Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
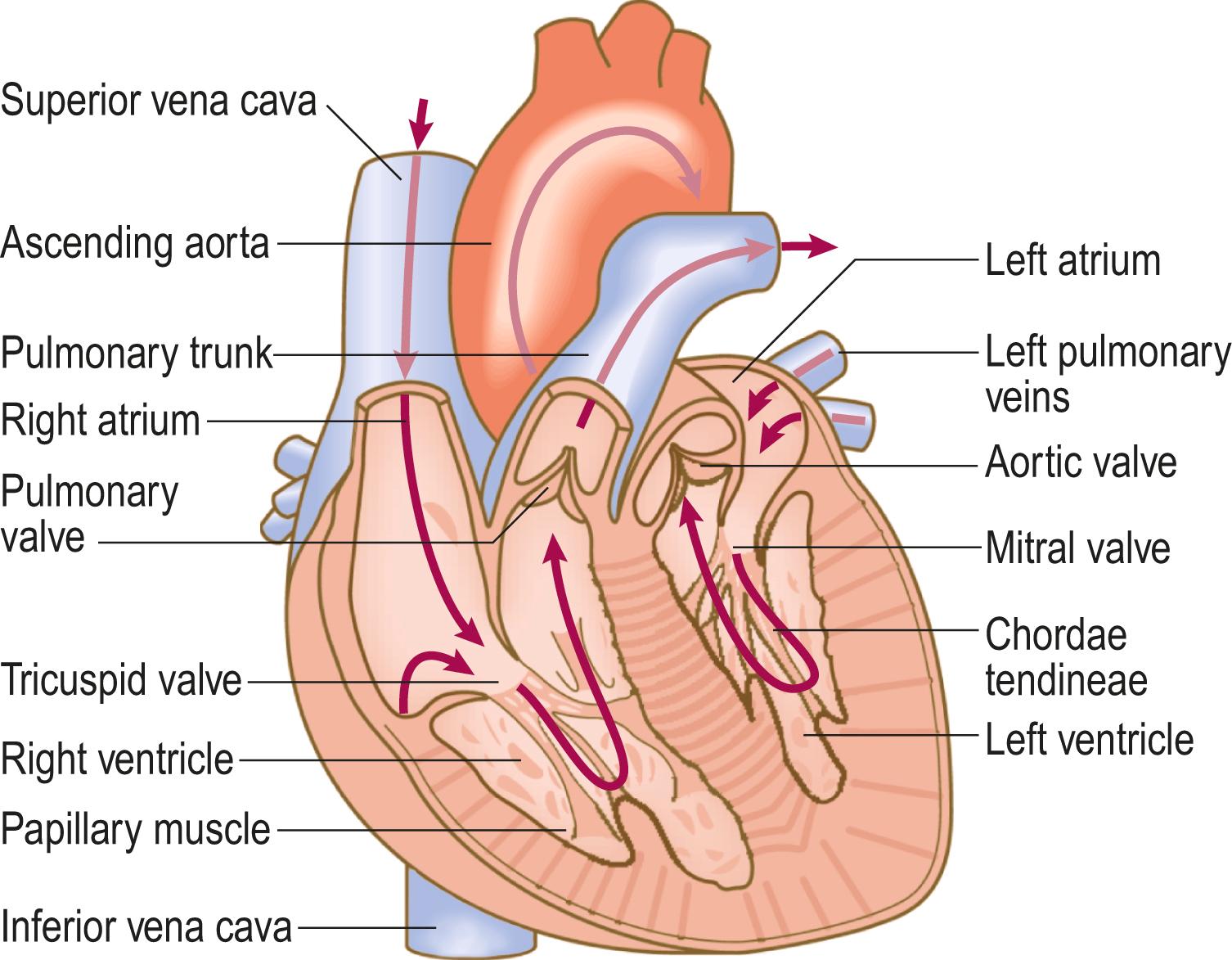
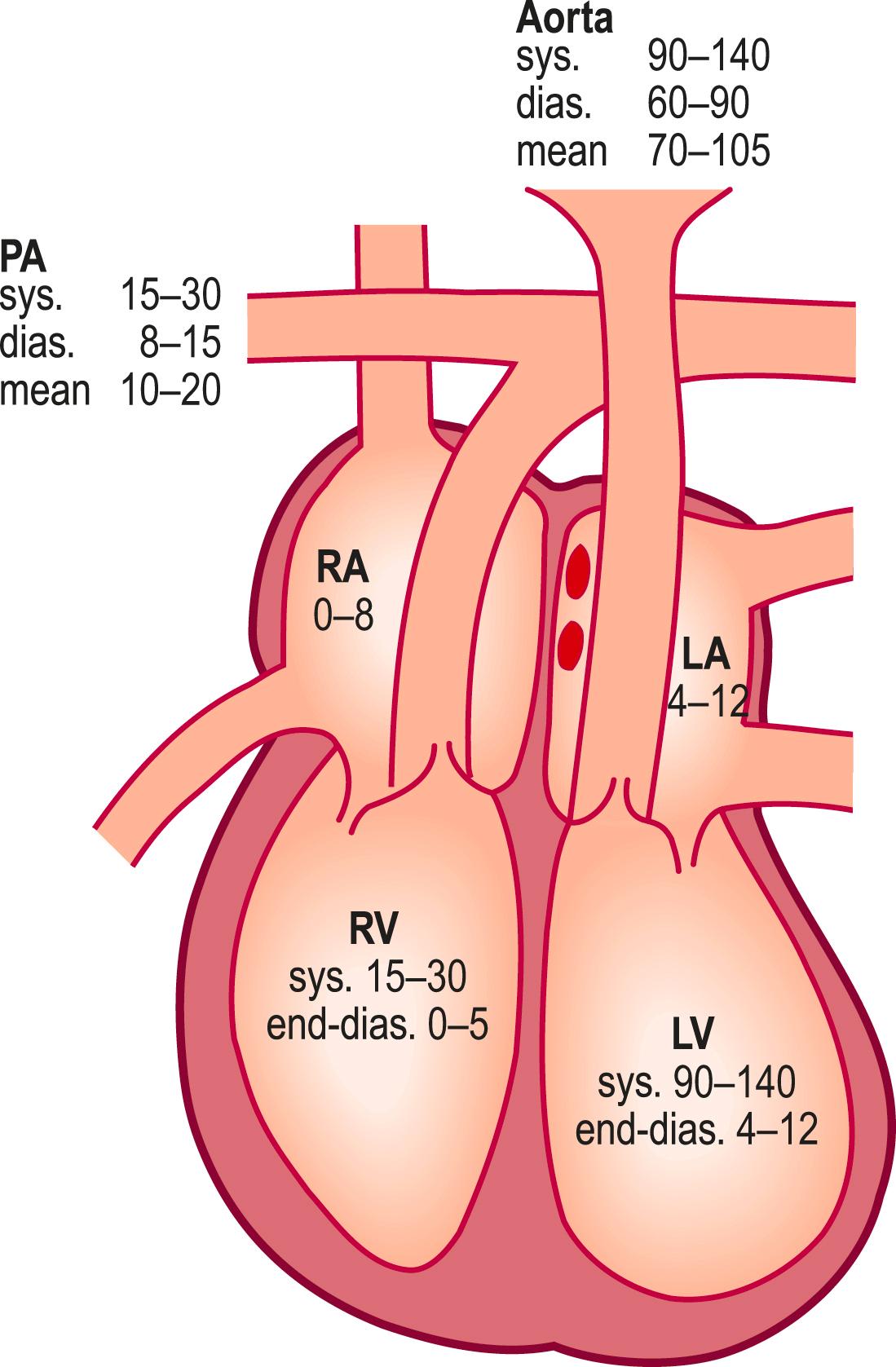
The heart comprises two muscular pumps working in a series, covered in a serous sac (pericardium) that allows free movement with each heart beat and respiration ( Fig. 4.1 ). The right heart (right atrium and ventricle) pumps deoxygenated blood returning from the systemic veins into the pulmonary circulation at relatively low pressures. The left heart (left atrium and ventricle) receives blood from the lungs and pumps it round the body to the tissues at higher pressures ( Fig. 4.2 ). Atrioventricular valves (tricuspid on the right side, mitral on the left) separate the atria from the ventricles. The pulmonary valve on the right side of the heart and the aortic valve on the left separate the ventricles from the pulmonary and systemic arterial systems, respectively. Cardiac contraction is coordinated by specialised groups of cells. The cells in the sinoatrial node normally act as the cardiac pacemaker. Subsequent spread of impulses through the heart ensures that atrial contraction is complete before ventricular contraction (systole) begins. At the end of systole the ventricles relax and the atrioventricular valves open, allowing them to refill with blood from the atria (diastole).
Cardiovascular disease may present with a number of diverse symptoms; non-cardiac causes must also be considered ( Box 4.1 ).
| Symptom | Cardiovascular causes | Other causes |
|---|---|---|
| Chest discomfort | Myocardial infarction Angina Pericarditis Aortic dissection |
Oesophageal spasm Pneumothorax Musculoskeletal pain |
| Breathlessness | Heart failure Valvular disease Angina Pulmonary embolism Pulmonary hypertension |
Respiratory disease Anaemia Obesity Anxiety |
| Palpitation | Tachyarrhythmias Ectopic beats |
Anxiety Hyperthyroidism Drugs |
| Syncope/presyncope | Arrhythmias Postural hypotension Aortic stenosis Hypertrophic cardiomyopathy Atrial myxoma |
Simple faints Epilepsy Anxiety |
| Oedema | Heart failure Constrictive pericarditis Venous stasis Lymphoedema |
Nephrotic syndrome Liver disease Drugs Immobility |
Chest pain due to intermittent myocardial ischaemia (angina pectoris) is typically a dull discomfort, often described as a tight or pressing ‘band-like’ sensation akin to a heavy weight. It tends to be felt diffusely across the anterior chest and may radiate down one or both arms and into the throat, jaw or teeth. In stable angina (caused by chronic narrowing in one or more coronary arteries), episodes of pain are precipitated by exertion and may occur more readily when walking in cold or windy weather, after a large meal or while carrying a heavy load; the pain is promptly relieved by rest and/or sublingual glyceryl nitrate (GTN) spray, and typically lasts for less than 10 minutes. The degree of physical exertion required to precipitate symptoms is a better guide to disease severity than the intensity of discomfort ( Box 4.2 ). Chest pain can be classified into typical angina, atypical angina and non-anginal chest pain ( Box 4.3 ). A history of typical angina significantly increases the likelihood of obstructive coronary heart disease. In unstable angina (caused by a sudden severe narrowing in a coronary artery), there is usually an abrupt onset or a worsening of chest pain episode that may occur on minimal exertion or at rest. It may be difficult to distinguish between angina and non-cardiac causes of episodic chest pain, such as oesophageal pain or musculoskeletal problems ( Box 4.4 ). The latter may occur at any site over the chest, often vary with posture or specific movements (such as twisting or turning) and may be associated with tenderness to palpation.
| Grade | Description |
|---|---|
| 1 | Ordinary physical activity, such as walking and climbing stairs, does not cause angina. Angina with strenuous, rapid or prolonged exertion at work or during recreation |
| 2 | Slight limitation of ordinary activity. Walking or climbing stairs rapidly, walking uphill, walking or climbing stairs after meals, in cold, in wind, or when under emotional stress, or only during the few hours after awakening |
| 3 | Marked limitation of ordinary physical activity. Walking one to two blocks on the level and climbing less than one flight in normal conditions |
| 4 | Inability to carry on any physical activity without discomfort; angina may be present at rest |
| Type | Characteristics | Likelihood of obstructive coronary heart disease |
|---|---|---|
| Typical angina | Meets all three of the following characteristics:
|
++++ |
| Atypical angina | Meets two of these characteristics. | ++ |
| Non-anginal chest pain | Meets only one or none of the characteristics. | – |
| Angina | Myocardial infarction | Aortic dissection | Pericardial pain | Oesophageal pain | |
|---|---|---|---|---|---|
| S ite | Retrosternal | Retrosternal | Interscapular/retrosternal | Retrosternal or left-sided | Retrosternal or epigastric |
| O nset | Progressive increase in intensity over 1–2 minutes | Rapid over a few minutes | Very sudden | Gradual; postural change may suddenly aggravate | Over 1–2 minutes; can be sudden (spasm) |
| C haracter | Constricting, heavy | Constricting, heavy | Tearing or ripping | Sharp, ‘stabbing’, pleuritic | Gripping, tight or burning |
| R adiation | Sometimes arm(s), neck epigastrium | Often to arm(s), neck, jaw sometimes epigastrium | Back, between shoulders | Left shoulder or back | Often to back sometimes to arms |
| A ssociated features | Breathlessness | Sweating, nausea, vomiting, breathlessness, feeling of impending death (angor animi) | Sweating, syncope, focal neurological signs, signs of limb ischaemia, mesenteric ischaemia | Flu-like prodrome, breathlessness, fever | Heartburn, acid reflux |
| T iming | Intermittent, with episodes lasting 2–10 minutes | Acute presentation; prolonged duration | Acute presentation; prolonged duration | Acute presentation; variable duration | Intermittent, often at night-time; variable duration |
| E xacerbating/relieving factors | Triggered by emotion, exertion, especially if cold, windy Relieved by rest, nitrates | ‘Stress’ and exercise are rare triggers, usually spontaneous Not relieved by rest or nitrates | SpontaneousNo manoeuvres relieve pain | Sitting up/lying down may affect intensity NSAIDs help | Lying flat/some foods may trigger Not relieved by rest; nitrates sometimes relieve |
| S everity | Mild to moderate | Usually severe | Very severe | Can be severe | Usually mild but oesophageal spasm can mimic myocardial infarction |
| Cause | Coronary atherosclerosis, aortic stenosis, hypertrophic cardiomyopathy | Plaque rupture and coronary artery occlusion | Thoracic aortic dissection rupture | Pericarditis (usually viral, also post myocardial infarction) | Oesophageal spasm, reflux, hiatus hernia |
Ask about:
site, onset, severity and character of the pain, and whether the pain radiates anywhere
associated symptoms such as breathlessness
aggravating and relieving factors, especially their relationship to exertion
frequency and duration of symptoms, and any recent change in pattern
degree of limitation caused by symptoms.
Myocardial infarction causes symptoms that are similar to, but more severe and prolonged than, those of angina pectoris. Associated features include restlessness, breathlessness and a feeling of impending death ( angor animi ). Radiation to one or both arms/shoulders, an association with exertion, sweating, nausea or vomiting and similarity to previous myocardial infarction all increase the likelihood of acute myocardial infarction. Pain that is pleuritic, positional, sharp, or reproduced with palpation is unlikely to be due to myocardial infarction.
Pericardial pain is typically a constant anterior central chest pain that may radiate to the shoulders. It tends to be sharp or stabbing in character, exacerbated by inspiration or lying down, and relieved by sitting forwards. It is caused by inflammation of the pericardium secondary to viral infection, connective tissue disease or myocardial infarction, or after surgery, catheter ablation or radiotherapy.
Aortic dissection (a tear in the intima of the thoracic aorta) is a life-threatening condition which is often missed. It is associated with abrupt onset of very severe, tearing chest pain that can radiate to the back (typically the interscapular region) and may be associated with profound autonomic stimulation. Over 90% of patients report the pain as severe or their ‘worst ever’, and the onset is sudden in 85% of cases; the absence of abrupt onset makes the diagnosis less likely. If the tear involves the cranial or upper limb arteries, there may be associated syncope, stroke or upper limb pulse asymmetry. Predisposing factors include connective tissue disorders, such as Marfan’s syndrome (see Fig. 3.21A–D ), family history of aortic disease, known aortic valve disease, previous aortic manipulation and known thoracic aortic aneurysm.
As with intermittent chest pain, explore the characteristics of the pain, and ask specifically about associated symptoms that may guide you to a likely diagnosis, such as interscapular pain, sweating, nausea, vomiting, syncope or neurological features (see Box 4.4 ).
Heart failure is the most common cardiovascular cause of both acute and chronic dyspnoea ( Box 4.5 ). Other cardiovascular causes of acute breathlessness include valvular heart disease, pulmonary embolism and arrhythmia, whilst non-cardiac dyspnoea may be due to pulmonary disease, obesity, anaemia, neuromuscular disease, chest wall disorders, pregnancy, hyperventilation syndrome and anxiety disorders.
| Mechanism | Cause |
|---|---|
| Reduced ventricular contractility (systolic dysfunction) | Myocardial infarction Dilated cardiomyopathy, e.g. genetic, idiopathic, alcohol excess, cytotoxic drugs, peripartum cardiomyopathy Myocarditis |
| Impaired ventricular filling (diastolic dysfunction) | Left ventricular hypertrophy Constrictive pericarditis Hypertrophic or restrictive cardiomyopathy |
| Increased metabolic and cardiac demand (rare) | Thyrotoxicosis Arteriovenous fistulae Paget’s disease |
| Valvular or congenital lesions | Mitral and/or aortic valve disease Tricuspid and/or pulmonary valve disease (rare) Ventricular septal defect Patent ductus arteriosus |
Patients with acute heart failure and pulmonary oedema (accumulation of fluid in the alveoli) usually prefer to be upright, while patients with massive pulmonary embolism are often more comfortable lying flat and may faint (syncope) if made to sit upright.
Exertional dyspnoea is the symptomatic hallmark of chronic heart failure. The New York Heart Association grading system is used to assess the degree of symptomatic limitation caused by the exertional breathlessness of heart failure ( Box 4.6 ). Dyspnoea caused by myocardial ischaemia is known as ‘angina equivalent’. It may occur instead of, or with, chest discomfort, especially in patients who are elderly or who have diabetes. It has identical precipitants to angina and may be relieved by GTN.
| Class | Description |
|---|---|
| I | No limitations. Ordinary physical activity does not cause undue fatigue, dyspnoea or palpitation (asymptomatic left ventricular dysfunction) |
| II | Slight limitation of physical activity. Such patients are comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnoea or angina pectoris (symptomatically ‘mild’ heart failure) |
| III | Marked limitation of physical activity. Less than ordinary physical activity will lead to symptoms (symptomatically ‘moderate’ heart failure) |
| IV | Symptoms of congestive heart failure are present, even at rest. With any physical activity, increased discomfort is experienced (symptomatically ‘severe’ heart failure) |
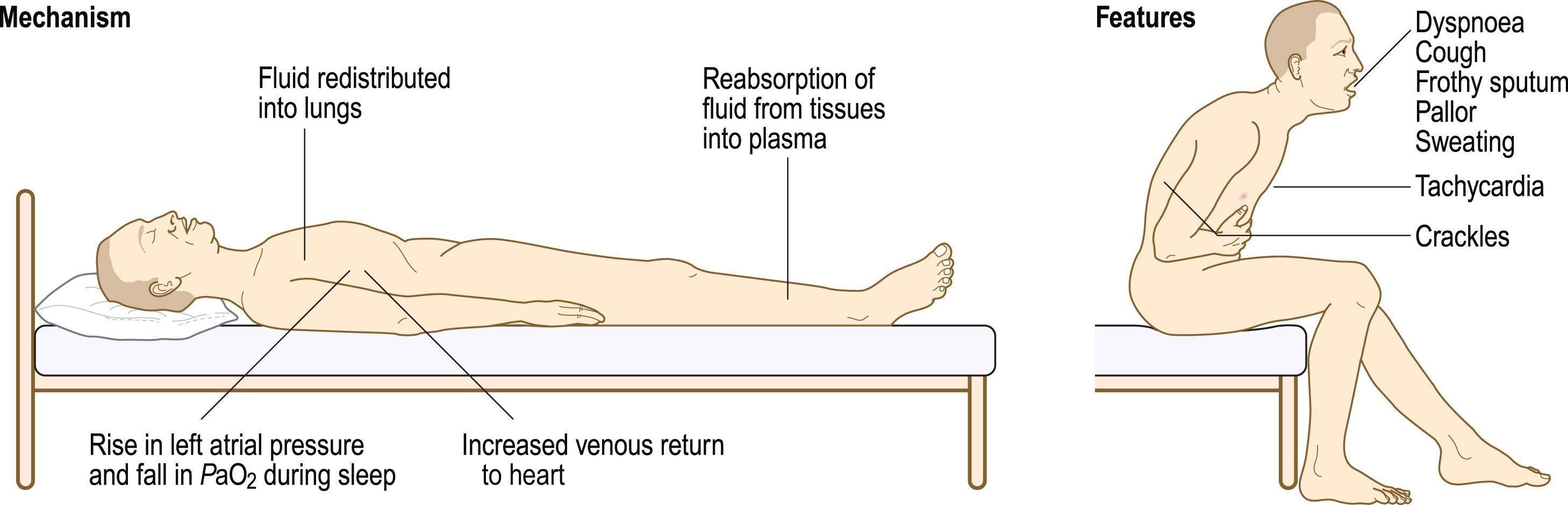
Orthopnoea, dyspnoea on lying flat, may occur in patients with heart failure, where it signifies advanced disease or incipient decompensation. Lying flat increases venous return and in patients with left ventricular impairment may precipitate pulmonary oedema. The severity can be graded by the number of pillows used at night: ‘three-pillow orthopnoea’, for example. Paroxysmal nocturnal dyspnoea is caused by the same mechanism, resulting in sudden breathlessness that wakes the patient from sleep ( Fig. 4.3 ). Patients may choke or gasp for air, sit on the edge of the bed and open windows in an attempt to relieve their distress. It may be confused with asthma, which can also cause night-time dyspnoea, chest tightness, cough and wheeze, but patients with heart failure may also produce frothy white or blood-stained sputum.
Bendopnoea is a symptom of dyspnoea when bending forward at the waist and is associated with increased cardiac filling pressures. Whilst common (18–49%) in patients with heart failure, it is not diagnostic and may occur in other conditions.
In acute dyspnoea, ask about:
duration of onset
background symptoms of exertional dyspnoea and usual exercise tolerance
associated symptoms: chest pain, syncope, palpitation or respiratory symptoms (such as cough, sputum, wheeze or haemoptysis; p. 87).
In patients with chronic symptoms, ask about:
relationship between symptoms and exertion
degree of limitation caused by symptoms and their impact on everyday activities
effect of posture on symptoms and/or episodes of nocturnal breathlessness
associated symptoms: ankle swelling, cough, wheeze or sputum.
Palpitation is an unexpected or unpleasant awareness of the heart beating in the chest. Detailed history-taking can help to distinguish the different types of palpitation ( Box 4.7 ).
| Extrasystoles | Sinus tachycardia | Supraventricular tachycardia | Atrial fibrillation | Ventricular tachycardia | |
|---|---|---|---|---|---|
| S ite | – | – | – | – | – |
| O nset | Sudden | Gradual | Sudden, with ‘jump’ | Sudden | Sudden |
| C haracter | ‘Jump’, missed beat or flutter | Regular, fast, ‘pounding’ | Regular, fast | Irregular, usually fast; slower in elderly | Regular, fast |
| R adiation | – | – | – | – | – |
| A ssociated features | Nil | Anxiety | Polyuria, lightheadedness, chest tightness | Polyuria, breathlessness Syncope uncommon | Presyncope, syncope, chest tightness |
| T iming | Brief | A few minutes | Minutes to hours | Variable | Variable |
| E xacerbating/relieving factors | Fatigue, caffeine, alcohol may trigger, often relieved by walking (increases sinus rate) |
Exercise or anxiety may trigger | Usually at rest, trivial movements, e.g. bending, may trigger Vagal manoeuvres may relieve |
Exercise or alcohol may trigger; often spontaneous | Exercise may trigger; often spontaneous |
| S everity | Mild (usually) | Mild to moderate | Moderate to severe | Very variable, may be asymptomatic | Often severe |
Ask about:
nature of the palpitation: is the heart beat rapid, forceful or irregular? Can the patient tap it out?
timing of symptoms: speed of onset and offset; frequency and duration of episodes
precipitants for symptoms or relieving factors
associated symptoms: presyncope, syncope or chest pain
history of underlying cardiac disease.
Healthy people are occasionally aware of their heart beating with normal (sinus) rhythm, especially after exercise or in stressful situations such as when waiting for an interview or examination. The sensation is often more common in bed at night and slim people may notice it when lying on their left side.
Ectopic beats (extrasystoles) are a benign cause of palpitation at rest and are abolished by exercise. The premature ectopic beat produces a small stroke volume and an impalpable impulse due to incomplete left ventricular filling. The subsequent compensatory pause leads to ventricular overfilling and a forceful contraction with the next beat. Accordingly, patients often describe ‘missed beats’, sometimes followed by a particularly strong heart beat (‘jolt’ or ‘thump’).
Supraventricular tachycardia produces sudden paroxysms of rapid, regular palpitation that can sometimes be terminated with vagal stimulation using Valsalva breathing manoeuvres or carotid sinus pressure. It often affects young patients with no other underlying cardiac disease. Ventricular tachycardia can produce similar symptoms but is more commonly associated with presyncope or syncope, and tends to affect patients with cardiomyopathy or previous myocardial infarction.
High-risk features that increase the likelihood of a life-threatening arrhythmia such as ventricular tachycardia include:
previous myocardial infarction or cardiac surgery
associated syncope or severe chest pain
family history of sudden death
Wolff–Parkinson–White syndrome
significant structural heart disease such as hypertrophic cardiomyopathy or aortic stenosis.
Syncope is a transient loss of consciousness due to transient cerebral hypoperfusion and episodes are typically characterised by rapid onset, short duration, and spontaneous complete recovery. Causes include postural hypotension, neurocardiogenic syncope, arrhythmias and mechanical obstruction to cardiac output. The same mechanisms may lead to a sensation of lightheadedness and impending loss of consciousness without progressing to actual loss of consciousness (presyncope). The main differential diagnosis of syncope is seizure (p. 136), while lightheadedness and presyncope must be distinguished from dizziness or vertigo due to non-cardiovascular causes (p. 44).
In patients who present with syncope, ask about:
circumstances of the event and any preceding symptoms: palpitation, chest pain, lightheadedness, nausea, tinnitus, sweating or visual disturbance
duration of loss of consciousness, appearance of the patient while unconscious and any injuries sustained (a detailed witness history is extremely helpful)
time to recovery of full consciousness and normal cognition
current driving status, including occupational driving.
In patients with presyncopal symptoms of lightheadedness or dizziness, ask about:
exact nature of symptoms and associated features such as palpitation
precipitants for symptoms, such as postural change, prolonged standing, intense emotion or exertion
frequency of episodes and impact on lifestyle
possible contributing medications, such as antihypertensive agents ( Box 4.8 ).
| Symptom | Medication |
|---|---|
| Angina | Aggravated by thyroxine or drug-induced anaemia, e.g. aspirin or NSAIDs |
| Dyspnoea | Beta-blockers in patients with asthma Exacerbation of heart failure by beta-blockers, some calcium channel antagonists (verapamil, diltiazem), NSAIDs |
| Palpitation | Tachycardia and/or arrhythmia from thyroxine, β 2 stimulants, e.g. salbutamol, digoxin toxicity, hypokalaemia from diuretics, tricyclic antidepressants |
| Syncope/presyncope | Vasodilators, e.g. nitrates, alpha-blockers, ACE inhibitors and angiotensin II receptor antagonists Bradycardia from rate-limiting agents, e.g. beta-blockers, some calcium channel antagonists (verapamil, diltiazem), digoxin, amiodarone |
| Oedema | Glucocorticoids, NSAIDs, some calcium channel antagonists, e.g. nifedipine, amlodipine |
Postural hypotension, a fall of more than 20 mmHg in systolic blood pressure on standing, may lead to syncope or presyncope. It can be caused by hypovolaemia, drugs (see Box 4.8 ) or autonomic neuropathy and is common in the elderly, affecting up to one-third of individuals over 65 years.
Reflex or neurocardiogenic syncope results from excessive autonomic reflexes which produce sudden bradycardia) and/or vasodilatation. Vasovagal syncope is the most common form of reflex syncope and may be triggered in healthy people following a period of prolonged standing or a painful or emotional stimulus, such as the sight of blood. There is typically a prodrome of lightheadedness, tinnitus, nausea, sweating and facial pallor, and a darkening of vision before loss of consciousness. When laid flat to aid cerebral circulation the individual wakes up, often flushing from vasodilatation and nauseated or even vomiting due to vagal overactivity. If the person is held upright by misguided bystanders, continued cerebral hypoperfusion delays recovery and may lead to a seizure and a mistaken diagnosis of epilepsy. In patients presenting with transient loss of consciousness, predictors of vasovagal syncope include a history of syncope or presyncope with pain or medical procedures, an age less than 35 at first syncopal episode, prodrome of sweating, warmth or abdominal discomfort or a postdrome of nausea.
In patients with hypersensitive carotid sinus syndrome, pressure over the carotid sinus may lead to reflex bradycardia and syncope.
Arrhythmias can cause syncope or presyncope. The most common cause is bradyarrhythmia caused by sinoatrial disease or atrioventricular block: Stokes–Adams attacks. Rate-limiting drugs are a common cause of bradyarrhythmia. Supraventricular tachyarrhythmias, like atrial fibrillation, rarely cause syncope whereas ventricular tachycardia often causes syncope or presyncope, especially in patients with impaired left ventricular function.
Mechanical obstruction to left ventricular outflow, including severe aortic stenosis and hypertrophic cardiomyopathy, can cause syncope or presyncope, especially on exertion, when cardiac output cannot meet the increased metabolic demand. Massive pulmonary embolism can lead to syncope by obstructing outflow from the right ventricle; associated features are usually apparent and include acute dyspnoea, chest pain and hypoxia. Cardiac tumours, such as atrial myxoma, and thrombosis, or failure of prosthetic heart valves are rare causes of syncope.
Excess fluid in the interstitial space causes oedema (tissue swelling). It is usually gravity-dependent and so is seen especially around the ankles, or over the sacrum in patients lying in bed. Unilateral lower limb oedema may occur in deep vein thrombosis (DVT) (p. 77). Heart failure is a common cause of bilateral lower limb oedema, but other causes include chronic venous disease, vasodilating calcium channel antagonists (such as amlodipine) and hypoalbuminaemia.
Infective endocarditis, microbial infection of a heart valve, frequently presents with non-specific symptoms, including weight loss, tiredness, fever and night sweats.
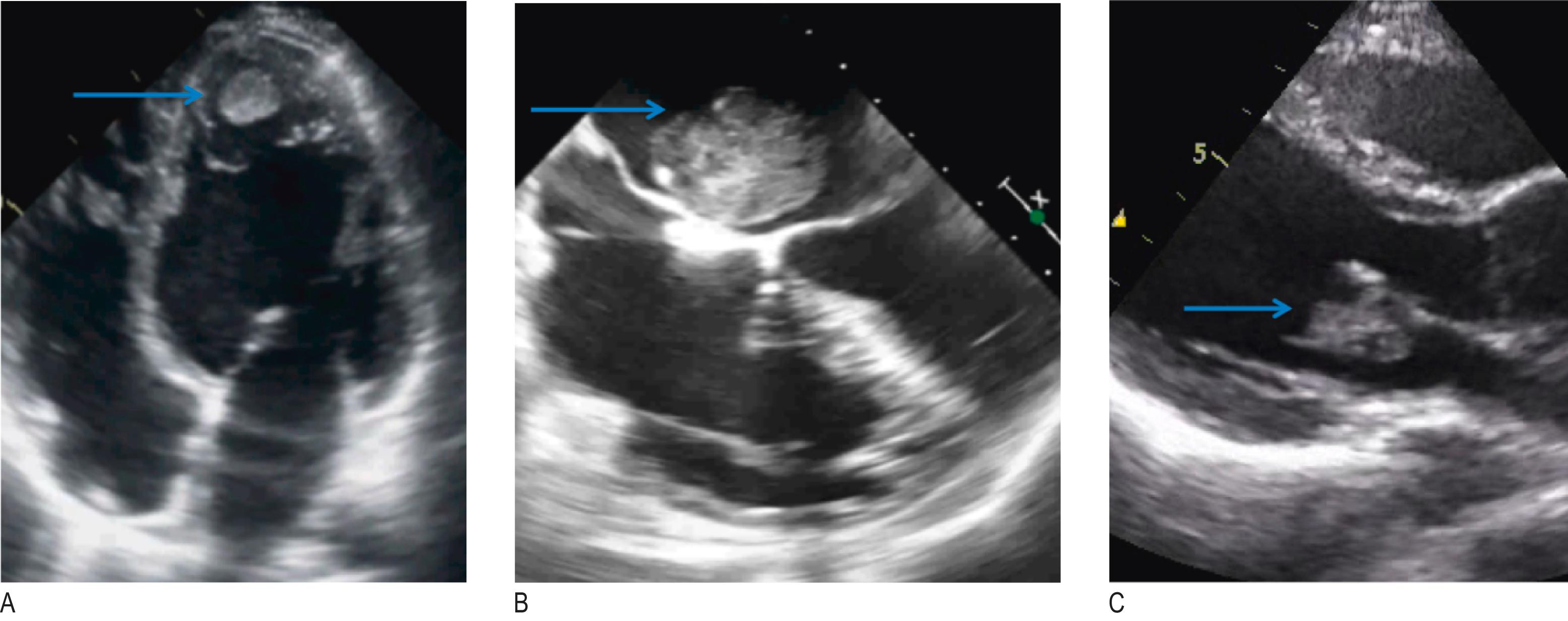
Embolisation of intracardiac thrombus, tumour (such as atrial myxoma) or infective ‘vegetations’ ( Fig. 4.4 ) may produce symptoms of stroke (p. 74), acute limb ischaemia (p. XXX) or acute mesenteric ischaemia (p. 73).
Advanced heart failure may result in either abdominal distension due to ascites, or weight loss and muscle wasting (‘cardiac cachexia’) due to a prolonged catabolic state.
Obtaining a detailed record of any previous cardiac disease, investigations and interventions is essential ( Box 4.9 ). You may need to consult the patient, family members and electronic case records.
| Ischaemic heart disease | Heart failure | Valvular disease | |
|---|---|---|---|
| Baseline symptoms | Exertional angina? If so, ascertain functional limitation (see Box 4.2) / response to GTN spray | Dyspnoea, fatigue, ankle swelling Record usual functional status (see Box 4.6) | Often asymptomatic Exertional dyspnoea (common), chest pain or syncope |
| Major events | Previous myocardial infarction/unstable angina | Hospitalisation for decompensated heart failure Ventricular arrhythmias | Infective endocarditis Previous rheumatic fever |
| Investigations | Coronary angiography (invasive or computed tomography): presence, extent and severity of coronary artery disease, Exercise electrocardiogram (or other stress test): evidence of inducible ischaemia? Exercise capacity and symptoms |
Echocardiogram (± cardiac magnetic resonance imaging): left ventricular size, wall thickness and systolic function; valvular disease; right ventricular function | Echocardiogram (transthoracic ± transoesophageal): nature and severity of valve lesion; ventricular size and function |
| Procedures | Percutaneous coronary intervention (angioplasty and stenting) Coronary artery bypass graft surgery |
Implantable cardioverter–defibrillator Cardiac resynchronisation therapy | Surgical valve repair or replacement (note whether mechanical or bioprosthetic)Transcatheter valve procedures |
Also ask about:
conditions associated with increased risk of vascular disease such as hypertension, diabetes mellitus and hyperlipidaemia
rheumatic fever or heart murmurs during childhood
potential causes of bacteraemia in patients with suspected infective endocarditis, such as skin infection, recent dental work, intravenous drug use or penetrating trauma
systemic disorders with cardiovascular manifestations such as connective tissue diseases (pericarditis and Raynaud’s phenomenon), Marfan’s syndrome (aortic dissection) and myotonic dystrophy (atrioventricular block).
Drugs may cause or aggravate symptoms such as breathlessness, chest pain, oedema, palpitation or syncope (see Box 4.8 ). Ask about ‘over-the-counter’ purchases, such as non-steroidal anti-inflammatory drugs (NSAIDs) and alternative and herbal medicines, as these may have cardiovascular actions.
Many cardiac disorders such as cardiomyopathies have a genetic component. Ask about premature coronary artery disease in first-degree relatives (<60 years in a female or <55 years in a male); sudden unexplained death at a young age may raise the possibility of a cardiomyopathy or inherited arrhythmia. Patients with venous thrombosis may have inherited thrombophilia, such as a factor V Leiden mutation. Familial hypercholesterolaemia is associated with premature arterial disease. Aortic disease can be inherited, and a family history of aortic aneurysm or dissection may be relevant.
Smoking is the strongest risk factor for coronary and peripheral arterial disease (PAD). Take a detailed smoking history (p. 16). Alcohol can induce atrial fibrillation and, in excess, is associated with obesity, hypertension and dilated cardiomyopathy. Recreational drugs such as cocaine and amphetamines can cause arrhythmias, chest pain, occlusive and aneurysmal PAD and even myocardial infarction. Heart disease may have important consequences for employment. Patients with limiting exertional symptoms may struggle to perform jobs that entail a high degree of physical activity. In addition, some diagnoses such as ischaemic heart disease or cardiac arrhythmia may impact on eligibility for certain occupations that have implications for public safety, such as commercial drivers and pilots. Finally, ask about undue stress or anxiety as these are commonly associated with cardiac-type symptoms including chest pain, dyspnoea and palpitation.
Tailor the sequence and extent of examination to the patient’s condition. If you suspect that the person may be unstable, deteriorating or critically unwell (breathless, distressed, cyanosed or obtunded, for example), adopt an ABCDE approach initially (p. 395) and defer detailed examination until stabilised. In stable patients, perform a detailed and comprehensive physical examination.
Look at the patient’s general appearance. Do they look unwell, frightened or distressed? Are there any signs of breathlessness or cyanosis? Is the patient overweight or cachectic? Are there any features of conditions associated with cardiovascular disease such as Marfan’s (p. 33), Down’s (p. 39) or Turner’s syndrome (p. 106), or ankylosing spondylitis (p. 300)?
Conclude by examining the entire skin surface for petechiae, checking the temperature (p. 345) and performing urinalysis (p. 281). Fever is a feature of infective endocarditis and pericarditis, and may occur after myocardial infarction. Urinalysis is necessary to check for haematuria (endocarditis, vasculitis), glucosuria (diabetes) and proteinuria (hypertension and renal disease).
Feel the temperature of the hands and measure capillary refill time (p. 396).
Examine the hands for tobacco staining (see Fig. 5.7 ), skin crease pallor (anaemia) or peripheral cyanosis.
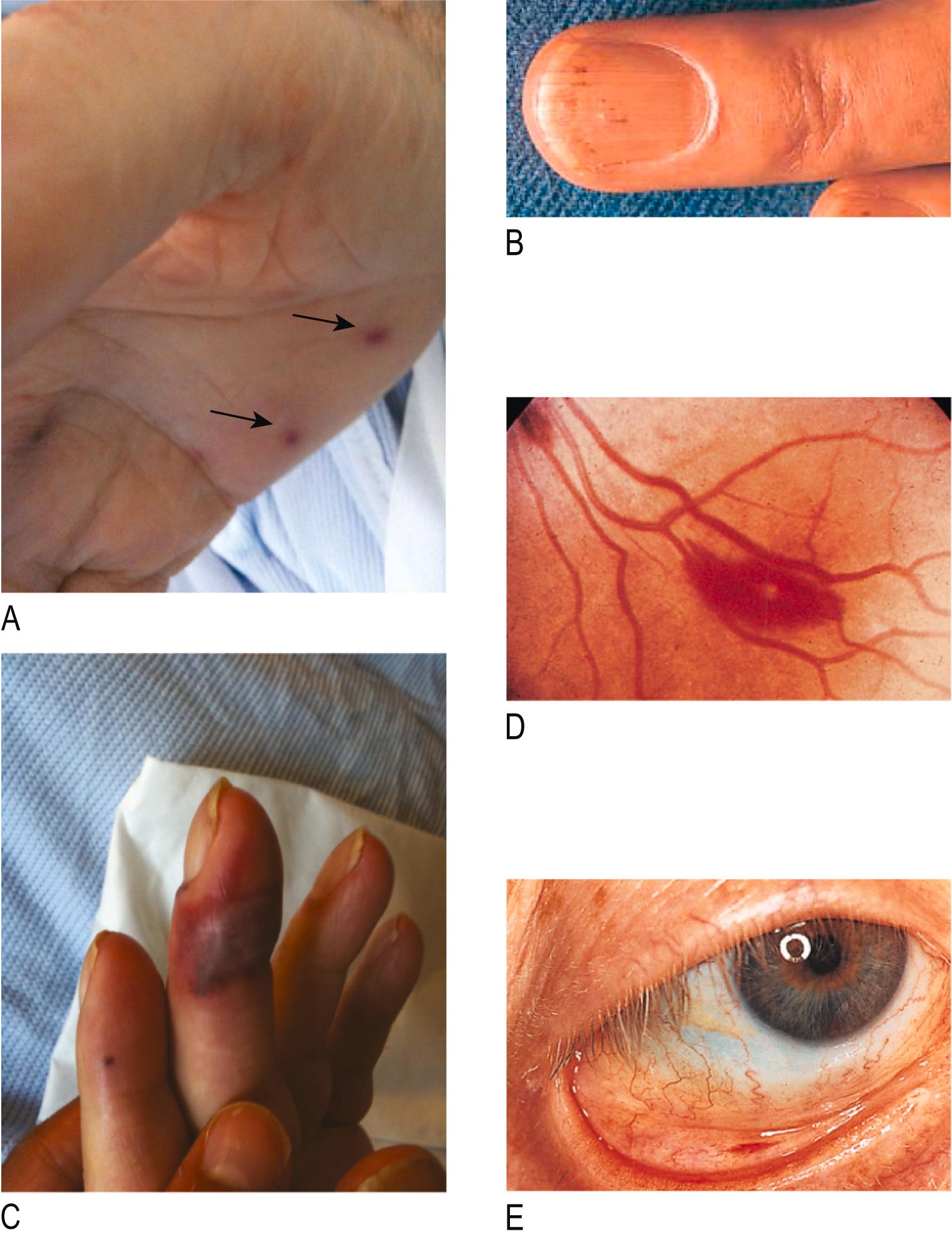
Look at the nails for finger clubbing (p. 326) and for splinter haemorrhages: linear, reddish-brown marks along the axis of the fingernails and toenails ( Fig. 4.5B ).
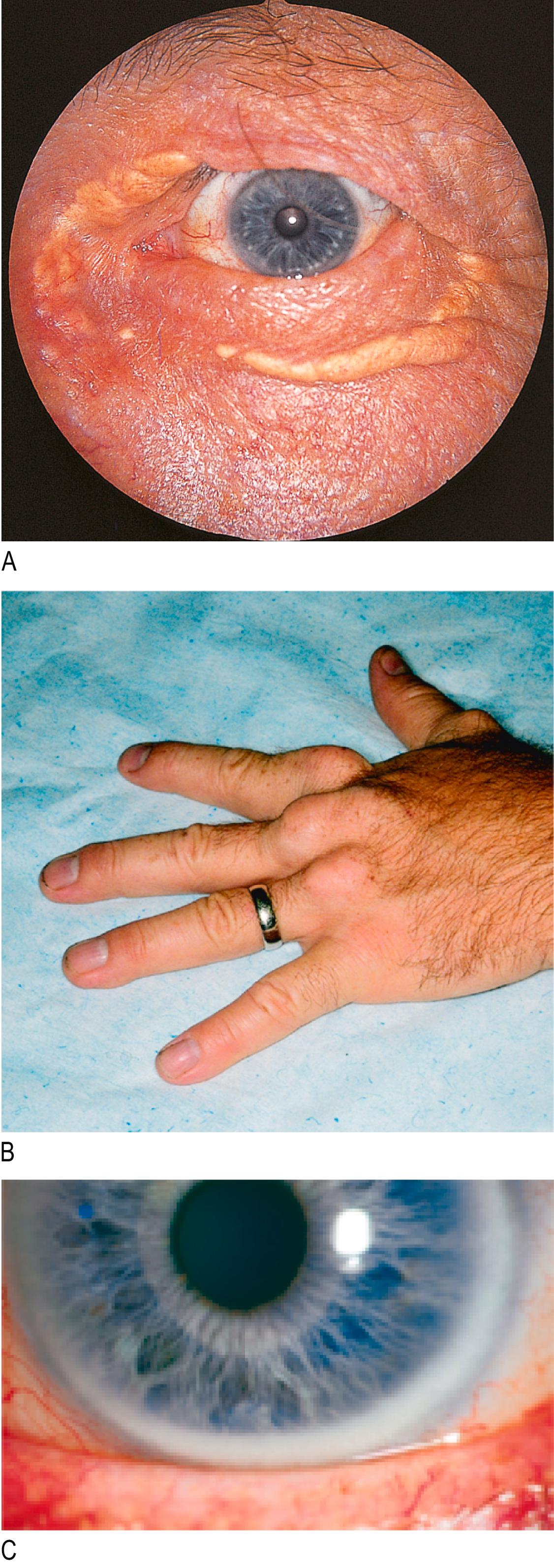
Examine the extensor surface of the hands for tendon xanthomata: hard, slightly yellowish masses over the extensor tendons of the hand from lipid deposits (see Fig. 4.6B ).
Examine the palmar aspect of the hands for:
The hands usually feel dry and warm at ambient temperature. Normal capillary refill time is 2 seconds or less. Cool extremities and prolonged capillary refill time signify impaired peripheral perfusion, which may occur in shock (p. 57) or chronic conditions associated with a low cardiac output state (as in severe aortic stenosis, mitral stenosis or pulmonary hypertension).
One or two isolated splinter haemorrhages from trauma are common in healthy individuals, especially in manual workers. Splinter haemorrhages (see Fig. 4.5B ) are found in infective endocarditis and some vasculitic disorders. A petechial rash (caused by vasculitis), most often present on the legs and conjunctivae (see Fig. 4.5E ), is a transient finding in endocarditis and can be confused with the rash of meningococcal disease. Janeway lesions and Osler's nodes (see Fig. 4.5A and C) are features of endocarditis but are rare in the modern era.
Tendon xanthomata ( Fig. 4.6 ) are a sign of familial hypercholesterolaemia, a genetic disorder associated with severe elevations in serum cholesterol and premature coronary artery disease.
Look in the mouth for central cyanosis: a purplish blue discoloration of the lips and underside of the tongue (see Fig. 5.11 ).
Examine the eyelids for xanthelasmata: soft, yellowish plaques found periorbitally and on the medial aspect of the eyelids ( Fig. 4.6A ).
Look at the iris for corneal arcus: a creamy yellow discoloration at the boundary of the iris and cornea ( Fig. 4.6C ).
Examine the fundi (p. 184) for features of hypertension (p. 189), diabetes (p. 188) or Roth's spots (flame-shaped retinal haemorrhages with a ‘cotton-wool’ centre; Fig. 4.5D ).
Cardiac causes of central cyanosis include heart failure sufficient to cause pulmonary congestion and oedema impairing gas exchange, or, rarely, congenital heart disease, in which case it is associated with right-to-left shunting and finger clubbing (p. 326).
Xanthelasmata and corneal arcus (see Fig. 4.6A and C) are associated with hyperlipidaemia but also occur frequently in normolipidaemic patients. The presence of xanthelasma is an independent risk factor for coronary heart disease and myocardial infarction but corneal arcus has no independent prognostic value.
The palpable pulse in an artery reflects the pressure wave generated by the ejection of blood into the circulation from the left ventricle.
When taking a pulse, assess:
rate: the number of pulses occurring per minute
rhythm: the pattern or regularity of pulses
volume: the perceived degree of pulsation
character: an impression of the pulse waveform or shape.
The rate and rhythm of the pulse are usually determined at the radial artery; use the larger pulses (brachial, carotid or femoral) to assess the pulse volume and character.
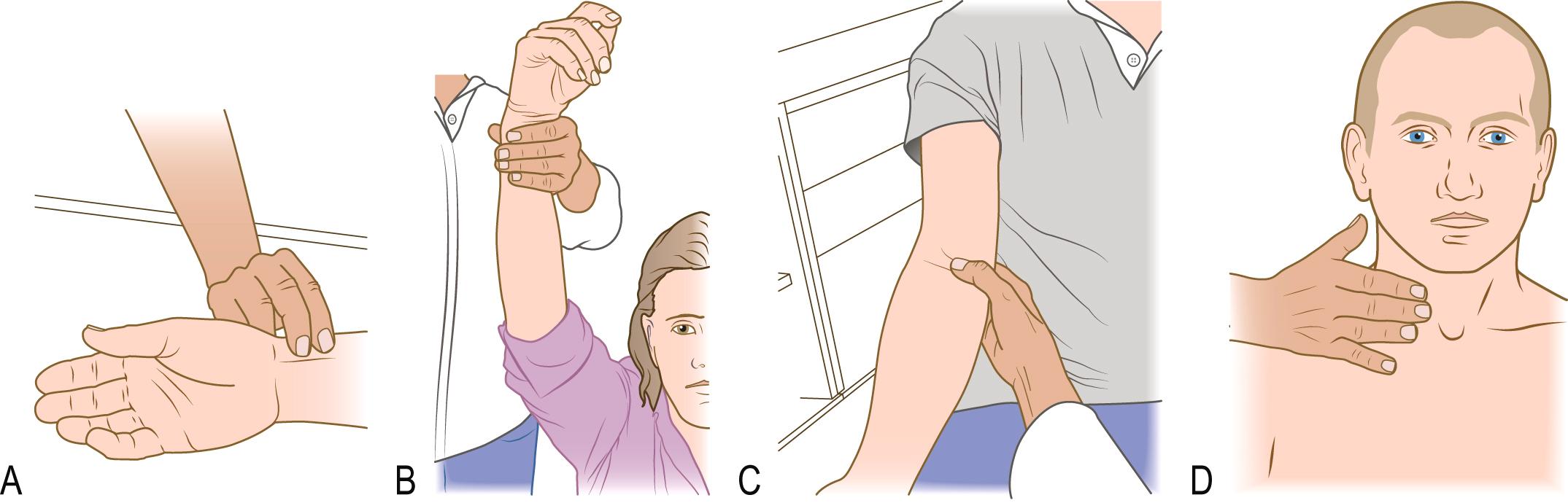
Place the pads of your index and middle fingers over the right wrist, just lateral to the flexor carpi radialis tendon ( Fig. 4.7A ).
Assess the rhythm of the pulse and count the number over 15 seconds; multiply by 4 to obtain the rate in beats per minute (bpm).
To detect a collapsing pulse: first, check that the patient has no shoulder or arm pain or restriction on movement; next, feel the pulse with the base of your fingers, then raise the patient’s arm vertically above their head (see Fig. 4.7B ).
Palpate both radial pulses simultaneously, assessing any delay between the two.
Cup your hand under the elbow and use your thumb to palpate the pulse in the antecubital fossa, just medial to the biceps tendon (see Fig. 4.7C ). Use your right thumb for the patient’s right arm and your left thumb for the patient’s left arm. Assess the character and volume of the pulse.
Explain what you are going to do.
With the patient semi-recumbent, place the tips of your fingers between the larynx and the anterior border of the sternocleidomastoid muscle (see Fig. 4.7D ).
Palpate the pulse gently to avoid a vagal reflex, and never assess both carotids simultaneously.
Listen for bruits over both carotid arteries, using the diaphragm of your stethoscope in held inspiration.
Resting heart rate is normally 50–95 bpm but should be considered in the clinical context. A pulse rate of 40 bpm can be normal in a fit young adult, whereas a pulse rate of 65 bpm may be abnormally low in acute heart failure. Bradycardia is defined as a pulse rate of less than 60 bpm; tachycardia is a rate of greater than 100 bpm. The most common causes of bradycardia are medication, athletic conditioning and sinoatrial or atrioventricular node dysfunction. The most common cause of tachycardia is sinus tachycardia ( Box 4.10 ).
| Abnormality | Sinus rhythm | Arrhythmia |
|---|---|---|
| Fast rate (tachycardia, >100 bpm) | Exercise Pain Excitement/anxiety Fever Hyperthyroidism Medication:
|
Atrial fibrillation Atrial flutter Supraventricular tachycardia Ventricular tachycardia |
| Slow rate (bradycardia, <60 bpm) | Sleep Athletic training Hypothyroidism Medication:
|
Carotid sinus hypersensitivity Sick sinus syndrome Second-degree heart block Complete heart block |
| Irregular pulse | Sinus arrhythmia Atrial extrasystoles Ventricular extrasystoles |
Atrial fibrillation Atrial flutter with variable response Second-degree heart block with variable response |
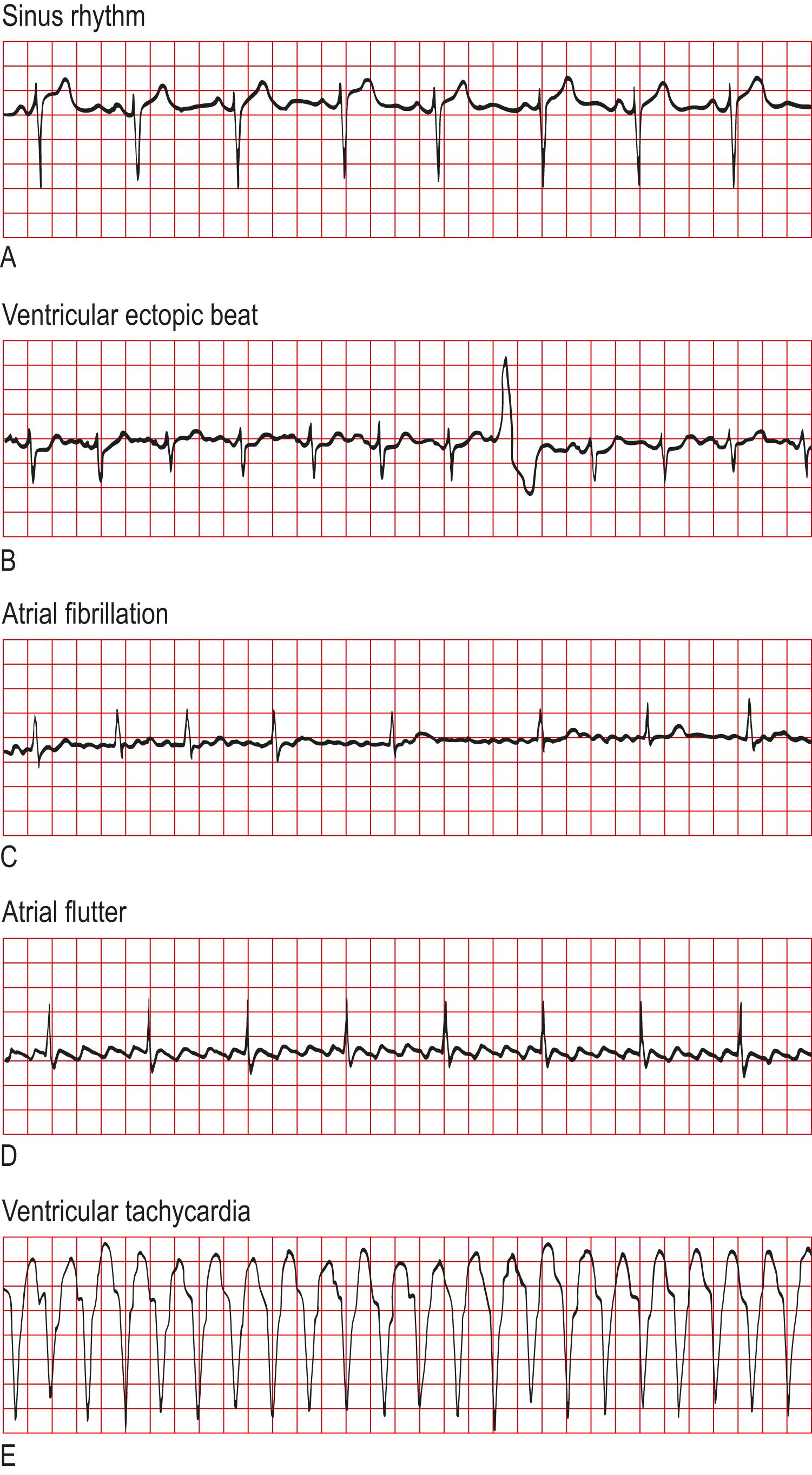
The pulse may be regular or irregular (see Box 4.10 ). Sinus rhythm is regular ( Fig. 4.8A ) but heart rate varies with the respiratory cycle, particularly in children, young adults or athletes (sinus arrhythmia). During inspiration, parasympathetic tone falls and the heart rate increases; on expiration, the heart rate decreases ( Box 4.11 ). With intermittent extrasystoles (see Fig. 4.8B ) or second-degree atrioventricular block, there may be an underlying regularity to the pulse, interspersed with periods of irregularity (sometimes referred to as ‘regularly irregular’). In atrial fibrillation the pulse has no appreciable pattern and is often described as ‘irregularly irregular’ (see Fig. 4.8C ). The rate in atrial fibrillation depends on the number of beats conducted by the atrioventricular node. Untreated, the ventricular rate may be very fast (up to 200 bpm). The variability of the pulse rate (and therefore ventricular filling) explains why the pulse volume varies and there may be a pulse deficit, with some cycles not felt at the radial artery. The pulse deficit can be calculated by counting the radial pulse rate and subtracting this from the apical heart rate, assessed by auscultation.
The ventricles fill during diastole. Longer diastolic intervals are associated with increased stroke volume, which is reflected by increased pulse volume on examination. Abnormalities of pulse volume and character are highly subjective, however, and tend to have poor inter-observer agreement.
A large pulse volume is a reflection of a large pulse pressure, which can occur in physiological states such as exercise or pregnancy, or in pathological conditions such as anaemia, thyrotoxicosis or aortic regurgitation.
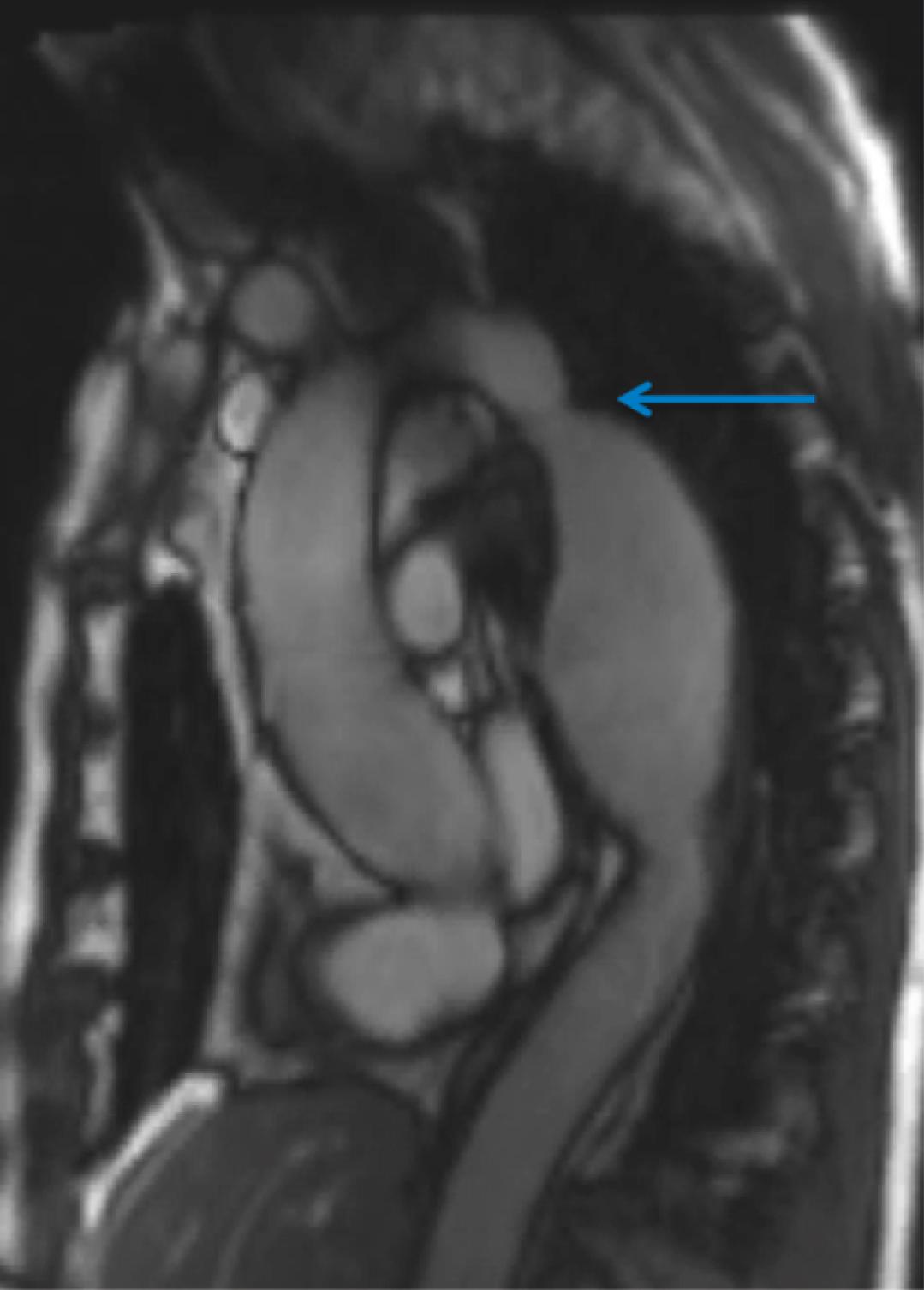
Low pulse volume may result from severe heart failure and conditions associated with inadequate ventricular filling such as hypovolaemia, cardiac tamponade and mitral stenosis. Asymmetric pulses may represent occlusive PAD or stenosis and, rarely, aortic dissection. Coarctation is a congenital narrowing of the aorta, usually distal to the left subclavian artery ( Fig. 4.9 ); it may produce reduced-volume lower limb pulses, which are also delayed relative to the upper limb pulses (radiofemoral delay). In adults, coarctation usually presents with hypertension and heart failure.
A slow-rising pulse has a gradual upstroke with a reduced peak occurring late in systole, and is a feature of severe aortic stenosis ( Fig. 4.10 ).
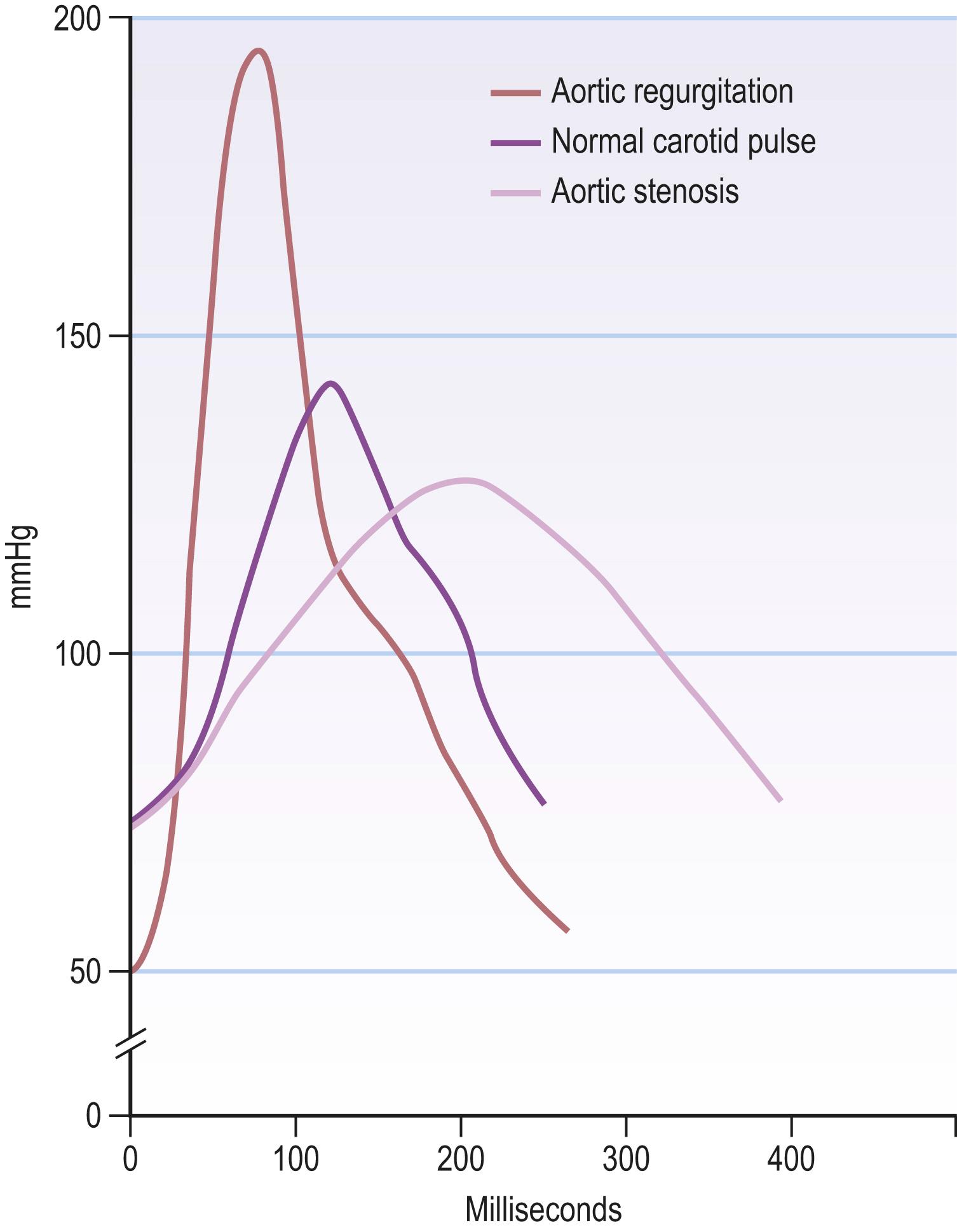
A collapsing pulse may occur with severe aortic regurgitation. The peak of the pulse wave arrives early and is followed by a rapid fall in pressure (see Fig. 4.10 ) as blood flows back into the left ventricle, resulting in a wide pulse pressure (systolic − diastolic blood pressure >80 mmHg). This rapid fall imparts the ‘collapsing’ sensation, and is exaggerated by raising the patient’s arm above the level of the heart (see Fig. 4.7B ).
Pulsus bisferiens, an increased pulse with a double systolic peak separated by a distinct mid-systolic dip, is classically produced by concomitant aortic stenosis and regurgitation. Pulsus alternans, beat-to-beat variation in pulse volume with a normal rhythm, may occur in advanced heart failure. Both of these signs are rare, however, and of limited relevance in contemporary practice.
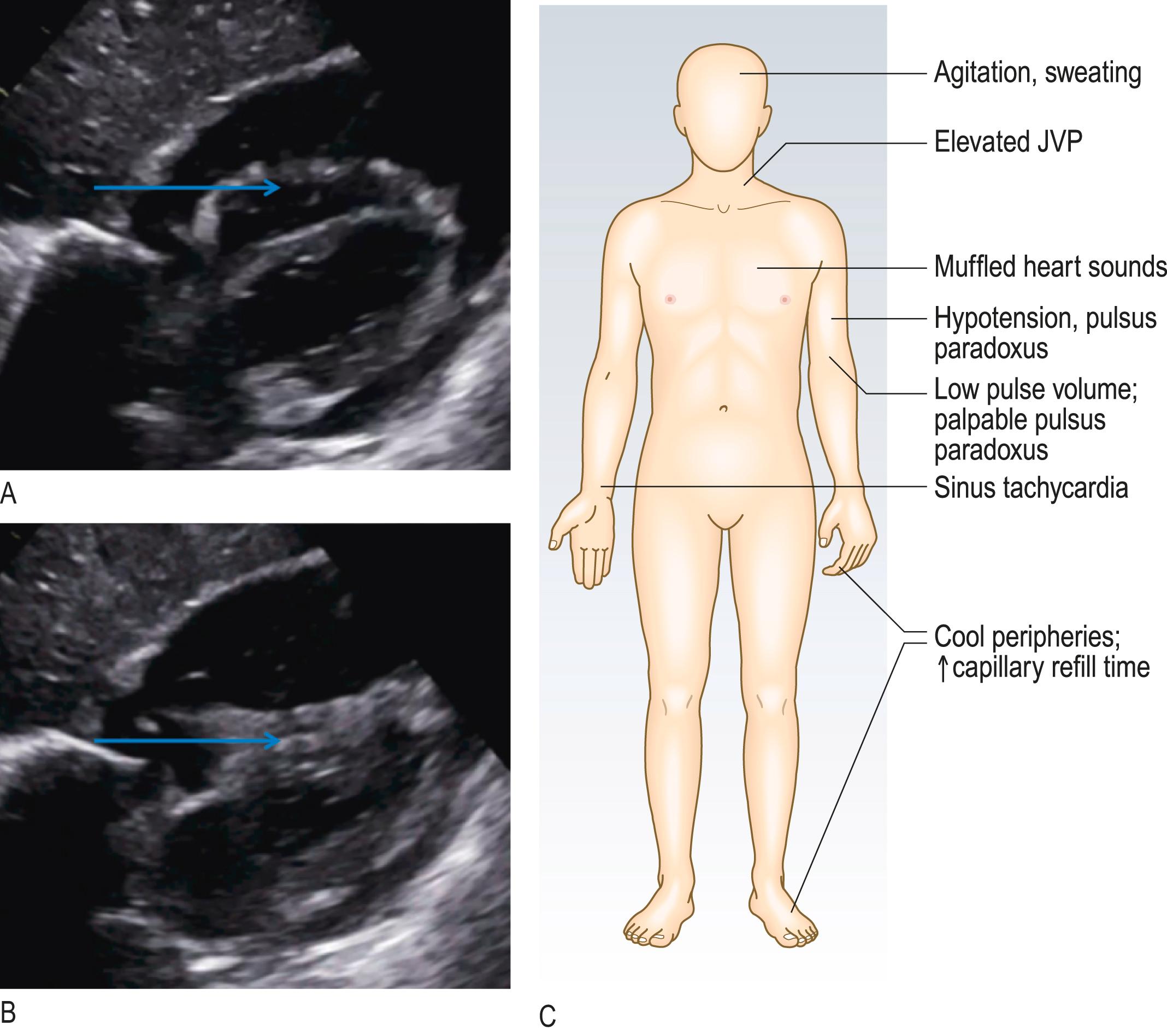
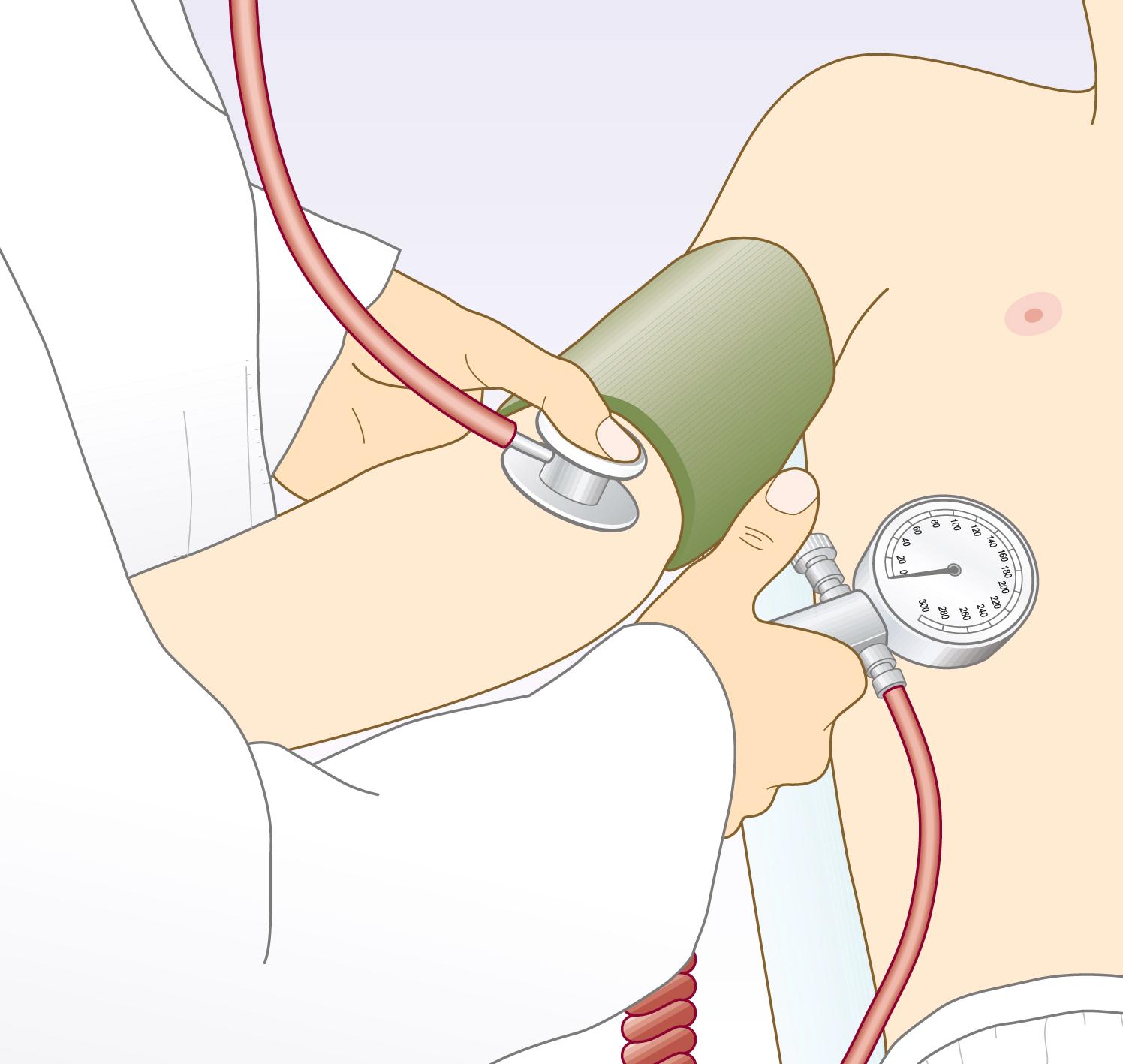
Pulsus paradoxus is an exaggeration of the normal variability of pulse volume with breathing. Pulse volume normally increases in expiration and decreases during inspiration due to intrathoracic pressure changes affecting venous return to the heart. This variability is exaggerated when ventricular diastolic filling is impeded by elevated intrapericardial pressure. This is usually due to accumulation of pericardial fluid (cardiac tamponade; Fig. 4.11 ) but can occur to a lesser extent with pericardial constriction and in acute severe asthma. If suspected, pulsus paradoxus can be confirmed using a blood pressure (BP) cuff (see later and Fig. 4.12 ); a fall of greater than 10 mmHg between the cuff pressure at which Korotkoff sounds appear in expiration only and the cuff pressure at which Korotkoff sounds persist throughout the respiratory cycle is diagnostic.
BP is a measure of the pressure that the circulating blood exerts against the arterial walls. Systolic pressure is the maximal pressure that occurs during ventricular contraction (systole). During ventricular filling (diastole), arterial pressure is maintained at a lower level by the elasticity and compliance of the vessel wall. The lowest value (diastolic pressure) occurs immediately before the next cycle.
BP is usually measured using a sphygmomanometer (see Fig. 4.12 ). In certain situations, such as the intensive care unit, it is measured invasively using an indwelling intra-arterial catheter connected to a pressure sensor.
BP is measured in mmHg and recorded as systolic pressure/diastolic pressure, together with a note of where and how the reading was taken: for example, BP 146/92 mmHg, right arm, supine.
BP provides vital information on the haemodynamic condition of acutely ill or injured patients. Over the longer term it is also an important guide to cardiovascular risk. BP constantly varies and rises with stress, excitement and environment. ‘White coat hypertension’ refers to a transient increase in BP caused by the stress of being in a healthcare setting. Ambulatory BP measurement, using a portable device at intervals during normal daytime activity and at night, is better at determining cardiovascular risk.
Although any threshold for distinguishing abnormal elevation of BP from normal BP is somewhat arbitrary, hypertension is widely defined as a systolic pressure of ≥140 mmHg and/or a diastolic pressure ≥90 mmHg ( Box 4.12 ). Hypertension is associated with significant morbidity and mortality from vascular disease (heart failure, coronary artery disease, cerebrovascular disease and chronic kidney disease). It is almost invariably asymptomatic, although, rarely and in severe hypertension, headaches and visual disturbances can occur. In most hypertensive patients there is no identifiable cause – so-called ‘essential hypertension’. Secondary hypertension is rare, occurring in less than 1% of the hypertensive population ( Box 4.13 ).
| BP | Systolic BP (mmHg) | Diastolic BP (mmHg) |
|---|---|---|
| Optimal | <120 | <80 |
| Normal | <130 | <85 |
| High normal | 130–139 | 85–89 |
| Hypertension | ||
| Grade 1 (mild) | 140–159 | 90–99 |
| Grade 2 (moderate) | 160–179 | 100–109 |
| Grade 3 (severe) | >180 | >110 |
| Isolated systolic hypertension b | ||
| 140–159 | <90 | |
a BP category is defined according to seated clinic BP and by the highest level of BP, whether systolic or diastolic.
b Isolated systolic hypertension is graded 1, 2, or 3 according to SBP values in the ranges indicated. BP, Blood pressure.From Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J . 2018;39(33):3021–3104.
| Clinical feature | Cause |
|---|---|
| Widespread vascular disease Renal bruit | Renovascular disease, including renal artery stenosis |
| Episodes of sweating, headache and palpitation | Phaeochromocytoma |
| Hypokalaemia | Primary aldosteronism |
| Cushingoid facies, central obesity, abdominal striae, proximal muscle weaknessChronic glucocorticoid use | Cushing’s syndrome |
| Low-volume femoral pulses with radiofemoral delay | Coarctation of the aorta |
| Bilateral palpable kidneys | Adult polycystic kidney disease (p. 277) |
Assess the hypertensive patient for:
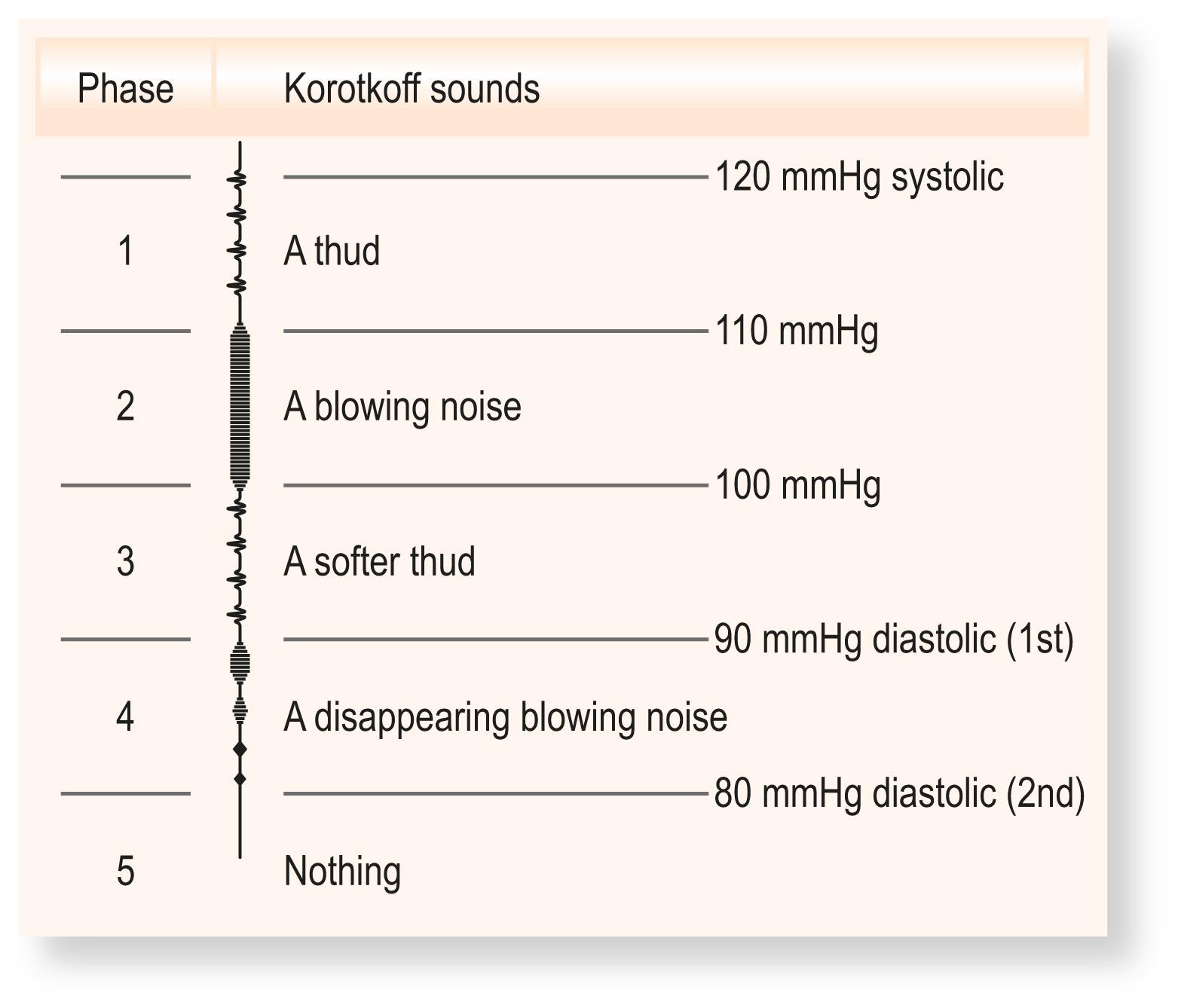
These sounds are produced when the cuff pressure is between systolic and diastolic because the artery collapses completely and reopens with each heart beat, producing a snapping or knocking sound ( Fig. 4.13 ). The first appearance of sounds (phase 1) during cuff deflation indicates systole. As pressure is gradually reduced, the sounds muffle (phase 4) and then disappear (phase 5).
Rest the patient for 5 minutes.
Ideally, measure BP in both arms (brachial arteries); the higher of the two is closest to central aortic pressure and should be used to determine treatment.
With the patient seated or lying down, support their arm comfortably at about heart level, with no tight clothing constricting the upper arm.
Apply an appropriately sized cuff to the upper arm, with the centre of the bladder over the brachial artery.
Palpate the brachial pulse.
Inflate the cuff until the pulse is impalpable. Note the pressure on the manometer; this is a rough estimate of systolic pressure.
Inflate the cuff another 30 mmHg and listen through the diaphragm of the stethoscope placed over the brachial artery.
Deflate the cuff slowly (2–3 mmHg/s) until you hear a regular tapping sound (phase 1 Korotkoff sounds). Record the reading to the nearest 2 mmHg. This is the systolic pressure.
Continue to deflate the cuff slowly until the sounds disappear.
Record the pressure at which the sounds completely disappear as the diastolic pressure (phase 5). If muffled sounds persist (phase 4) and do not disappear, use the point of muffling as the diastolic pressure.
Different BP in each arm: a difference of greater than 10 mmHg on repeated measurements suggests the presence of aortic or subclavian artery disease. Record the highest pressure and use this to guide management.
Wrong cuff size: the bladder should be approximately 80% of the length and 40% of the width of the upper arm circumference. A standard adult cuff has a bladder that measures approximately 13 × 30 cm and suits an arm circumference of 22–26 cm. In obese patients a standard adult cuff will overestimate BP, so use a large adult (bladder 16 × 38 cm) or thigh cuff (20 × 42 cm).
Auscultatory gap: up to 20% of elderly hypertensive patients have Korotkoff sounds that appear at systolic pressure and disappear for an interval between systolic and diastolic pressure. If the first appearance of the sound is missed, the systolic pressure will be recorded at a falsely low level. Avoid this by palpating the systolic pressure first.
Patient’s arm at the wrong level: the patient’s elbow should be level with the heart. Hydrostatic pressure causes a change of approximately 5 mmHg in recorded systolic and diastolic BP for a 7 cm change in arm elevation.
Postural change: the pulse increases by about 11 bpm, systolic BP falls by 3–4 mmHg and diastolic BP rises by 5–6 mmHg when a healthy person stands. The BP stabilises after 1–2 minutes. Check the BP after a patient has been standing for 2 minutes; a drop of greater than 20 mmHg on standing is postural hypotension.
Atrial fibrillation: in this condition, stroke volume and BP vary from beat to beat, making accurate measurement challenging, so extra care is needed. Reducing cuff pressure slowly and repeating the measurement more than once will allow an acceptable average value of BP to be obtained.
Estimate the jugular venous pressure (JVP) by observing the level of pulsation in the internal jugular vein. The vein runs deep to the sternomastoid muscle and enters the thorax between the sternal and clavicular heads. The normal JVP waveform has two main peaks per cycle, which helps to distinguish it from the carotid arterial pulse ( Box 4.14 ). Although the right internal jugular vein is traditionally used, studies using the left internal jugular vein have yielded similarly accurate results. The external jugular vein is more superficial, prominent and easier to see. It can be kinked or obstructed as it traverses the deep fascia of the neck but, when visible and pulsatile, can be used to estimate the JVP in difficult cases.
| Carotid | Jugular |
|---|---|
| Rapid outward movement | Rapid inward movement |
| One peak per heart beat | Two peaks per heart beat (in sinus rhythm) |
| Palpable | Impalpable |
| Pulsation unaffected by pressure at the root of the neck | Pulsation diminished by pressure at the root of the neck |
| Independent of respiration | Height of pulsation varies with respiration |
| Independent of the position of the patient | Varies with the position of the patient |
| Independent of abdominal pressure | Rises with abdominal pressure |
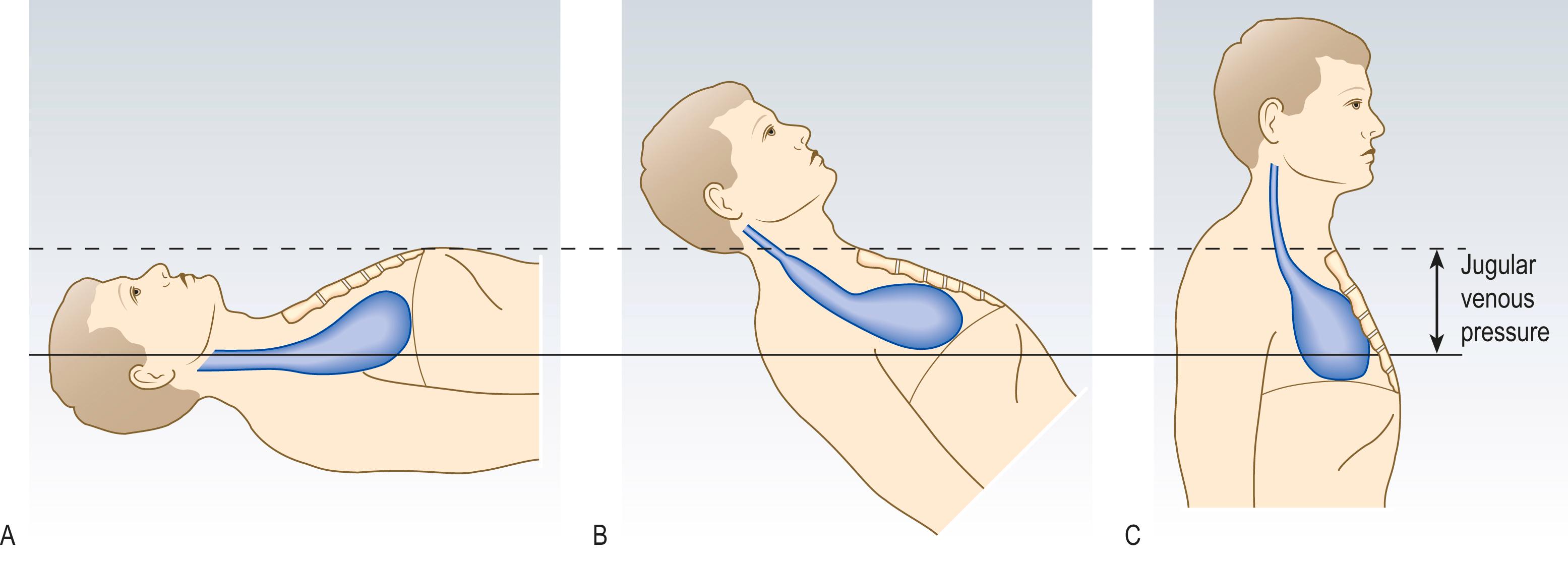
The JVP level reflects right atrial pressure (normally <7 mmHg/9–10 cmH 2 O). If right atrial pressure is low, the patient may have to lie flat for the JVP to be seen; if high, the patient may need to sit upright ( Fig. 4.14 ).
Position the patient supine, reclined at 45 degrees, with the head resting on a pillow and turned slightly to the left. The jugular venous pressure (JVP) is seen best if the sternocleidomastoid muscles and overlying skin are relaxed, so ensure the head is supported and avoid excessive head turning or elevation of the chin.
Look across the patient’s neck from the right side ( Fig. 4.15A ). Use oblique lighting if the JVP is difficult to see.
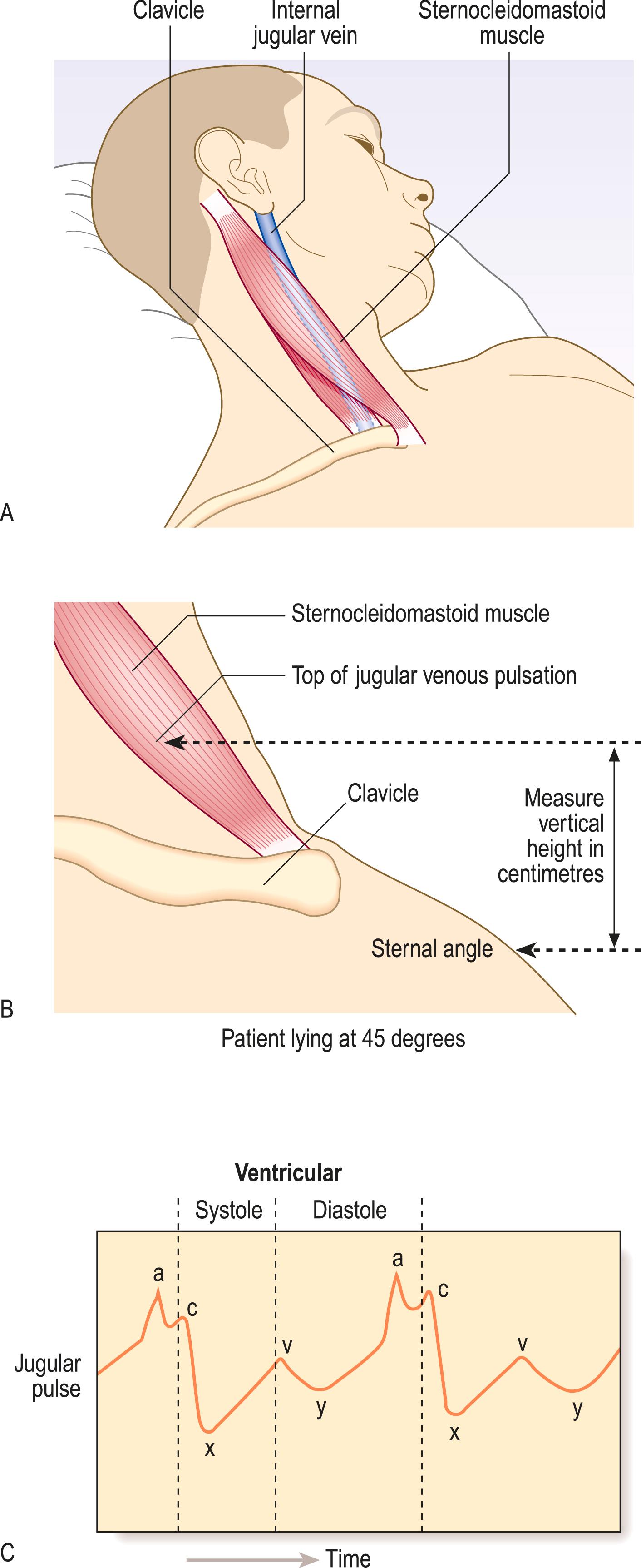
Identify the jugular vein pulsation behind the sternocleidomastoid muscle (usually just above the clavicle, unless it is elevated).
If a pulsation is visualised, use the abdominojugular test and/or occlusion to help confirm that it is the JVP.
The JVP is the vertical height in centimetres between the upper limit of the venous pulsation and the sternal angle (junction of the manubrium and sternum at the level of the second costal cartilages; Fig. 4.15B ).
Identify the timing and waveform of the pulsation and note any abnormality.
It can be difficult to differentiate the jugular venous waveform from arterial pulsation (see Box 4.14 ). If that is the case, the following may help:
Abdominojugular test: press firmly over the abdomen. This increases venous return to the right side of the heart temporarily and the JVP normally rises.
Changes with respiration: the JVP normally falls with inspiration due to decreased intrathoracic pressure.
Waveform: the normal JVP waveform has two distinct peaks per cardiac cycle (see Fig. 4.15C ):
The ‘a’ wave corresponds to right atrial contraction and occurs just before the first heart sound. In atrial fibrillation the ‘a’ wave is absent.
The ‘v’ wave is caused by atrial filling during ventricular systole when the tricuspid valve is closed.
Rarely, a third peak (‘c’ wave) may be seen due to closure of the tricuspid valve.
Occlusion: the JVP waveform is obliterated by gently occluding the vein at the base of the neck with your finger.
Changes with position: the JVP will vary with the position of the patient (see Fig. 4.14 ).
The JVP provides a reasonably accurate guide to central venous pressure, though it is better to estimate whether this is high, normal or low rather than attempting to measure a specific value. A JVP greater than 3 cm above the sternal angle strongly suggests elevated central venous pressure which occurs in states of volume overload (particularly heart failure). It is also elevated in any condition that leads to high right ventricular filling pressures, such as pulmonary embolism, chronic pulmonary hypertension, cardiac tamponade (see Fig. 4.11 ) or pericardial constriction ( Box 4.15 ).
| Condition | Abnormalities |
|---|---|
| Heart failure | Elevation, sustained abdominojugular reflux >10 seconds |
| Pulmonary embolism | Elevation |
| Pericardial effusion | Elevation, prominent ‘y’ descent |
| Pericardial constriction | Elevation, Kussmaul's sign |
| Superior vena cava obstruction | Elevation, loss of pulsation |
| Atrial fibrillation | Absent ‘a’ waves |
| Tricuspid stenosis | Giant ‘a’ waves |
| Tricuspid regurgitation | Giant ‘v’ or ‘cv’ waves |
| Complete heart block | ‘Cannon’ waves |
In patients presenting with dyspnoea, an elevated JVP is a very valuable sign for diagnosing heart failure; examine the patient for pulmonary oedema or pleural effusions (p. 85), ascites (p. 123) and/or peripheral oedema (p. 280).
Mechanical obstruction of the superior vena cava (most often caused by lung cancer) may cause extreme, non-pulsatile elevation of the JVP. In this case the JVP no longer reflects right atrial pressure and the abdominojugular test will be negative.
Kussmaul’s sign is a paradoxical rise of JVP on inspiration that is seen in pericardial constriction, severe right ventricular failure and restrictive cardiomyopathy.
Prominent ‘a’ waves are caused by delayed or restricted right ventricular filling, as in pulmonary hypertension or tricuspid stenosis.
Cannon waves (giant ‘a’ waves) occur when the right atrium contracts against a closed tricuspid valve. Irregular cannon waves are seen in complete heart block and are due to atrioventricular dissociation. Regular cannon waves occur during junctional rhythm and with some ventricular and supraventricular tachycardias.
Tricuspid regurgitation results in prominent systolic ‘v’ waves, which can fuse with the ‘c’ waves to produce ‘cv’ waves; there may be an associated pulsatile liver.
The precordium is the anterior chest surface overlying the heart and great vessels.
Learn the surface anatomy and basic physiology of the heart to understand the basis and timing of the heart sounds and murmurs, and why they are heard best in different locations and radiate in a particular direction ( Fig. 4.16 ).
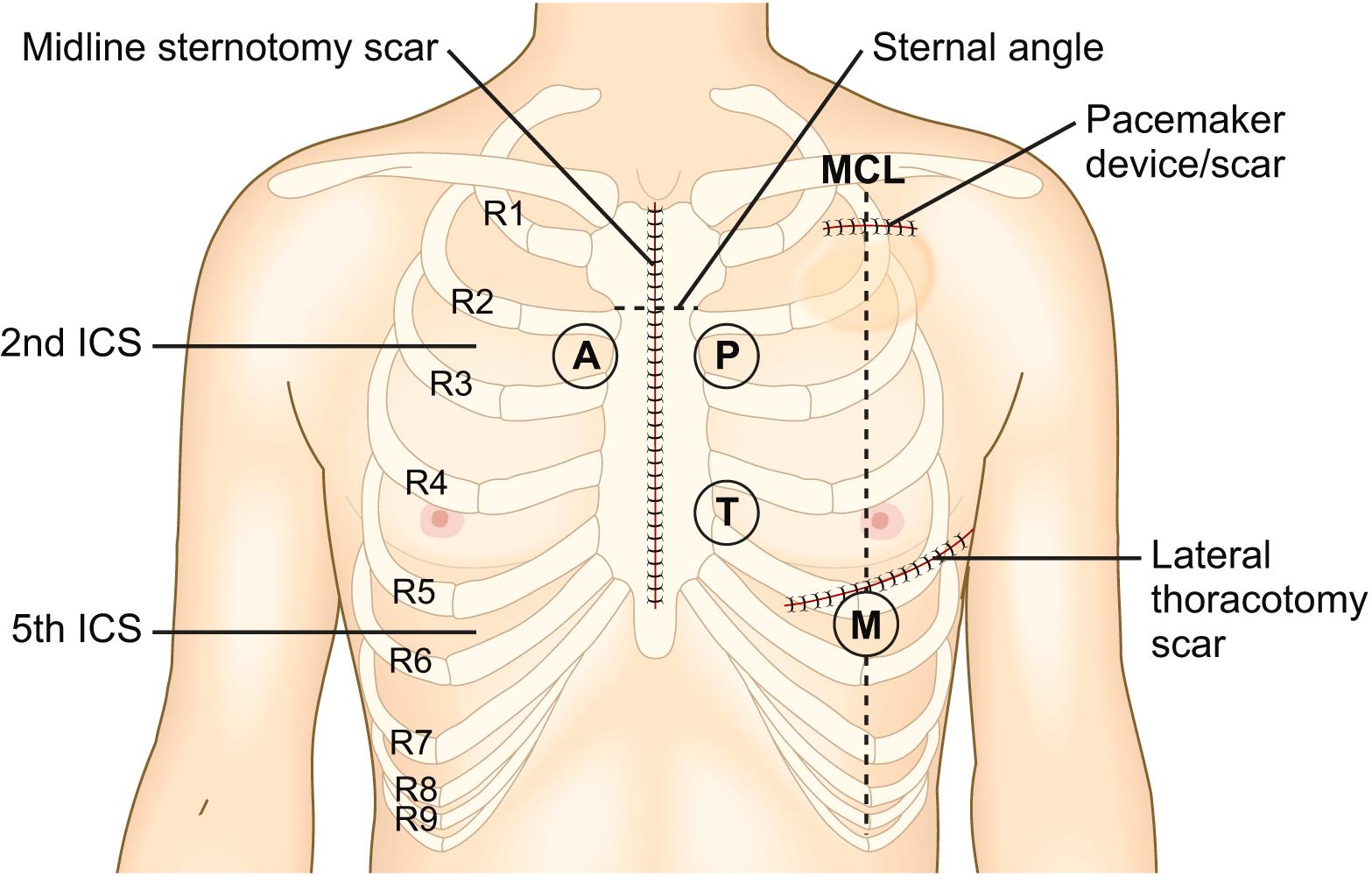
Pectus excavatum (funnel chest; see Fig. 5.5D ), a posterior displacement of the lower sternum, and pectus carinatum (pigeon chest; see Fig. 5.5C ) may displace the heart and affect palpation and auscultation. Scars or visible bulges on the chest may indicate previous cardiac surgery or device implantation, e.g. cardiac pacemaker.
The cardiac impulse results from the left ventricle moving forwards and striking the chest wall during systole and may be visible on inspection. The apex beat is defined as the most lateral and inferior position at which the cardiac impulse can be felt. A heave is a palpable impulse that noticeably lifts your hand. A thrill is the tactile equivalent of a murmur and is a palpable vibration.
Explain that you wish to examine the chest and ask the patient to remove all clothing above the waist. Keep a female patient’s chest covered with a sheet as far as possible.
Inspect the precordium with the patient sitting at a 45-degree angle with shoulders horizontal. Look for surgical scars, visible pulsations and chest deformity.
Place your right hand flat over the precordium to obtain a general impression of the cardiac impulse ( Fig. 4.17A ) then lay your fingers on the chest parallel to the rib spaces to locate the most inferior and lateral position at which the impulse is palpable (the apex beat); if you cannot feel it, ask the patient to roll onto their left side (see Fig. 4.17B ).
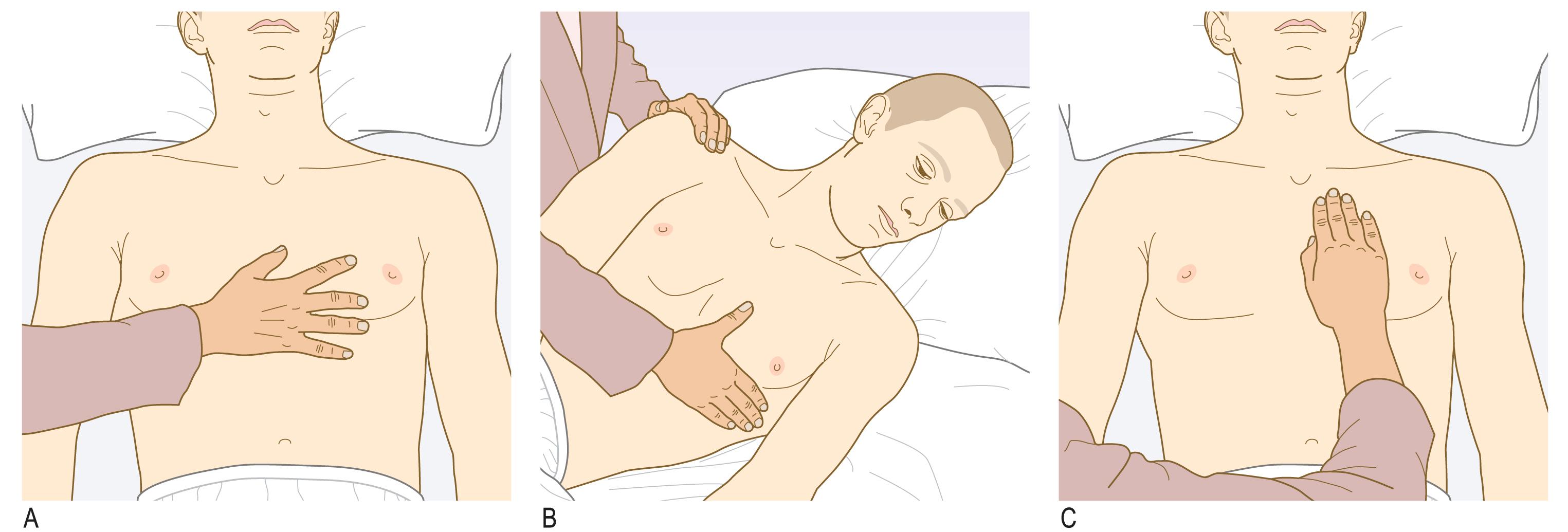
Assess the character of the apex beat and note its position by counting down the intercostal spaces from the second, which is just below the sternal angle.
Apply the heel of your right hand firmly to the left parasternal area and feel for a right ventricular heave. Ask the patient to hold their breath in expiration (see Fig. 4.17C ).
Palpate for thrills at the apex and on both sides of the sternum using the flat of your fingers.
A midline sternotomy scar usually indicates previous valve replacement or coronary artery bypass surgery, in which case it may be accompanied by the saphenous vein or radial artery graft harvest scars. A left submammary scar is usually the result of mitral valvotomy or transapical-transcatheter aortic-valve implantation. Infraclavicular scars are seen after pacemaker or defibrillator implantation, and the bulge of the device may be obvious in this position.
A normal apical impulse briefly lifts your fingers and is localised, but it may be impalpable, particularly in overweight or muscular people, or in patients with hyperinflated lungs due to obstructive airways disease (see Fig. 5.4 ).
The apex beat is normally in the fifth left intercostal space at, or just medial to, the mid-clavicular line (see Fig. 4.16 ). It may be displaced laterally, to the anterior or mid-axillary line, or inferiorly to the sixth or seventh intercostal space when the left ventricle is dilated e.g. in patients with heart failure or severe aortic regurgitation. When detected, a displaced apex beat is one of the most helpful clinical signs for identifying patients with left ventricular systolic dysfunction, although it is important to note that a non-displaced apex beat does not help to rule out heart disease. In dextrocardia the cardiac apex is palpable on the right side but this condition is uncommon, with a prevalence of 1:10,000.
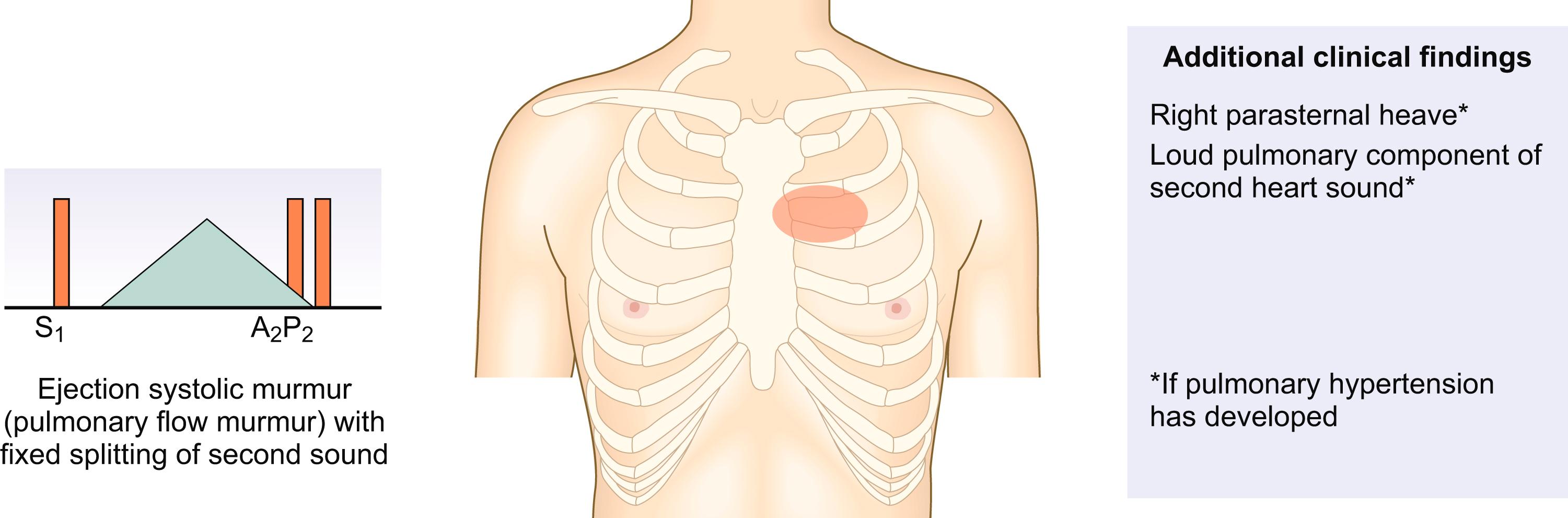
A sustained and forceful but undisplaced apical impulse, known as an apical ‘heave’ is sometimes detected in patients with left ventricular hypertrophy due to hypertension or severe aortic stenosis, whilst a diffuse and less forceful impulse is more characteristic of left ventricular dilatation. Pulsation over the left parasternal area (right ventricular heave) indicates right ventricular hypertrophy or dilatation, most often accompanying pulmonary hypertension. The ‘tapping’ apex beat in mitral stenosis represents a palpable first heart sound and is not usually displaced.
The most common thrill is that of aortic stenosis, which is usually palpable over the upper right sternal border. The thrill caused by a ventricular septal defect is best felt at the left and right sternal edges. Diastolic thrills are very rare.
Use auscultation to identify and characterise the heart sounds and any added sounds and/or murmurs. The optimal sites for auscultation do not correspond with the location of cardiac structures but are where the transmitted sounds and murmurs are best heard ( Box 4.16 ).
| Site | Sound |
|---|---|
| Cardiac apex (mitral area) | First heart sound Third and fourth heart sounds Mid-diastolic murmur of mitral stenosis Opening snap of mitral stenosis |
| Lower left sternal border (tricuspid area) | Early diastolic murmur of aortic regurgitation and pansystolic murmur of tricuspid regurgitation Pansystolic murmur of ventricular septal defect |
| Upper left sternal border (pulmonary area) | Second heart sound Pulmonary valve murmurs |
| Upper right sternal border (aortic area) | Systolic ejection (outflow) murmurs, e.g. aortic stenosis, hypertrophic cardiomyopathy |
| Left axilla | Radiation of the pansystolic murmur of mitral regurgitation |
| Below left clavicle | Continuous ‘machinery’ murmur of a persistent patent ductus arteriosus |
The diaphragm accentuates high-frequency sounds and is better for hearing normal heart sounds and high-pitched sounds, such as the early diastolic murmur of aortic regurgitation. The bell is better for hearing low pitched sounds, particularly the diastolic murmur of mitral stenosis and third and fourth heart sounds.
Minimise external noise as far as possible when you auscultate. Your stethoscope should fit comfortably with the earpieces angled slightly forwards. The tubing should be approximately 25 cm long and thick enough to reduce external sound.
Follow the same approach at each site that you auscultate:
Identify the first and second heart sounds (S 1 and S 2 ) by simultaneously palpating the carotid pulse; the S 1 immediately precedes the upstroke of the pulse, while the S 2 follows well after.
Assess the character and intensity of S 1 and S 2 ; note any splitting of S 2 and how it varies with respiration.
Next, concentrate in turn on systole (the interval between S 1 and S 2 ) and diastole (the interval between S 2 and S 1 ). Listen specifically for:
Added heart sounds (S 3 and S 4 )
Additional sounds such as clicks, snaps and pericardial rubs
Murmurs (see below)
Follow a regular sequence for auscultation:
Listen with your stethoscope diaphragm at the:
apex
lower left sternal border
upper right and left sternal borders.
Listen with your stethoscope bell at the:
apex
lower left sternal border.
Listen over the carotid arteries (ejection systolic murmur of aortic stenosis and carotid bruits) and in the left axilla (pansystolic murmur of mitral regurgitation).
Roll the patient on to their left side. Listen at the apex using light pressure with the bell to detect the mid-diastolic murmur of mitral stenosis ( Fig. 4.18A ).
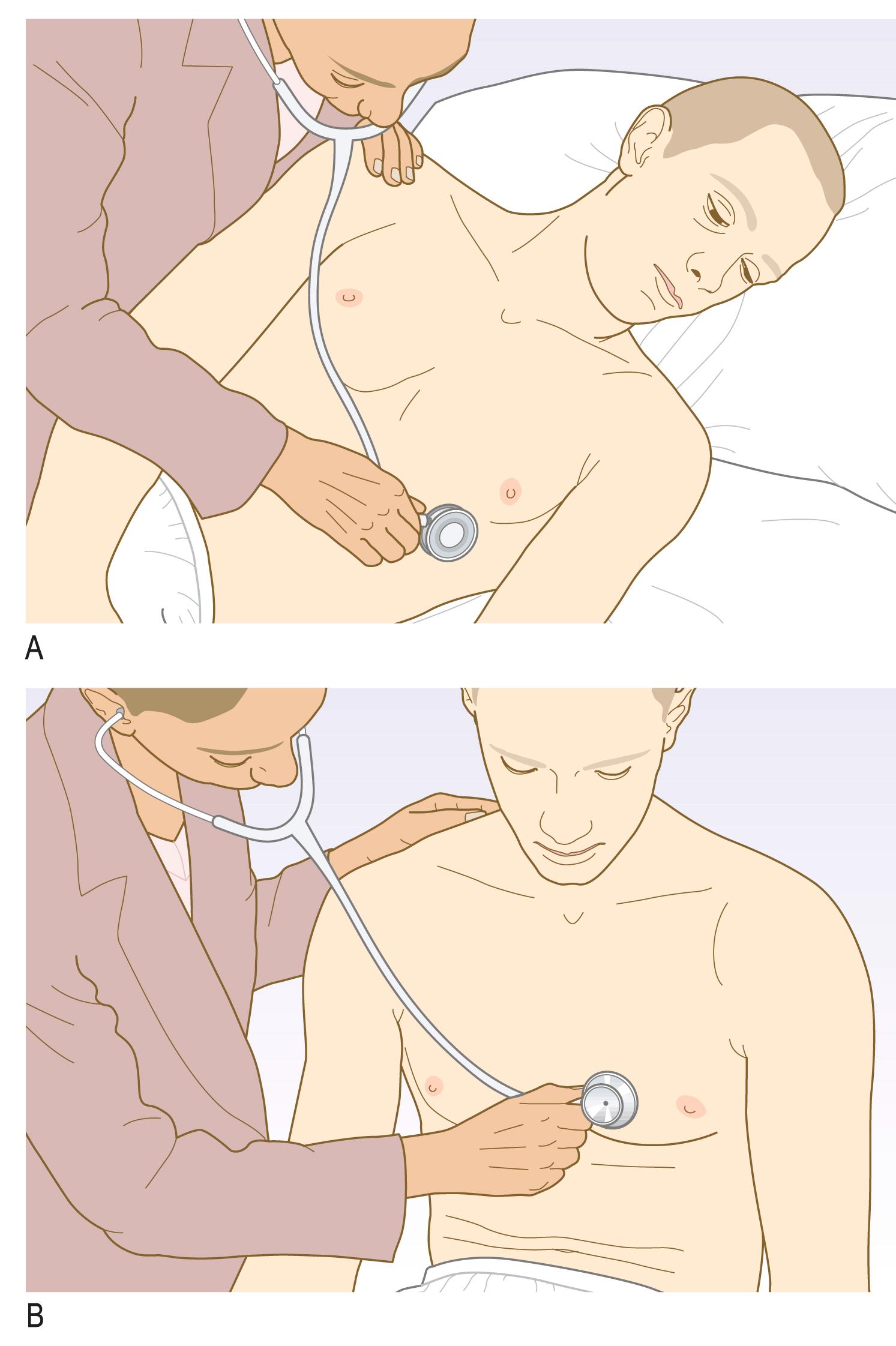
Ask the patient to sit up and lean forwards, then to breathe out fully and hold their breath (see Fig. 4.18B ). Listen over the right second intercostal space and over the left sternal edge with the diaphragm for the murmur of aortic regurgitation.
Integrate the findings from the different sites you have auscultated to characterise any murmurs detected.
Timing and duration. Ask yourself if the murmur is systolic (interval between S 1 and S 2 ) or diastolic (interval between S 2 and S 1 ).
If the murmur is systolic, does it:
persist throughout the whole of systole with no distinct gap between the murmur and either S 1 or S 2 (‘pansystolic’ or ‘holosystolic’)?
occur from the onset of systole (no gap between S 1 and murmur) but with a distinct gap between the end of the murmur and S 2 (typical of ‘ejection systolic’ murmur)?
begin later in systole with a distinct gap between S 1 and the onset of the murmur (mid/late systolic murmur)?
If the murmur is diastolic does it:
persist throughout the whole of diastole with no distinct gap between the murmur and either S 1 or S 2 (‘holodiastolic’)?
occur from the onset of diastole (no gap between S 2 and murmur) but with a distinct gap between the end of the murmur and S 1 (early diastolic murmur)
begin later in diastole with a distinct gap between S 2 and the onset of the murmur (mid-diastolic murmur)?
Quality and pitch. This is somewhat subjective but ask yourself whether the murmur is:
a coarse or harsh sound akin to noises generated from the back of the mouth such as clearing the throat (typical of ejection systolic murmurs)?
a blowing sound akin to noises generated from the front of the mouth with lips parted such as an unsuccessful whistle (typical of regurgitant systolic murmurs)
a low-pitched, rumbling sound akin to noises generated from the back of the mouth with lips closed like a gentle growl (typical of mitral stenosis)?
Intensity. Ask yourself how easily the murmur is heard and whether there is an associated thrill then grade according to Box 4.17 .
Location and radiation. Ask yourself the following questions:
At what sites on the precordium is the murmur audible?
At what site is the murmur most easily heard/loudest?
Is the murmur audible at any other site, e.g. over the carotids or in the axilla?
The first heart sound (S 1 ), ‘lub’, is caused by closure of the mitral and tricuspid valves at the onset of ventricular systole. It is best heard at the apex. In mitral stenosis the intensity of S 1 is increased due to elevated left atrial pressure ( Box 4.18 ).
| Quiet | |
|
|
| Loud | |
|
|
| Variable | |
|
|
The second heart sound (S 2 ), ‘dub’, is caused by closure of the pulmonary and aortic valves at the end of ventricular systole and is best heard at the left sternal edge. It is louder and higher-pitched than the S 1 ‘lub’, and the aortic component is normally louder than the pulmonary component.
Physiological splitting of S 2 occurs because left ventricular contraction ends slightly before that of the right ventricle so that the aortic valve closes before the pulmonary valve. This splitting increases on inspiration (‘lub d-dub’) because increased venous filling of the right ventricle further delays pulmonary valve closure. The separation disappears on expiration (‘lub dub’; Fig. 4.19 ).
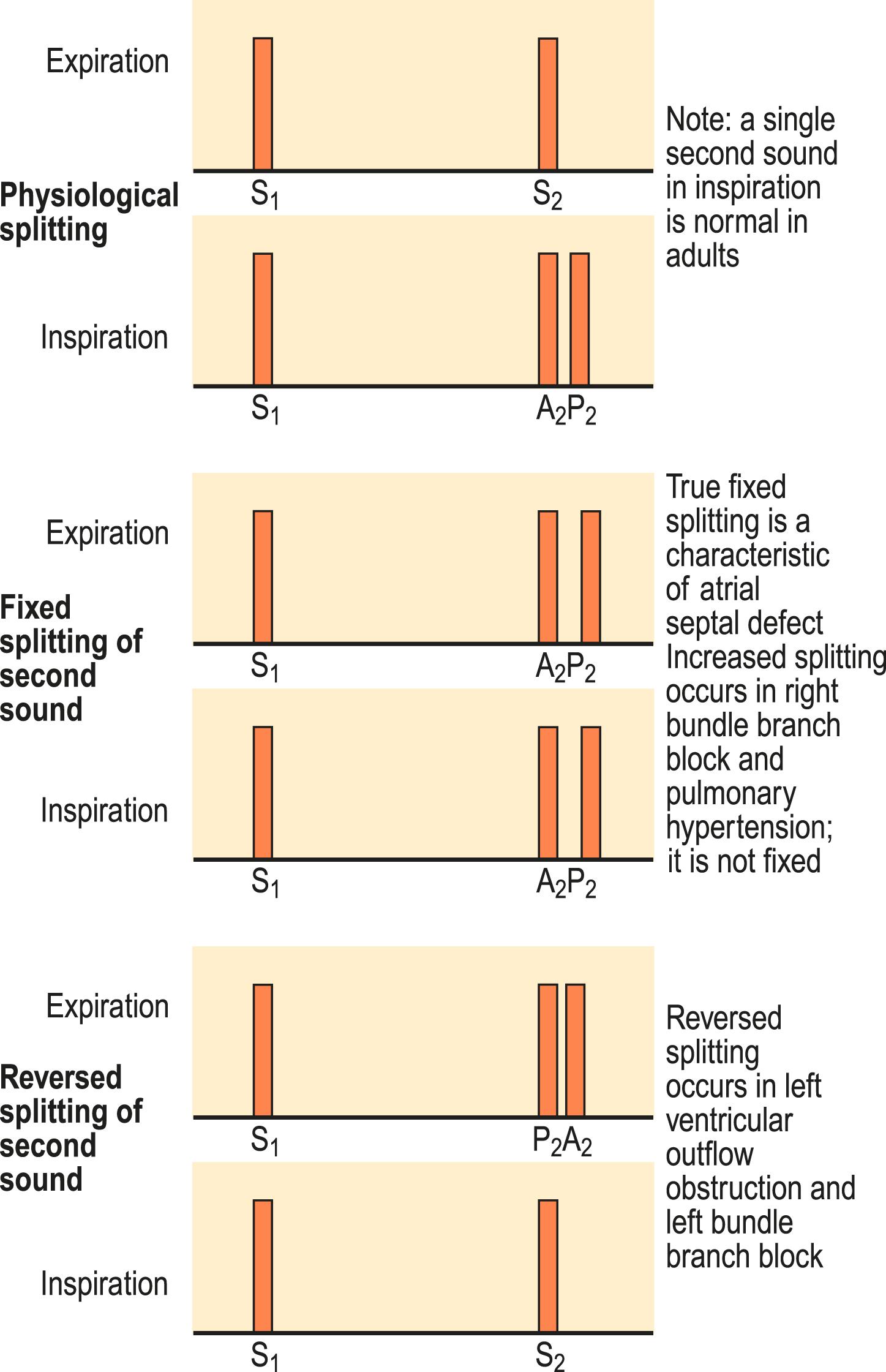
Wide splitting of S 2 , but with normal respiratory variation, occurs in conditions that delay right ventricular emptying, such as right bundle branch block or pulmonary hypertension. Wide and fixed splitting of S 2 , with no variation in respiration, is almost always due to an atrial septal defect ( Fig. 4.20 ). In this condition, shunting of blood from the left atrium to the right atrium causes right ventricular stroke volume to be significantly larger than the left throughout the respiratory cycle.
Reversed splitting of S 2 (‘lub dub’ on inspiration; ‘lub d-dub’ on expiration; Fig. 4.19 ) occurs when left ventricular emptying is delayed so that the aortic valve closes after the pulmonary valve. Examples include left bundle branch block and severe aortic stenosis.
The aortic component of S 2 is sometimes quiet or absent in calcific aortic stenosis. A loud pulmonary component of S 2 is an important sign of pulmonary hypertension.
The third heart sound (S 3 ) is a low-pitched early diastolic sound best heard with the bell at the apex. It results from a brief period of rapid ventricular filling immediately after opening of the atrioventricular valves and is therefore heard after the second heart sound as ‘lub dub-dum’. It may be a normal physiological finding in children and young adults or during fever or pregnancy. However, after the age of 40 years, it is usually due to left ventricular failure or mitral regurgitation, with the rapid ventricular filling a consequence of high left atrial pressure at the onset of diastole. In patients presenting to hospital with acute breathlessness, the presence of an S 3 , on examination, strongly increases the likelihood of heart failure but its absence does not help to rule out heart failure. In the context of heart failure, S 3 is typically accompanied by a tachycardia and referred to as a ‘gallop’ rhythm.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here