Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The development of contemporary corneal transplantation has been evolutionary and largely evidence-based over the past century.
The first successful, documented corneal graft was reported in 1906.
Ramon Castroviejo is recognized as the pioneer of modern keratoplasty, and R. Townley Paton is the father of eye banking.
Contemporary keratoplasty has moved away from penetrating keratoplasty and has focused on layer-specific transplantation contributing to a re-emergence of emphasis on layer-specific lamellar techniques.
An emerging understanding of ocular surface physiology and limbal stem cell deficiency has led to the development of a menu of ocular surface transplant procedures.
The next major advancement in keratoplasty will move toward cell-based therapy.
From the first documented successful corneal transplant performed by Eduard Konrad Zirm in 1906 to contemporary layer-specific lamellar surgery, the evolution of keratoplasty has been nothing short of remarkable. Some of the most talented ophthalmologists of our time have served as the inspiration for research and advancements in corneal transplantation. This chapter will outline the historical journey and landmark achievements that have marked the evolution of keratoplasty from penetrating keratoplasty to the varied array of technically diverse, innovative surgeries that we employ today.
Historically, recognition for the term “keratoplasty” has been attributed to Franz Reisinger, who first described the term in a publication in 1824. , Early concepts of corneal transplantation were further developed by Astley Cooper, Karl Himly, Gottlieb Mössner, Johannes Dieffenbach, and Samuel Bigger. The first recorded experiments were performed on rabbits, while later experimentation included rabbits, chickens, and doves, with varying degrees of success. In 1840, Michael Marcus outlined the first set of basic principles for keratoplasty surgery including the need for similar size and shape of the donor and recipient tissues, rapid transfer of donor tissue to host, attachment of donor tissue in an atraumatic fashion, and preservation of intraocular contents. , That same year, Franz Mühlbauer also described a technique for using a triangular-shaped lamellar graft to perform the first anterior lamellar keratoplasty.
For the most part, however, these early attempts at corneal grafting proved to be unsuccessful. As a result, in the ensuing decades, interest in keratoplasty declined, even while research was directed toward the development of the artificial cornea (keratoprosthesis). By the late 1800s, primarily due to the efforts of Arthur von Hippel promoting lamellar grafts and the design of a circular mechanical trephine, a resurgence of interest in corneal transplantation emerged. Dürr and Fox further stimulated interest by reporting their techniques for lamellar grafting. Dürr described a partial lamellar graft, which employed a triangular piece of peripheral cornea that still had a triangular conjunctival flap attached. Fox employed a lamellar technique in which a full-thickness rabbit cornea was placed into a prepared lamellar recipient bed. In 1878, G.F. Sellerbeck performed the first human corneal transplant using a simple manual trephine and stressed the importance of the presence of a healthy donor tissue, without a conjunctival flap. ,
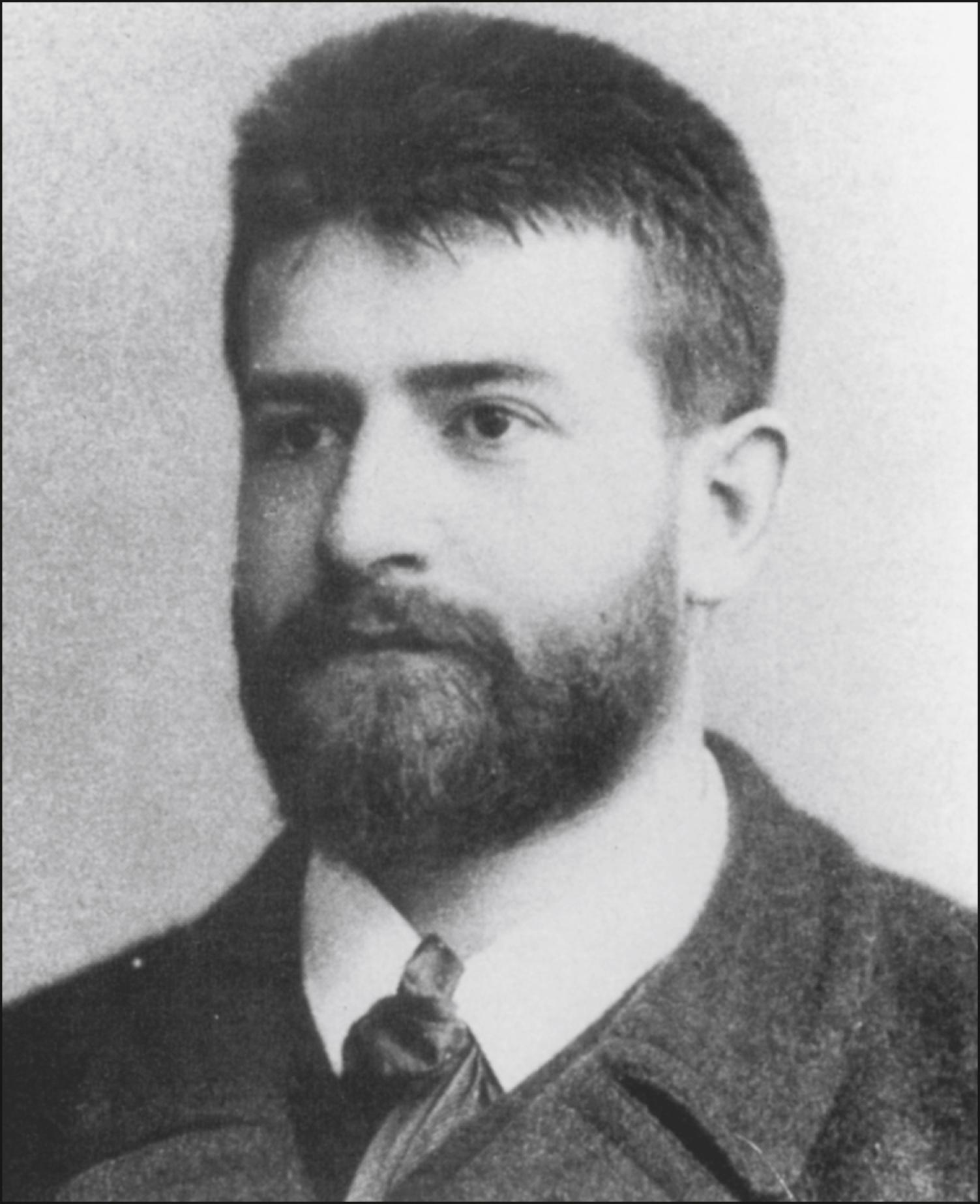
The procedure that instigated a sea-change in keratoplasty came from an unlikely source. Eduard Zirm ( Fig. 109.1 ) in Moravia performed the first documented successful human corneal transplant in 1906. , Ironically, he effectively performed the operation for one of the most difficult indications for successful grafting: bilateral alkali burns in a patient injured with unslaked lime. He used one donor tissue for both eyes from the enucleated eye of an 11-year-old boy. The donor grafts were removed using a 5-mm von Hippel trephine, and the grafts remained clear for at least 6.5 months. Based on this procedure, Zirm elaborated several fundamental principles of corneal transplant surgery including the exclusive use of healthy, human donor material; the employment of strict sterile technique; the protection of the graft with physiologic saline and avoidance of exposure to any toxic chemicals; the use of overlay sutures to secure the graft; and the careful selection of cases.
Although Zirm identified several of the fundamental principles of keratoplasty, it would take approximately 50 years and the significant effort and dedication of a number of skilled surgeons in the field to transform these early methods to the modern techniques of corneal transplantation. The work of Anton Elschnig, Tudor Thomas, Vladimir Filatov, Zdanko Nizetic, Joszef Imre Jr., Adolph Franceschetti, Hermenegildo Arruga, Walther Löhlein, Mauno Vannas, and Benjamin Rycroft, among others, all contributed to the evolution of modern techniques of penetrating keratoplasty through the development of new trephine models, techniques for fixation of the graft with direct appositional as opposed to overlay sutures, and expansion of the indications for keratoplasty. , However, it was the work of Ramon Castroviejo that had the most profound influence on modern-day corneal transplantation ( Fig. 109.2 ).
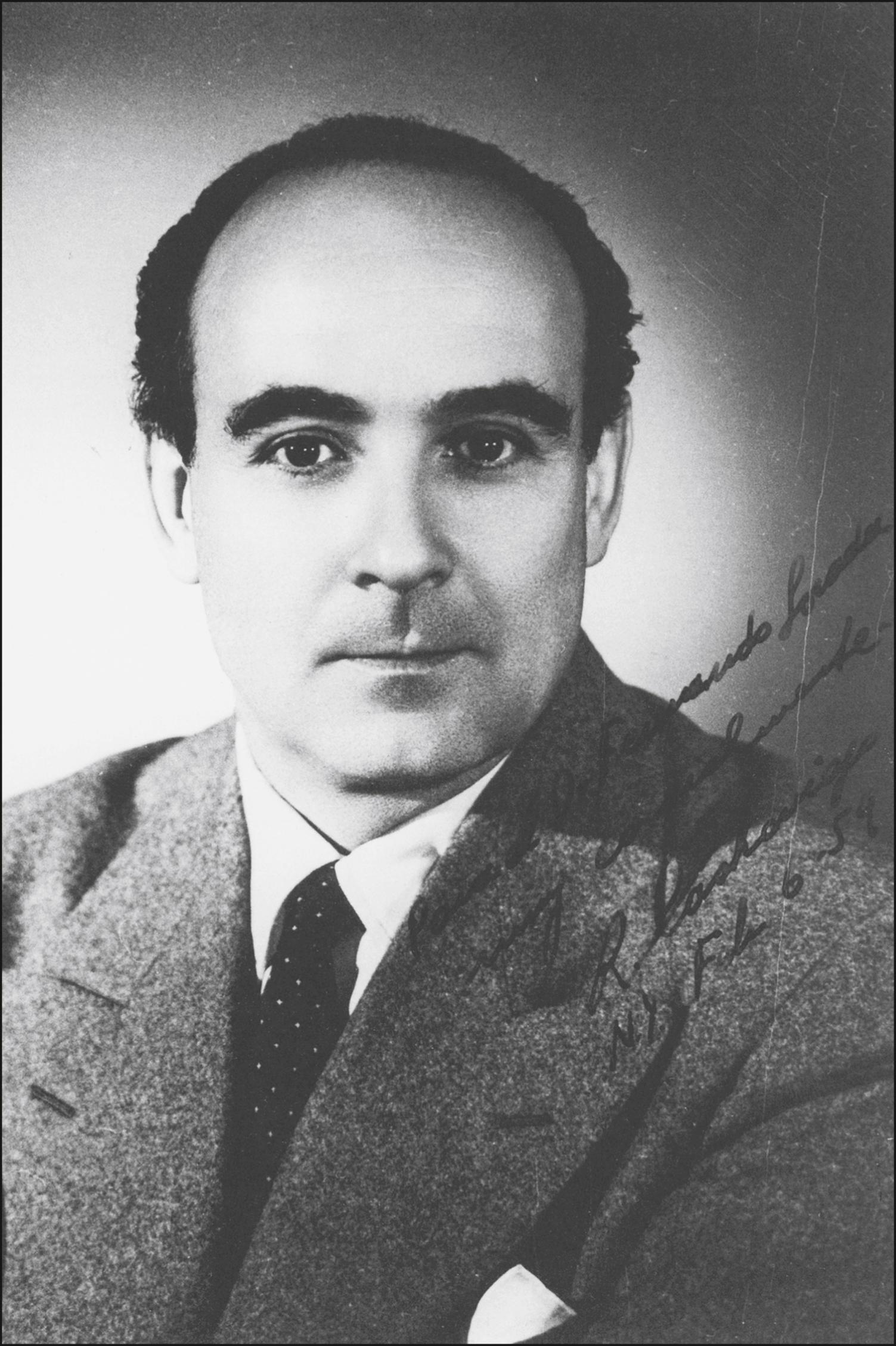
Castroviejo studied keratoplasty both clinically and in the research laboratory. He based the development of successful clinical techniques on studies of rabbits as well as on clinical series of keratoplasty in humans. , He refined his techniques and progressed from use of a square to a circular graft and converted from traditional overlay sutures to direct appositional suturing. Castroviejo also had a particular penchant and talent for the development of surgical instruments to assist in successful transplantation. Many of these instruments are still in widespread use today.
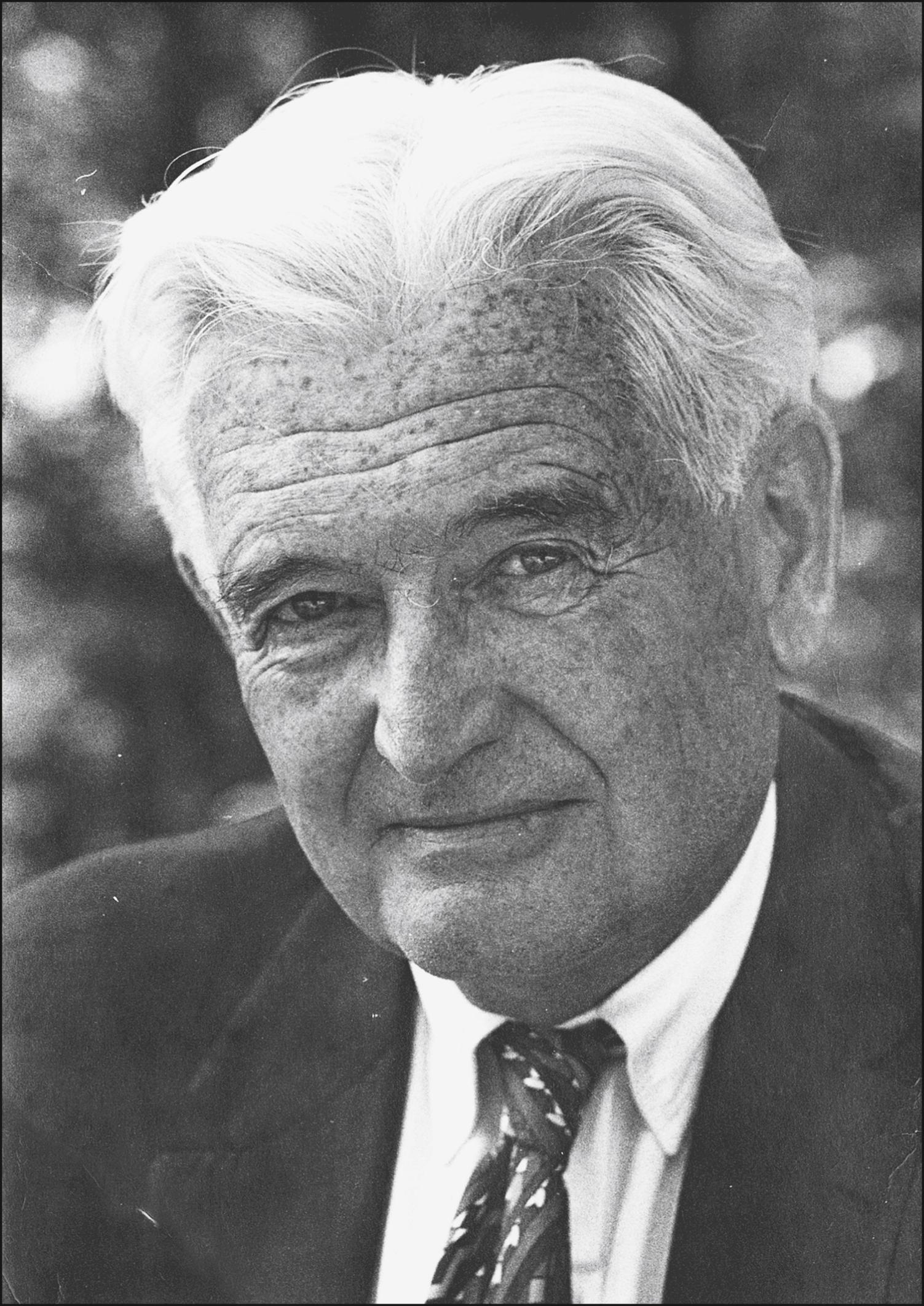
In addition to Castroviejo’s innovative techniques, other notable events that significantly contributed to modern-day keratoplasty included the development of the operating microscope and the availability of monofilament nylon microsuture materials. The establishment of the first eye bank by R. Townley Paton ( Fig. 109.3 ) in 1945 served as the cornerstone for the later development of a national eye banking movement, which allowed keratoplasty to be performed across the country. In San Francisco, the work of Max Fine led to the recognition that keratoplasty could be successfully performed for the treatment of aphakic bullous keratopathy. Further, the immunologic discoveries of A. Edward Maumenee and the simultaneous introduction of topical corticosteroids had a profound impact on the success of modern penetrating keratoplasty. ,
Nonetheless, even with the great successes of modern-day corneal transplantation, the procedure has continued to evolve. While penetrating keratoplasty remains one of the most common transplant procedures, over the past three decades, innovations in corneal transplantation surgery have resulted largely from the diversification and improvement of techniques in lamellar transplantation.
The concept of lamellar keratoplasty was developed in the late 19th century. In 1914, Anton Elsching, using the von Hippel trephine, reported the first successful lamellar keratoplasty in a case of interstitial keratitis. , His subsequent report of a series of 174 cases inspired others, such as Vladimir Filatov, to investigate further the advantages of partial-thickness keratoplasty. Lamellar keratoplasty continued to evolve in the early 20th century under the advances made by Barraquer, Filatov, Paufique, and others. However, lamellar techniques gave way to the growing popularity and success of penetrating keratoplasty in the second half of the 20th century, largely because of the persistent problems of interface haze, scarring, and epithelial ingrowth associated with lamellar procedures.
As technical and laboratory advancements in penetrating keratoplasty took place, the goals of surgery became not only successful transplantation but also optical performance: minimal astigmatism, improved predictability of corneal refractive power, ease of recovery, and decreased rates of rejection. Further, with increased understanding of pathophysiology came the realization that, in many cases, it might not be necessary to replace the entire cornea, but, in fact, it might be preferable to replace only the “diseased” portion, maintaining the integrity of the host cornea as much as possible in order to avoid the refractive and immune issues associated with penetrating grafts. These realizations, along with the well-documented risks of open-sky corneal transplantation, led to a resurgence of interest in revising the techniques of lamellar keratoplasty. Indeed, the most fascinating innovations of the past two decades have come from the evolution back to lamellar keratoplasty techniques.
Posterior lamellar keratoplasty (PLK) evolved into Descemet stripping automated endothelial keratoplasty (DSAEK) for endothelial disease. Deep anterior lamellar keratoplasty (DALK) is now the preferred surgery for corneal stromal disease with normal endothelium. And ocular surface transplantation techniques are the treatment of choice for isolated epithelial disease.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here