the Arab physician Rhazes Athuriscus wrote, “But if thou make thine apparatus with lime and white of egg it will be much handsomer and still more useful. In fact it will become as hard as stone and will not need to be removed until the healing is complete.”
William Cheselden (1688–1752), the famous English surgeon and anatomist, as a schoolboy sustained an elbow fracture that was treated in this manner. In his book Anatomy of the Human Body, he recorded, “I thought of a much better bandage which I had learned from Mr. Cowper, a bonesetter at Leicester, who set and cured a fracture of my own cubit when I was a boy at school. His way was, after putting the limb in a proper posture, to wrap it up in rags dipped in the whites of eggs and a little wheat flour mixed. This drying grew stiff and kept the limb in good posture. And I think there is no way better than this in fractures, for it preserves the position of the limb without strict [tight] bandage which is the common cause of mischief in fractures.” Cheselden was later reputed to have been able to perform a lithotomy procedure in 68 seconds; it would appear that his functional result was excellent. A more precise use of the technique of Rhazes was introduced into France by Le Dran in the late 18th century; he stiffened his bandage with egg white, vinegar, and powder of Armenian clay or plaster.
The technique of pouring a plaster-of-Paris mixture around an injured limb would appear to have been used in Arabia for many centuries and was brought to the attention of European practitioners by Eaton, a British diplomat in Bassora, Turkey. In 1798 he wrote:
I saw in the eastern parts of the Empire a method of setting bones practised, which appears to me worthy of the attention of surgeons in Europe. It is by inclosing [sic] the broken limb, after the bones are put in their places, in a case of plaster of Paris (or gypsum) which takes exactly the form of the limb without any pressure and in a few minutes the mass is solid and strong [ Fig. 74.5 ]. This substance may be easily cut with a knife and removed and replaced with another. When the swelling subsides, [and] the cavity is too large for the limb, a hole or holes being left, liquid gypsum plaster may be poured in which will perfectly fill up the void and exactly fit the limb. A hole may be made at first by placing oiled cork or a bit of wood against any part where it is required and when the plaster is set it is to be removed. There is nothing in gypsum injurious if it be free from lime. It will soon become hard and light and the limb may be bathed with spirits which will penetrate through the covering. I saw a case of a most terrible compound fracture of the leg and thigh by the fall of a cannon. The person was seated on the ground and the plaster case extended from below the heel to the upper part of his thigh, where a bandage fastened into the plaster went round his body.

This technique of plâtre coulé was enthusiastically embraced in Europe in the early 19th century. Malgaigne recorded in detail the various techniques of its use, stating that he found it first employed by Hendriksz at the Nosocomium Chirurgicum of Groningen in 1814. Shortly afterward Hubenthal, believing himself to be its inventor, described plâtre coulé in the Nouveau Journal de Médecine. In 1828, Keyl, working with Dieffenbach at the Charity Hospital in Berlin, finally succeeded in calling general attention to it. Although the Berlin surgeons applied the method only to fractures of the leg, Hubenthal had described its use in fractures of the forearm, the hand, and the clavicle, mixing the plaster powder with unsized paper (similar to blotting paper). He encased the limb in a trough made of pasteboard, closed at the top and bottom with toweling, and first poured in the mixture to encase only the posterior half of the limb. After this posterior cast was allowed to set, the edges were smoothed, notched, and then oiled so that a second anterior cast could be created by applying the paste to the front of the limb, thus ending up with two halves of a cast, which could be bandaged together, yet easily separated for wound inspection or to relieve any tension. Malgaigne himself was not keen on plâtre coulé and after having problems with swelling within a rigid cast, albeit incomplete over the crest of the tibia, he abandoned the technique in favor of albuminated and starched bandages of the type recommended by Seutin—bandage amidonné.
A great variety of other apparatuses have been devised over the centuries for the management of fractures, notably the copper limb cuirasse described by Heister and what Malgaigne called “the great machine of La Faye.” The latter was made of tin and consisted of longitudinal pieces that were hinged together so that it could be laid flat beneath the limb and then wrapped around. It was described as confining “at once the pelvis, thigh, leg and foot, hence it ensured complete immobility.” Bonnet of Lyons went one stage further by producing an apparatus for the management of fractures of the femur that enveloped both legs, the pelvis, and the trunk up to the axillae. The great disadvantage of all these extensive and heavy forms of immobilization of the limb was that the patient was largely confined to bed during the whole period of fracture healing. This disadvantage was particularly emphasized by Seutin, who, in recommending his bandage amidonné, or starched bandage, wrote:
It has not yet been well understood that complete immobility of the body, whilst being recommended by authors as an adjunct to other curative methods, is truly but a last resort which one would be better to avoid than to prescribe. One has not previously dared to say that the consolidation of the bony rupture is certainly more sure and prompt than the injured person's recovery of movements and (ability) to forget thereby his affliction, in order to take up again at least part of his ordinary occupation. Early mobilization causes neither accident nor displacement of the fragments. In permitting the patient to distract himself and take himself out into the fresh air, instead of remaining nailed to his bed, it has the happiest influence on the formation and consolidation of callus.
Again we see the roots of the concept of functional bracing. Seutin showed a man with a light starched bandage on his leg, the limb suspended by a strap around his neck, and walking with crutches.
In the first half of the 19th century, battle lines were drawn between the European surgeons who prescribed total immobilization and those who followed Seutin's déambulation regimen, and much intellectual effort was wastefully expended in fruitless argument. Seutin's emphasis on the importance of joint motion was also appreciated by others. In 1875 Sir James Paget wrote, “With rest too long maintained the joint becomes stiff and weak, even though there be no morbid process in it; and this mischief is increased if the joint hath been too long bandaged.” A little later, Lucas-Championnière wrote:
The immobilisation of the members, which was dogma not open for discussion in the treatment of fractures and as well articular lesions, has been practised with such contentment by the authors of the immovable apparatuses, that we threw ourselves with abandon into all forms of immobilisation. It was forbidden even to discuss such immobilisation and to criticise it in the name of healthy physiology. When I attacked, at the Society of Surgery, this forced immobilisation, I was called by Verneuil an “ankylophobe” and I remained practically alone in protesting against these practises, which are so contrary to the interests of the injured and the ill. … Absolute immobilisation is not a favourable condition for bony repair. … [A] certain quantity of movement, regulated movement, is the best condition for this process of repair.
He then described animal experiments that confirm this view and went so far as to recommend massage of the injured limb to produce some degree of movement between the fragments. He was particularly vitriolic in his condemnation of prolonged immobilization of children and became the great champion of early and graduated controlled mobilization, not only to achieve union of the fracture but also to prevent edema, muscle atrophy, and joint stiffness, later to be christened fracture disease.
The battle of minds between the mobilizers and the immobilizers was neither won nor lost but rather forgotten with the advent of the plaster-of-Paris bandage. In Holland in 1852, Antonius Mathijsen (1805–1878) published a new method for the application of plaster in fractures. As a military surgeon, he had been seeking an immobilizing bandage that would permit the safe transport of patients with gunshot wounds to specialized treatment centers. He sought a bandage that could be used at once, would become hard in minutes, could be applied so as to give the surgeon access to the wound, was adaptable to the form of the extremity, would not be damaged by wound discharge or humidity, and was neither too heavy nor too expensive. His exact technique was described by van Assen and Meyerding as follows:
He cut pieces of double folded unbleached cotton or linen to fit the part to be immobilized. Then the pieces were fixed and held in position by woollen thread or pins. The dry plaster which was spread between the layers remained two finger breadths within the edges of the cloth. The extremity was then placed on the bandage, which was moistened with water. Next the edges of the bandage were pulled over so that they overlapped one another and they were held by pins. When an opening in the bandage was necessary, a piece of cotton wool the size of the desired opening was placed between the compresses so that this area remained free of plaster. In cases in which it was found necessary to enlarge the cast, enlargement could be achieved by the application of cotton bandages, four inches wide, rubbed with plaster and moistened.
Mathijsen introduced his plaster bandage in 1876 at the Centennial Exhibition in Philadelphia at the invitation of his friend Dr. M. C. Gori. The use of plaster-of-Paris bandages for the formation of fracture casts became widespread after Mathijsen's death and replaced most other forms of splintage.
Although the fire of the intellectual contest between the mobilizers and the immobilizers was reduced to mere embers, it was not extinguished, and the early functional concepts of Gooch, Seutin, Paget, Lucas-Championnière, and many others continued for decades to be regarded by surgical orthodoxy as heretical. In Britain, the great advocate of rest—enforced, prolonged, and uninterrupted—in the management of skeletal disorders, both traumatic and nontraumatic, was Hugh Owen Thomas ( Fig. 74.6 ), who came from a long line of unqualified bonesetters residing in the Isle of Anglesey. Hugh Thomas's father, Evan Thomas, left his home and agricultural background to work in a foundry in Liverpool. His native skills as a bonesetter rapidly became legendary, and he opened consulting rooms in Liverpool, developing an extensive practice. His eldest son, Hugh Owen, broke with family tradition and qualified in medicine in 1857. His attempt at a partnership with his father failed, and he set himself up as a general practitioner in the slums of Liverpool, where he worked for 32 years, reputedly taking only 6 days of vacation. He died in 1891 at the age of 57.

There cannot be an orthopaedic surgeon in the world who is not familiar with the Thomas splint, still in current use in many centers throughout the world in the management of fractures of the femur, although it was originally designed to assist in the management of tuberculous disease of the knee joint ( Fig. 74.7 ). As discussed later, the use of this splint in World War I saved many lives. Not the least of the contributions of this industrious, single-minded, chain-smoking eccentric was to fire his nephew with enthusiasm for orthopaedic surgery. Robert Jones, later to be knighted, practiced with his uncle Hugh for many years in Liverpool before becoming one of the best known orthopaedic surgeons in the English-speaking world. Hugh Owen Thomas and Robert Jones were the two men to whom Watson Jones dedicated his classical work Fractures and Joint Injuries, writing of them, “They whose work cannot die, whose influence lives after them, whose disciples perpetuate and multiply their gifts to humanity, are truly immortal.” Watson Jones remained greatly influenced by Hugh Owen Thomas's belief in enforced, uninterrupted, and prolonged rest, and in the preface to the fourth edition of his book, he described one of its chapters as
… a vigorous attack upon the almost universally accepted belief that contact compression, lag screws, slotted plates, compression clamps, and early weight bearing promote the union of fractures. I do not accept a word of it. Forcible compression of bone is pathological rather than physiological and it avails in the treatment of fractures only insofar as it promotes immobility and protects from shear. In believing this and denying the view that is held so widely, I reiterate the observations of Hugh Owen Thomas. Moreover, I believe that gaps between the fragments of a fractured bone are always filled if immobility is complete. … I still believe firmly that, apart from interposition of muscle and periosteum, the sole important cause of nonunion is inadequate immobilization.
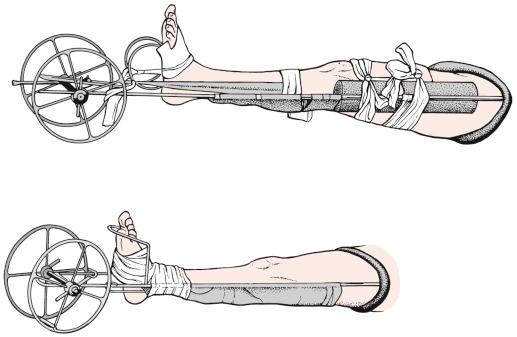
Although longitudinal traction of the limb to overcome the overriding of fracture fragments had been described as early as the writings of Galen ( ad 130–200), in which he described his own extension apparatus, or glossocomium ( Fig. 74.8 ), this traction was immediately discontinued once splintage had been applied. The use of continuous traction in the management of diaphyseal fractures seems to have appeared around the middle of the 19th century, although Guy de Chauliac (1300 to 1367) wrote in Chirurgia Magna, “After the application of splints, I attach to the foot a mass of lead as a weight, taking care to pass the cord which supports the weight over a small pulley in such a manner that it shall pull on the leg in a horizontal direction (Ad pedum ligo pondus plumbi transeundo chordam super parvampolegeam; itaque tenebit tibiam in sua longitudinae) .”

Whereas Sir Astley Cooper in his celebrated treatise on dislocations and fractures of the joints illustrated the method of treating simple fractures of the femur on a double inclined plane with a wooden splint strapped to the side of the thigh, there is no mention in his work of the use of traction. On the other hand, in his book on fractures and dislocations published in 1890, Albert Hoffa of Wurzburg (where Roentgen discovered x-rays) liberally illustrated the use of traction for many types of fractures—not only of the femur in adults and children but also of the humerus. Straight arm traction for supracondylar and intercondylar fractures of the distal humerus recently so in vogue was clearly described and illustrated by Helferich in 1906 ( Fig. 74.9 ).
Certainly one of the earliest accounts of the use of continuous skin traction in the management of fractures must be that of Dr. Josiah Crosby of New Hampshire. He described the application of “two strips of fresh spread English adhesive plaster, one on either side of the leg, wide enough to cover at least half of the diameter of the limb from above the knee to the malleolar processes.” Over these he laid a firm spiral bandage before applying weight to the lower ends of the adhesive straps. He recorded the use of this method in a fracture of the femur, an open fracture of the tibia, and, surprisingly, two cases of fracture of the clavicle in 2-year-old children. The technique of Dr. Crosby was illustrated in detail by Hamilton in his treatise on military surgery. Billroth, describing his experiences between 1869 and 1870, gave the alternatives of plaster-of-Paris bandages or extension in the management of fractures of the shaft of the femur. He stated, “On the whole, I far prefer extension by means of ordinary strapping. This I apply generally on Volkmann's plan.” It is interesting to note that in the early descriptions of traction for the management of fractures of the femoral shaft, when no other form of splintage was used, union was usually said to have been consolidated by 5 or 6 weeks, in comparison with the 10 to 14 weeks that later came to be regarded as the average time to femoral shaft union using traction in association with external splintage.
The rapid consolidation of femoral shaft fractures was, of course, stressed by Professor George Perkins of London in the 1940s and 1950s, when he abandoned external splintage and advocated straight simple traction through an upper tibial pin and immediate mobilization of the knee, using a split bed (so-called Pyrford traction). This was in some ways a development and simplification of the traction principles outlined by R. H. Russell (who also remarked on rapid consolidation with early movement), describing his mobile traction in 1924. In the same year, Dowden, speaking mainly of upper limb fractures, wrote, “The principle of early active movement in the treatment of practically all injuries and in most inflammations will assuredly be adopted before long.” Perkins, like Dowden and the many others before, was a great advocate of movement, both active and passive, of all the joints of the involved limb as being more important than precise skeletal form.
Given that Gooch's description in 1767 of the first tibial and femoral functional braces was to remain obscure for more than two centuries, it is surprising that after the intense discussion of the technical minutiae and principles of splintage in the 19th century, there was no real modification of the “standard” plaster-of-Paris cast until the work of Sarmiento, published 200 years after that of Gooch. Following experience with patellar tendon-bearing below-knee limb prostheses, Sarmiento developed a patellar tendon-bearing cast for the treatment of fractures of the tibia, applied after initial standard cast treatment had been used to permit the acute swelling to settle. This heralded the renaissance of functional bracing, and in 1970 Mooney and colleagues described hinged casts for the lower limb in the management of femoral fractures treated initially with some 6 weeks of traction.
Since the mid-1970s, the development of a variety of casting materials and the use of thermoplastics in brace construction have extended the ideas of these pioneers of the 1960s and 1970s to the point where functional bracing, certainly for shaft fractures of the tibia and certain lower femoral fractures, is accepted without question as the natural sequel to early management by plaster casting or traction. The widespread use of functional bracing has liberated countless patients from prolonged hospitalization and permitted early return to function and to gainful employment.
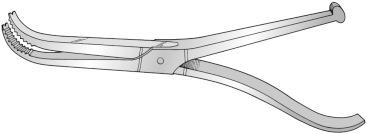
Until about 150 years ago, an open fracture was virtually synonymous with death and generally necessitated immediate amputation. Amputation itself carried with it a very high mortality rate, usually with death resulting from hemorrhage or sepsis. Until the 16th century, the traditional method of attempting to control the hemorrhage after amputation was cauterization of the wound, either with hot irons or by the application of boiling pitch. This in itself may well have caused tissue necrosis and encouraged infection and secondary hemorrhage. The famous French surgeon Ambroise Paré (1510 to 1590), who served as surgeon to the Court of Henry II and Catherine de Medici and is rightfully regarded as the father of military surgery, was in 1564 the first to describe the ligation of the bleeding vessels after amputation. He developed an instrument that he called the “crow's beak” (bec de corbin) for securing the vessels and pulling them out of the cut surface of the amputation stump in order to ligate them ( Fig. 74.10 ). Notwithstanding this advance, Le Petit, who in 1718 described the use of the tourniquet to control hemorrhage during amputation, is reputed to have claimed that his invention reduced the mortality rate from amputation of the lower limb from 75 percent to 25 percent.
In the history of the open fracture, Ambroise Paré features again in documenting for the first time the conservation of a limb after an open fracture. He in fact described his own injury, sustained on May 4, 1561, when, while crossing the Seine on a ferry to attend a patient in another part of Paris, his horse, startled by a sudden lurch of the vessel, gave him “such a kick that she completely broke the two bones of the leg four fingers above the junction of the foot.” Fearing that the horse would kick him again and not appreciating the nature of the injury, he took an instinctive step backward “but sudden falling to the earth, the fractured bones leapt outwards and ruptured the flesh, the stocking and the boot, from which I felt such pain that it was not possible for man (at least in my judgment) to endure any greater without death. My bones thus broken and my foot pointing the other way, I greatly feared that it would be necessary to cut my leg to save my life.” He then described how, with a combination of prayer, splintage, and dressing of the open wound with various astringents, coupled with the regular use of soap suppositories, he survived the initial infection and by September, “finally thanks to God, I was entirely healed without limping in any way,” returning to his work that month ( Fig. 74.11 ).
Nevertheless, in insisting on conservative management of his open fracture rather than amputation, Paré was flying in the face of orthodox surgical practice, as indeed was the English surgeon Percival Pott, who in 1756 was thrown from his horse while riding in Kent Street, Southwark, and suffered a compound fracture of the lower leg. Aware of the dangers of mishandling such an injury, he would not permit himself to be moved until he had summoned his own chairmen from Westminster to bring their poles, and it is said that while lying in the January cold awaiting them, he bargained for the purchase of a door, to which his servants subsequently nailed their poles and thereby carried him on a litter to Watling Street near St. Paul's cathedral. There he was attended by an Edward Nourse, a prominent contemporary surgeon, who expressed the view that because of the gentle handling of the limb, no air had entered the wound and therefore there was a chance of preserving the leg, which otherwise was destined for amputation. Finally, success attended a long period of immobilization and convalescence.
As late as the 19th century, not all victims of open fracture were so fortunate. Even in circumstances considered ideal at the time, the mortality rate associated with open injuries remained high. Billroth recorded four patients with compound dislocations of the ankle who came under his care in Zurich, with one dying of pyemia, one of septicemia, and a third of overwhelming infection after amputation for suppuration on the 36th day after injury. The fourth patient recovered. Of 93 patients with compound fractures of the lower leg whom he treated in Zurich, 46 died. Recovery from open fracture of the femur was, in Billroth's experience, so unusual that, describing the case of a woman of 23 who recovered from such an injury, he stated, “The following case of recovery is perhaps unique.”
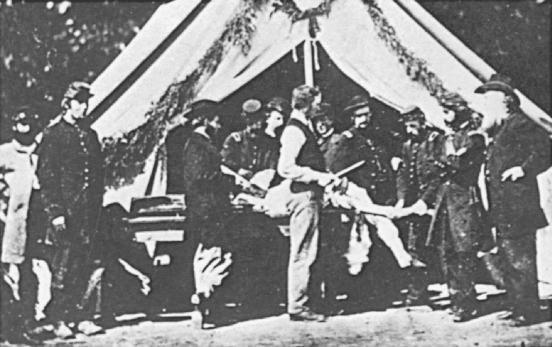
Gunshot wounds producing fracture were particularly notorious and generally treated with immediate amputation, certainly until the early part of the 20th century. The results of this policy, however, were in certain instances quite horrifying. Wrench recorded that in the Franco-Prussian War (1870–1871), the death rate from open fracture was 41 percent, and open fractures of the knee joint carried a 77 percent mortality rate. On the French side, of 13,172 amputees, some 10,006 died. On the other hand, in the American Civil War, the overall mortality rate for nearly 30,000 amputations was on the order of 26 percent, although for thigh amputations it reached 54 percent ( Fig. 74.12 ). The difference in the mortality rates for different theaters of war around that time was probably related to the postoperative management, as very often the suppurating amputation stump was sponged daily with a solution from the same “pus bucket” used for all the patients. It has been said of that era that it was probably safer to have your leg blown off by a cannonball than amputated by a surgeon!
During World War I, gunshot wounds of the femur carried a very high mortality rate in the early years. In 1916 the death rate from gunshot wound of the femur was 80 percent in the British army. Thereafter it became policy to use the Thomas splint, with fixed traction applied via a clove hitch around the booted foot, before transportation to the hospital. Robert Jones reported in 1925 that this simple change of policy resulted in a reduction of the mortality rate to 20 percent by 1918. With progressive understanding of bacterial contamination and cross-infection after the pioneering work of Pasteur, Koch, Lister, and Semmelweis; the use of early splintage, as learned by the British forces in World War I; and the application of open-wound treatment following wound extension and excision as advocated first by Paré and later by Larrey (Napoleon's surgeon and inventor of the ambulance ), the scourge of the open fracture, even from a femoral gunshot wound, has been greatly reduced.
It is generally believed that the earliest technique of internal fixation of fractures was that of ligature or wire suture and, according to Malgaigne, the first mention of the ligature dates back to the early 1770s. A. M. Icart, surgeon of the Hôtel Dieu at Castres, claimed to have seen it used with success by Lapujode and Sicre, surgeons of Toulouse. This observation came to light when, in 1775, M. Pujol accused Icart of bringing about the death of a young man with an open fracture of the humerus in whom Icart was alleged to have performed bone ligature using brass wire. In his defense, Icart cited the experience of the Toulouse surgeons in the earlier part of the decade, although denying that he himself had personally used this technique in the case in dispute. In a scholarly discussion of Pujol versus Icart, Evans has called into question whether this type of operation was any more than the subject of surgical theory at that time, but Icart's contention was widely accepted by so many French observers in the 19th century that it is highly probable that bone ligature was performed at least by Lapujode (if not Sicre) around 1770.
On July 31, 1827, Dr. Kearny Rodgers of New York is recorded as having performed bone suture. He resected a pseudarthrosis of the humerus and, finding the bone ends to be most unstable, drilled a hole in each and passed a silver wire through to retain coaption of the bone fragments. The ends of the wire were drawn out through a cannula that remained in the wound. Although on the 16th day the cannula fell from the wound with the entire wire loop, the bones remained in their proper position and union was said to have occurred by 69 days after the operation. The patient was not allowed to leave his bed for 2 months after the operation!
In the introduction to his Traité de l'Immobilisation Directe des Fragments Osseux dans les Fractures (the first book ever published on internal fixation), Bérenger Féraud recounted that, at the beginning of his medical career when he was an intern at the Hôtel Dieu Saint Esprit at Toulon in 1851, he was involved in the treatment of an unfortunate workman who had sustained a closed, comminuted fracture of the lower leg in falling down a staircase. Initial splintage was followed by a period of infection and suppuration, requiring several drainage procedures; eventually, after many long weeks, amputation was decided on. At the last moment, the poor patient begged to be spared the loss of his leg, so Dr. Long, Bérenger Féraud's chief, exposed the bone ends, freshened them, and held them together with three lead wire ligatures (cerclage) “as one would reunite the ends of a broken stick, and to our great astonishment then guided the patient to perfect cure without limp or shortening of the member, which for so long had appeared to be irrevocably lost.” The patient survived, and the lead wires were removed 3 weeks later; the fracture united, and the workman left the hospital 105 days after his accident and resumed work 6 months after the operation. Bérenger Féraud went on to say:
I assisted at the operation and I bandaged with my own hands the injured for many long weeks. Can anyone understand how this extraordinary cure struck me? The strange means of producing and maintaining solid coaptation of the bony fragments by encircling them with a metallic ligature fascinated me as during my childhood I had heard tales of this technique being performed by Arab surgeons and, until then, had considered this to be a mere product of a barbaric empiricism. … In my childhood, in 1844 and 1845, I heard an old tebib renowned in the environs of Cherchell, in Algeria, for his erudition and his experience, recount to my father who, a surgeon impassioned with our art, avidly questioned native practitioners of French Africa, in order to sort out, from their experiences and their therapeutic means, the scientific principles, which had been passed down to them from their ancestors, amidst some of the ordinary practices of a more or less coarse empiricism. I tell you, I heard him say that in certain cases of gunshot wounds, or when a fracture had failed to unite, the ancient masters advised opening the fracture site with a cutting instrument, ligating the fragments one to another with lead or iron wire … and only to remove the wire once the fracture was consolidated.
It therefore seems that there is some anecdotal evidence to suggest that such techniques had been used in the early part of the 19th century or even before. Bérenger Féraud himself cited the example of Lapujode and Sicre mentioned earlier. Commeiras reported native Tahitian practitioners to be skilled in the open fixation of fractures using lengths of reed.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here