Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The conjunctival and limbal epithelia are derived from surface ectoderm.
The mucocutaneous junction at the lid margins is the junction between hydrophobic (unwettable) epidermis and hydrophilic (wettable) conjunctiva.
The corneoscleral limbus is a unique stem cell niche microenvironment that supports a population of pluripotent limbal stem cells.
Injury to the limbus and loss of limbal stem cells result in conjunctivalization of the cornea.
Conjunctival goblet cells secrete MUC5AC, the primary constituent of the tear mucin layer.
Conjunctival epithelial cells express membrane-bound mucins (MUC1, MUC4, MUC16), which confer wettability to the ocular surface.
The conjunctiva modulates the volume, osmolarity, and electrolyte concentration of the tear film.
The conjunctiva is a mucous membrane that is vital to the health of the ocular surface and the eye as a whole. It provides extensive coverage of the ocular surface from the upper and lower lid margins to the corneal limbus. The unique anatomy of the conjunctiva allows unrestricted movement of the eye and facilitates normal eyelid function. The conjunctiva also plays critical roles in the production of both the aqueous and mucous components of the tear film. It further plays a major role in ocular surface immunology as the main reservoir of ocular surface lymphoid tissue and other antimicrobial agents that protect the surface. The corneal limbus at the junction of the conjunctiva and cornea is a crucial and unique microenvironment that maintains the limbal stem cells that sustain the avascular corneal epithelium. Abnormalities of the conjunctiva and limbus may lead to restriction of ocular movement, lid malposition, deficiency of the tear film, decreased host resistance to ocular surface infection, and loss of corneal epithelial integrity and clarity.
The conjunctival epithelium is derived from surface ectoderm and becomes distinguishable from adjacent limbal-corneal epithelium as early as the seventh week of human fetal development. Outgrowth and apposition of the neural ectoderm–derived optic vesicle to the overlying surface ectoderm results in activation of PAX6 gene expression within the overlying surface ectoderm cells. This triggers elongation of the majority of the surface ectodermal cells within the apposition area, resulting in formation of a lens placode. The lens placode cells then invaginate and separate from the surface ectoderm to form the lens vesicle. The small cohort of residual nonelongated, PAX6 -expressing ectodermal cells on the embryonic surface in turn differentiate into conjunctival and limbal-corneal epithelium. The surrounding surface ectodermal cells that lack PAX6 expression continue through a default differentiation pathway to become the epidermis of the lids ( Fig. 2.1 ).
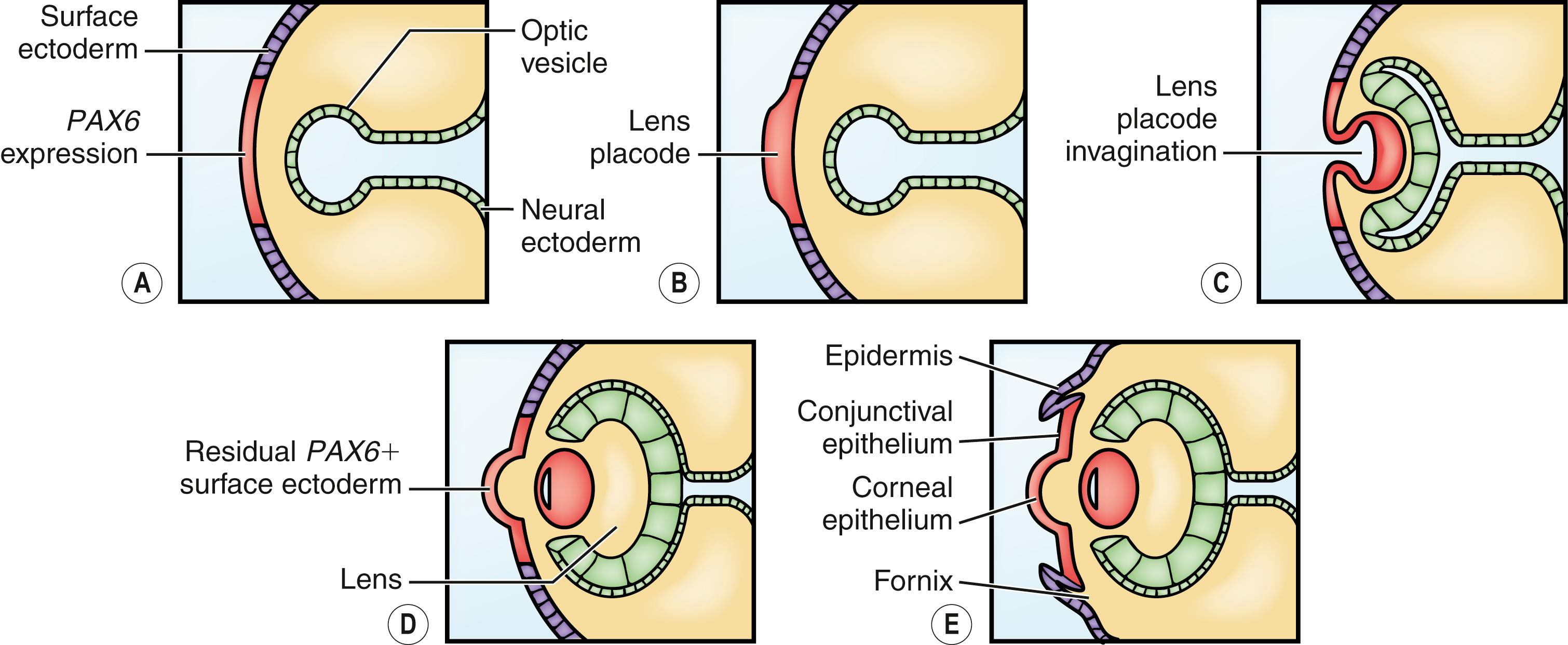
Limbal-corneal epithelium then undergoes a further, remarkable segregation of stem cells and early precursor cells to the anatomic limbus. Subsequent expression of putative stem cell markers such as ABCG2, ΔNp63α, and ABCB5 2 ; loss of gap junctions in the limbal-basal epithelium; and the expression of tissue-specific cytokeratins in corneal and conjunctival epithelium lead to phenotypically distinct corneal, limbal, and conjunctival epithelium.
At 8 weeks, the eyelids form from folds of the surface ectoderm and fuse together. The conjunctival epithelium develops within the lid folds from surface ectoderm along the posterior surface of the lids and around the developing cornea. Budding of the epithelium in the conjunctival fornices forms the lacrimal gland superotemporally and accessory lacrimal glands of Wolfring and Krause in the inferior and superior fornices (12 weeks). The caruncle arises as a sequestration of the medial lower eyelid and is not formed from the conjunctiva.
The conjunctiva extends from the mucocutaneous junction (MCJ) at the margin of the eyelids to the corneoscleral limbus. The conjunctiva covering the posterior surface of the eyelid is known as palpebral conjunctiva, and the conjunctiva covering the surface of the globe is known as bulbar conjunctiva. Redundant conjunctiva at the transition between the palpebral and bulbar conjunctiva forms the fornices superiorly, inferiorly, and temporally and an extendible plica medially. The redundancy of the conjunctiva in the fornices and at the plica allows for independent movement of the eye and eyelids.
The larger superior fornix is maintained by fine smooth muscle slips passing from the deep surface of the levator palpebrae muscle to insert into the conjunctiva. These effectively prevent the superior forniceal conjunctiva from prolapsing down and blocking vision during upward gaze. The temporal conjunctiva is attached by fine fibrous slips to the lateral rectus tendon, which maintains the position of the conjunctiva during horizontal gaze. A true fornix does not exist medially except in adduction. Instead, a crescent-shaped fold of conjunctiva known as the plica semilunaris is formed medially, with its free lateral border lying 3–6 mm temporal to the caruncle when the eye is in primary position. Fine fibrous strips from the medial rectus tendon insert deep into the plica and caruncle. With contraction of the medial rectus and adduction of the eye, these slips tighten and form a medial cul-de-sac, approximately 2–3 mm in depth.
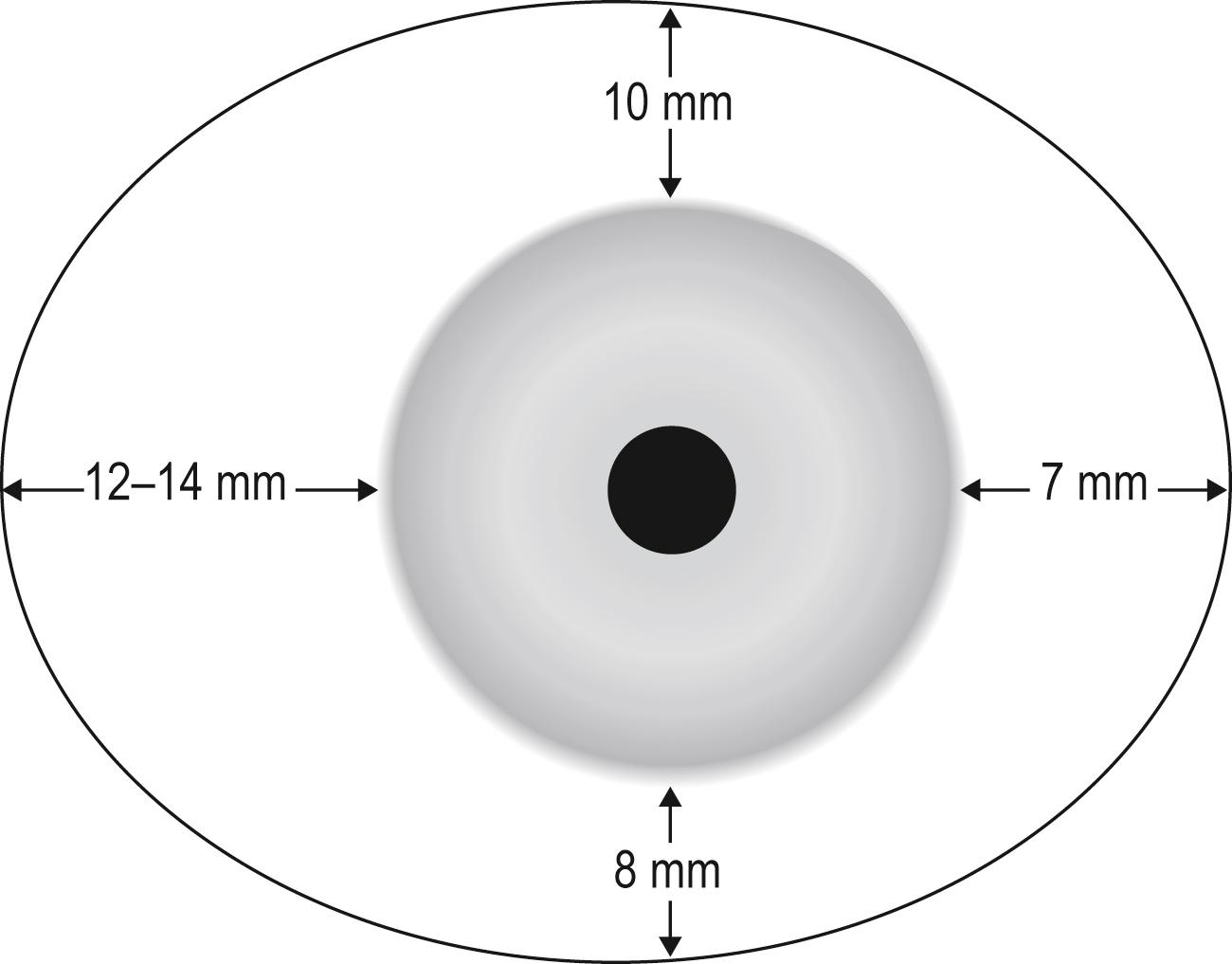
The mean total surface area for the adult conjunctival sac, including the cornea, is 16 cm 2 per eye ( Fig. 2.2 ). The epithelium contains goblet cells, Langerhans cells, and dendritic melanocytes. The substantia propria, or conjunctival stroma, is highly vascularized and may contain nonstriated muscle, sympathetic nerves, cartilage, and fatty tissue.
The caruncle measures 4–5 mm horizontally and 3–4 mm vertically and is located at the most medial aspect of the interpalpebral fissure. The caruncle is composed of pilosebaceous units, accessory lacrimal gland tissue, fibrofatty tissue, occasional smooth muscle fibers, and eccrine glands. Deep to the caruncle there may be several large sebaceous glands without cilia, similar to meibomian glands, which open onto the surface.
The MCJ is the transition from the keratinized skin of the eyelid margin to the nonkeratinized skin of the palpebral conjunctiva. Physiologically, this also correlates with the transition from the hydrophobic (unwettable), air-exposed cutaneous surface of the lid to hydrophilic (wettable), fluid-covered conjunctival mucous membrane. The MCJ also demarcates and defines the anterior apex of the tear meniscus, which terminates at the unwettable eyelid skin. The MCJ is not stationary but rather can move depending on the position of the tear film meniscus. Nasally, the MCJ runs anterior to the lacrimal puncta, which ensures that the puncta remain bathed within the tear meniscus. Just posterior to the MCJ, a physiologic line of vital-dye (lissamine green or rose Bengal) stainable conjunctival epithelium known as the Marx line is found along the upper and lower margins in normal subjects of all ages. Anterior displacement of the MCJ and widening of the Marx line can occur with natural aging or dry eye conditions. Posterior displacement of the MCJ can occur in cases of conjunctival cicatrization.
Just anterior to the MCJ lie the meibomian gland orifices of the upper and lower lids. Their location anterior to the MCJ ensures that lipid excreted from the meibomian glands can pool as a reservoir on the hydrophobic skin surface of the eyelid margin before being spread over the ocular surface during a blink. Meibomian glands of the eyelid are seen easily through the transparent palpebral conjunctiva as yellow lobulated structures separated by vascular arcades in the tarsus of the upper and lower eyelids running perpendicular to the eyelid margin.
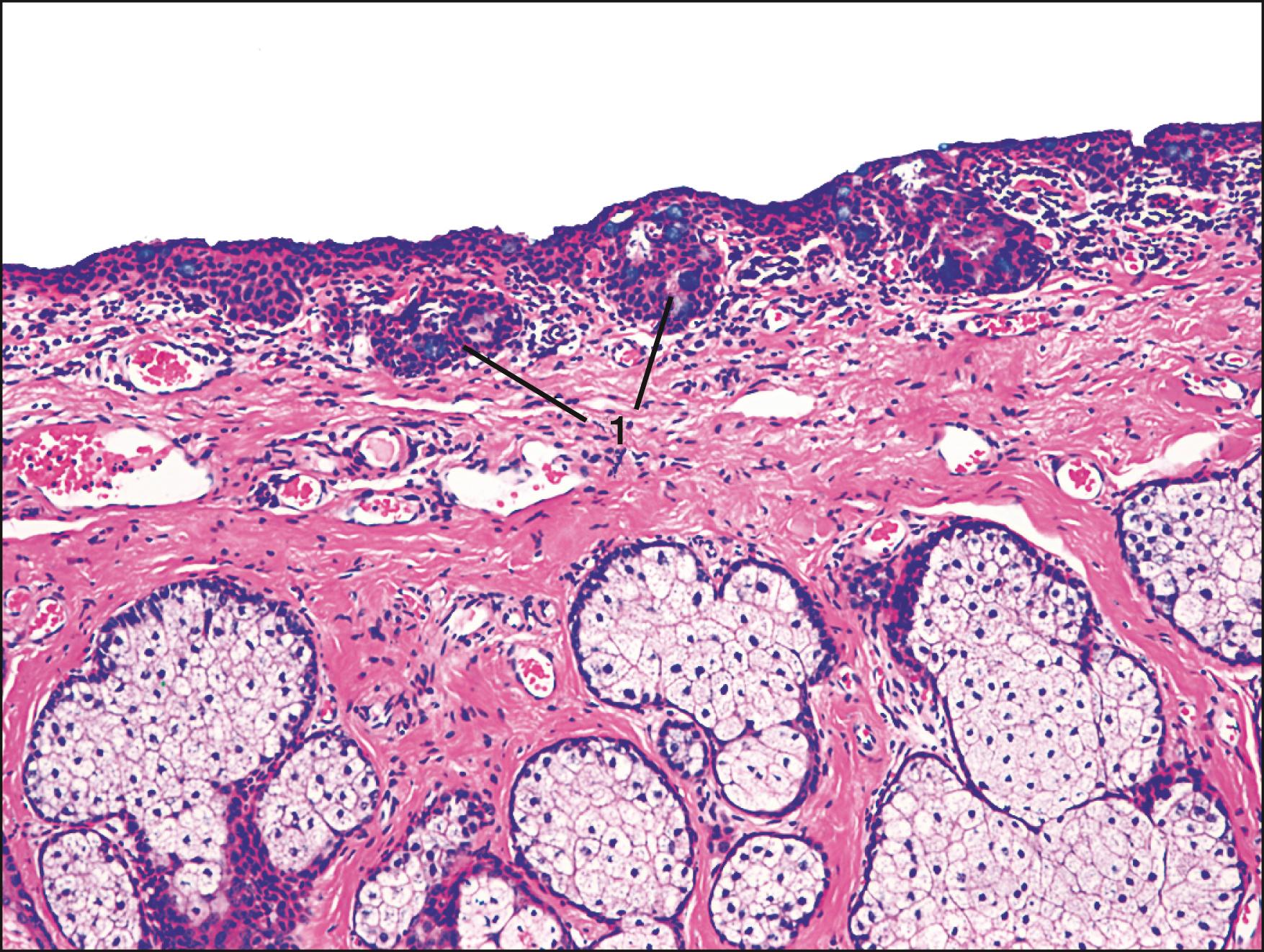
The tarsal conjunctiva is tightly adherent to the substance of the tarsus in order to present a smooth surface to interface with the anterior corneal surface. Consequently, there is no readily accessible subconjunctival tissue plane for dissection of the tarsal conjunctiva. Along the tarsal surface, 2 mm posterior to the lid margin, lies a shallow subtarsal groove less than 1 mm deep that runs parallel to the eyelid margin for most of the length of the tarsus. Between the eyelid margin and the tarsal groove are multiple ridges and grooves that communicate with goblet cell–lined invaginations of the conjunctival epithelium (the pseudocrypts of Henle) ( Fig. 2.3 ). Few crypts are present at birth; most develop at puberty. By age 50 years the crypts are found in approximately one-third of specimens. The crypts are more numerous in the nasal conjunctiva and around the plica. Accessory lacrimal glands are located in the forniceal conjunctiva (glands of Krause) and in the palpebral conjunctiva above or within the tarsus (glands of Wolfring) ( Fig. 2.4 ).
The bulbar conjunctiva is smoother and more loosely adherent to underlying tissues than the tarsal conjunctiva. Near the limbus, the bulbar conjunctiva blends with the underlying Tenon capsule and episclera. At the corneoscleral limbus there is a series of fibrovascular ridges perpendicular to the corneal margin (palisades of Vogt) that are more prominent superiorly and inferiorly and contain limbal epithelial stem cells.
The conjunctival surface is composed of two layers, the stratified epithelial layer and its underlying stroma (substantia propria). The stratified nonkeratinizing epithelium varies in thickness and appearance from the eyelid margin to the limbus. Unlike any other stratified squamous epithelium, goblet cells are dispersed among and attached to neighboring epithelial cells within the conjunctiva.
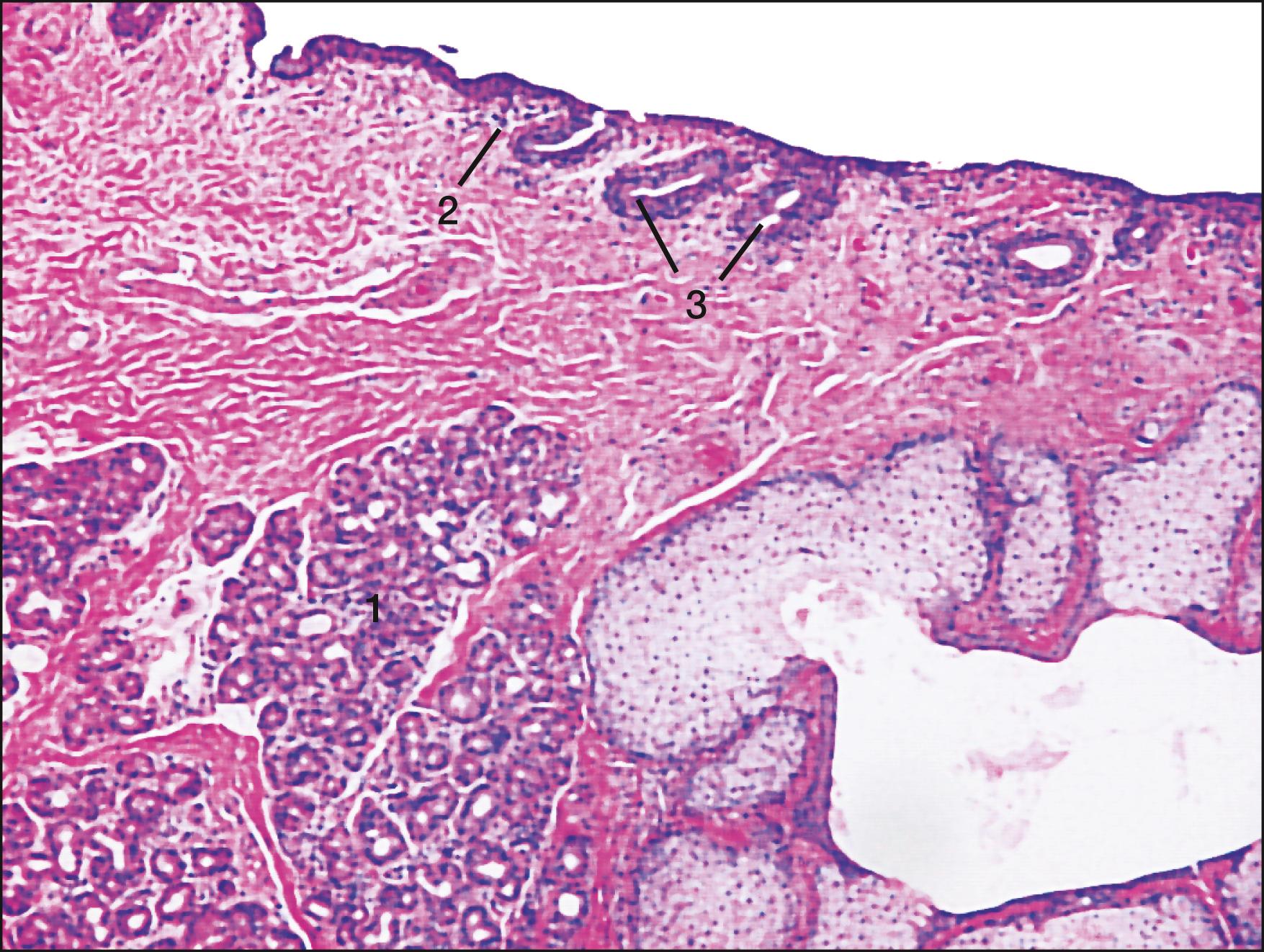
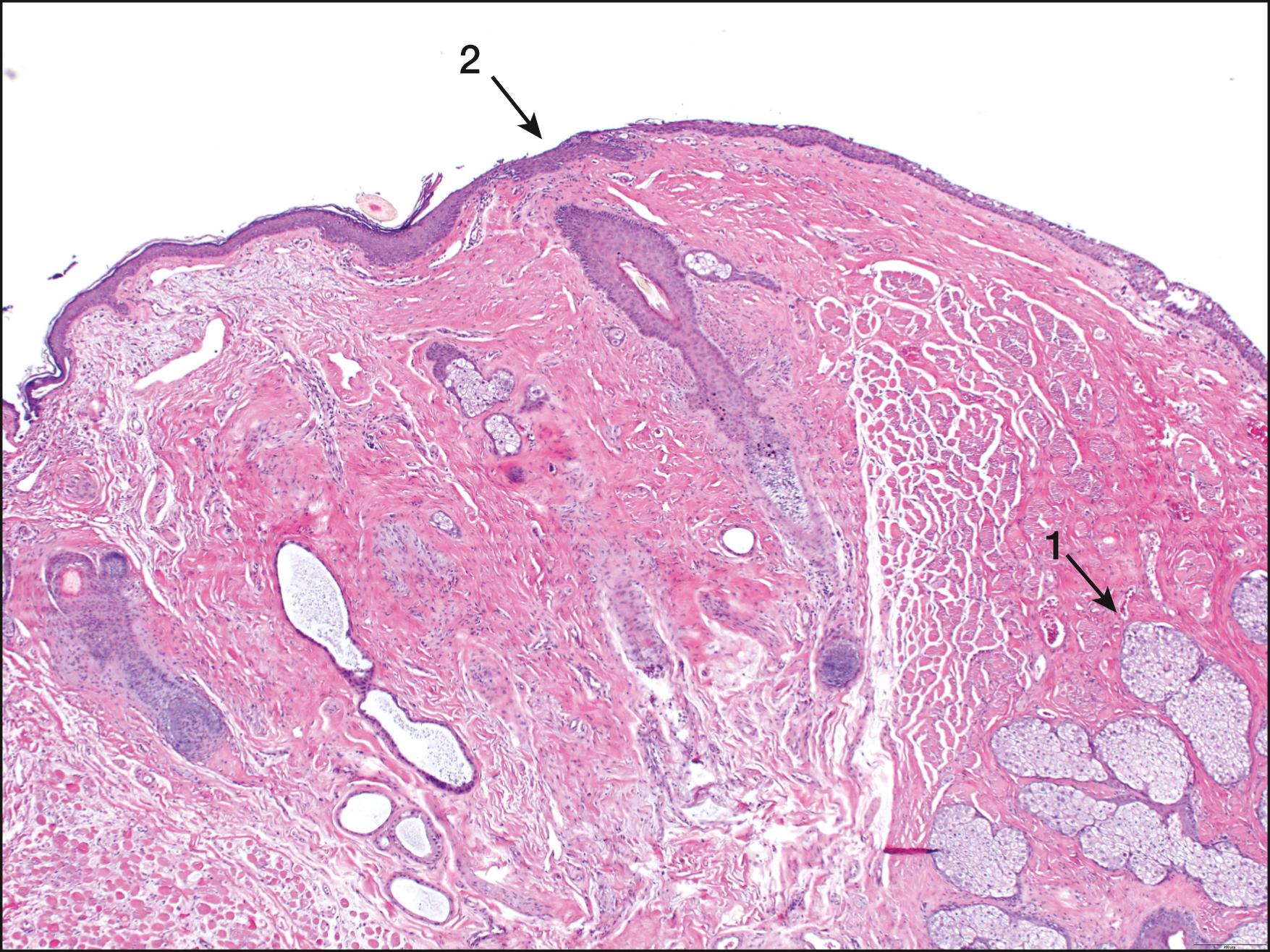
At the MCJ of the eyelid margin, there is an abrupt transition from the keratinized, stratified squamous epithelium of the eyelid skin to the nonkeratinized, stratified squamous epithelium of the marginal conjunctiva. The marginal conjunctiva then extends posteriorly for approximately 2 mm around the crest of the posterior lid margin before terminating at the subtarsal fold. Here, the stratified squamous, nonkeratinized epithelium transitions into the columnar/cuboidal epithelium characteristic of the palpebral conjunctiva overlying the tarsus ( Fig. 2.5 ).
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here