Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The modern female brow peak is closer to the lateral canthus than to the lateral limbus
In many patients the medial brow does not descend and may actually elevate with age
The shape of the upper lid crease in comparison to the superior orbital rim and the distance between these curves are important components of a person's apparent age
Avoid excess cautery, scalp excision, and subcutaneous sutures in surgical brow rejuvenation
Periosteal release is necessary, but temporal orbicularis release is essential
Bony fixation is usually not necessary if an extensive release is performed
Deep temporal fixation with absorbable sutures is all that is needed to maintain brow height in many patients
Avoid excess glabellar muscle manipulation
Overcorrect brow height
Be aware of neurologic deficit, do not be afraid of it; permanent motor damage is rare, and sensory deficit is common and is usually temporary
Postoperative dressings can increase periorbital edema and ecchymosis
Drains can decrease edema and bruising and provide a painless way to deliver bupivacaine after surgery in patients with excess pain
Botox is an excellent adjunct in the preoperative and postoperative period
Volumetric restoration of the temple and brow can achieve significant upper facial rejuvenation
The face is divided into horizontal thirds, with the upper third extending from the glabella to the trichion. In patients with a receding hairline, the uppermost point of action of the frontalis muscle is used instead.
The glabella is defined as the point of maximal anterior projection on lateral view.
The youthful brow region is full and convex with smooth skin and no creases.
On three-quarter view, the convex brow gently transitions into the concave lateral orbital wall to form the upper facial ogee .
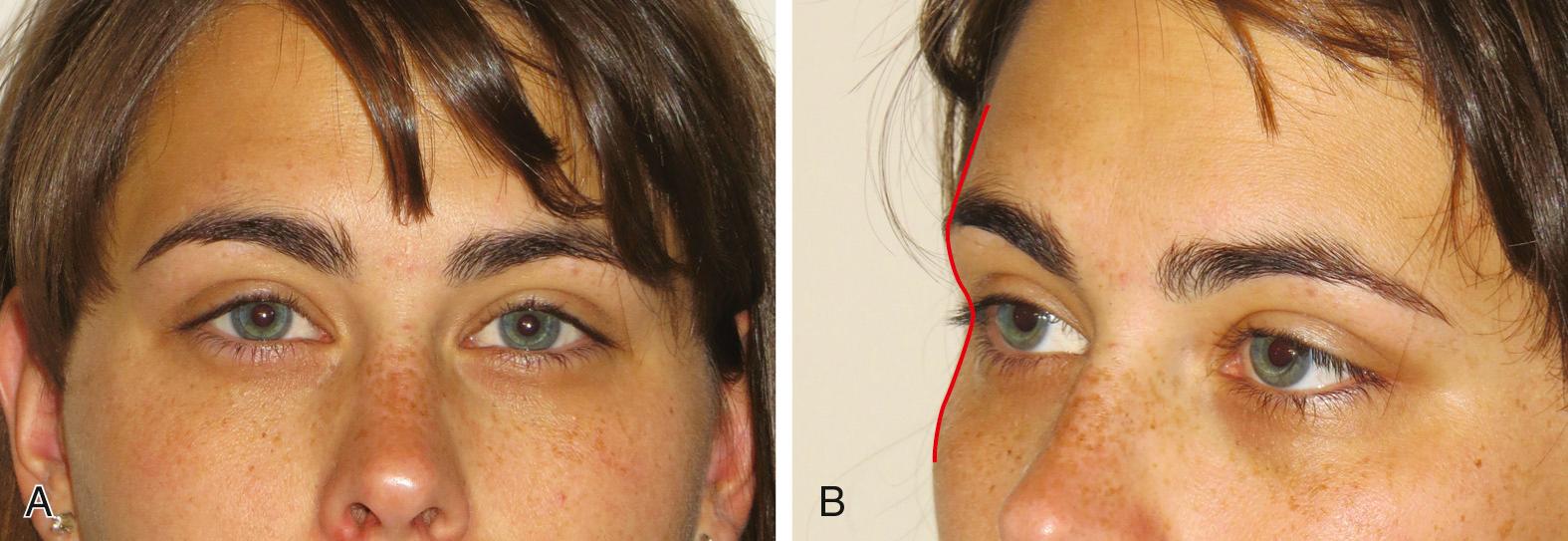
On frontal view, the temple is full and prevents visualization of the zygomatic arch or temporal line ( Fig. 25.1 ).
Brow fat span (BFS) and tarsal platform show (TPS) represent the distance between the upper eyebrow and upper lid crease and lid crease and upper eyelid margin, respectively; the youthful patient has a TPS:BFS ratio of 1 : 1.5 medially and 1 : 3 laterally ( Fig. 25.2 ).

Forehead has a smooth and gentle convexity on profile
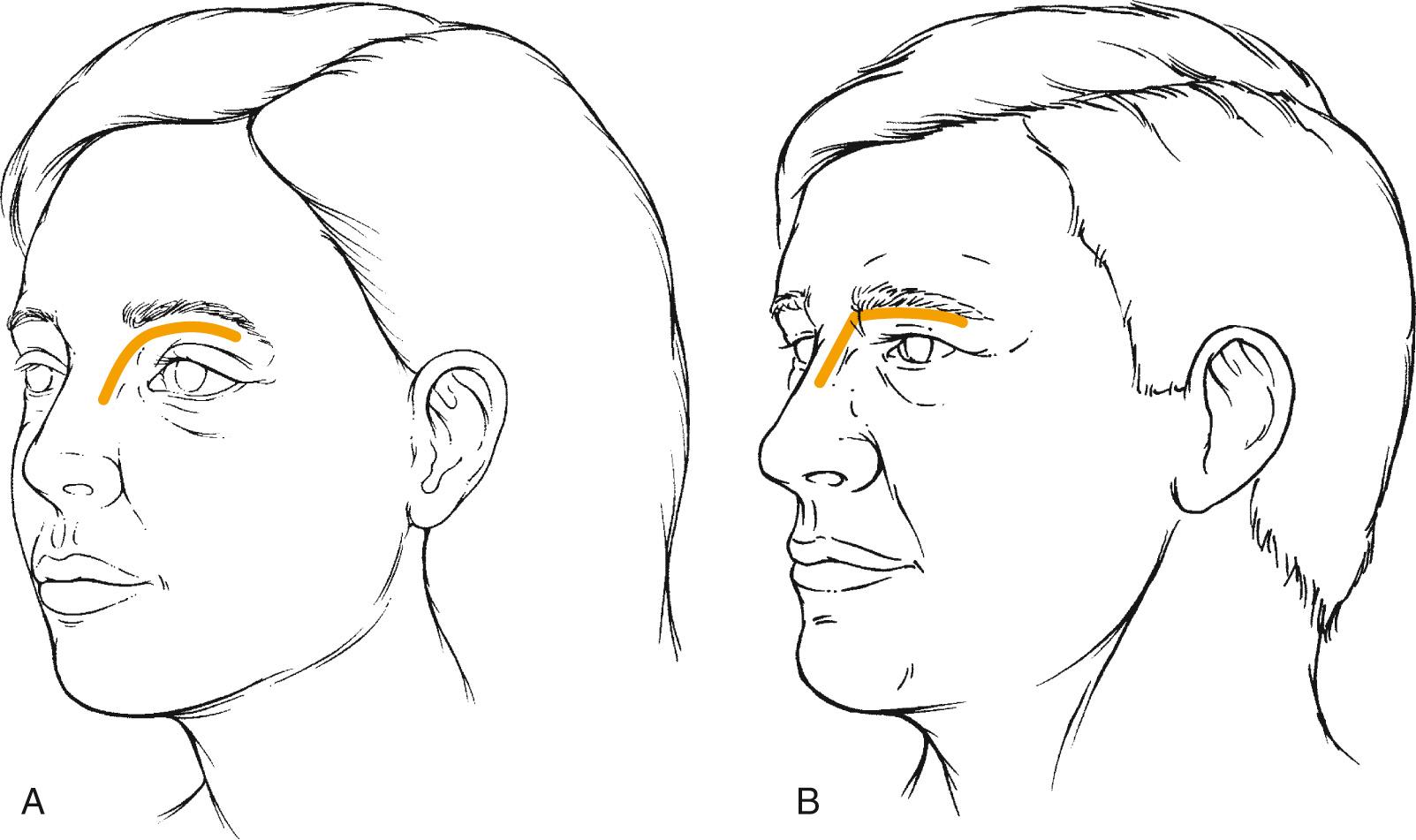
Eyebrows follow a smooth, gently curving arc that extends from the lateral eyebrow around the nasion and down the lateral nasal sidewall ( Fig. 25.3A )
Eyebrow should lie slightly above the supraorbital rim and follow a gently curving arc ( Fig. 25.4 ). The eyebrow begins at a line drawn from the alar-facial groove through the medial canthus and ends at a line drawn from the alar-facial groove through the lateral canthus.
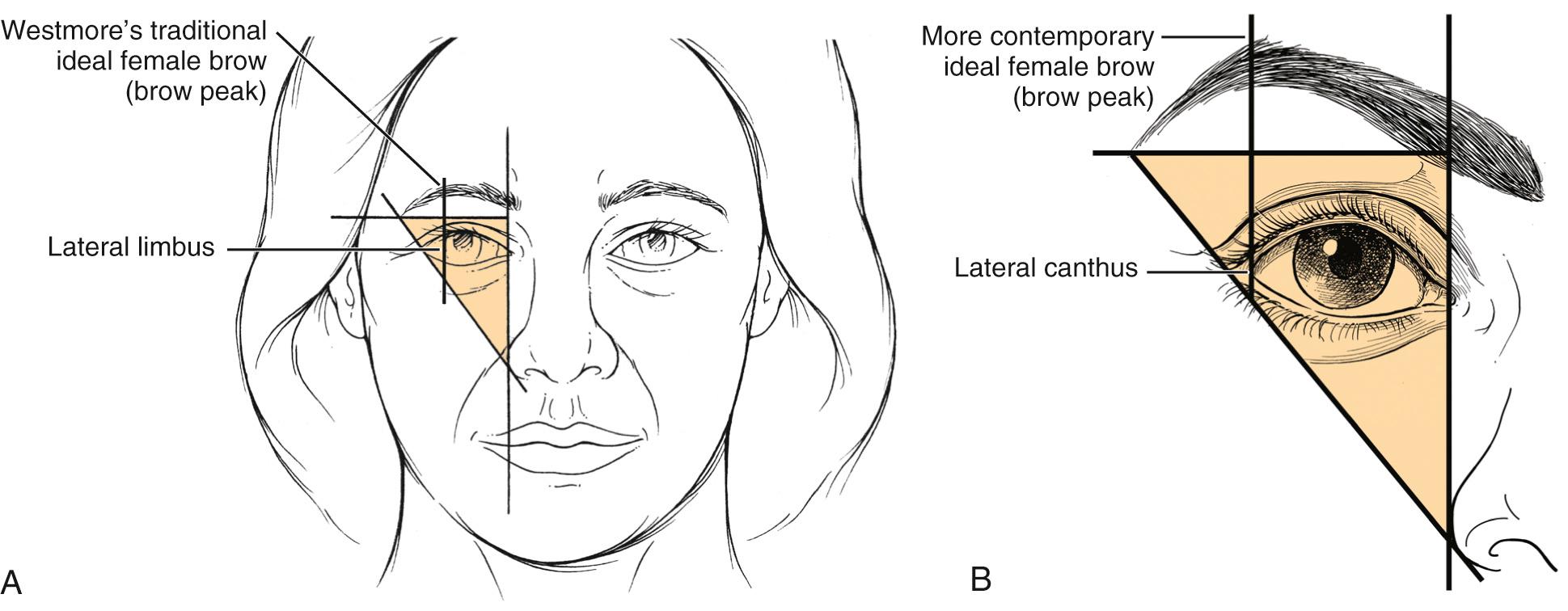
The modern ideal female brow has a peak above the lateral canthus.
The medial and lateral ends of the eyebrow should lie in a horizontal line, and the medial end should have a clublike configuration that gradually tapers laterally.
Forehead is less curved and broader than females
Eyebrow lies at the level of the supraorbital rim and is less arched (see Fig. 25.3B ).
Brow is thick and flat without lateral tapering
The forehead and periorbital muscles are key drivers of upper facial aging.
Orbicularis oculi muscle is superficial to the frontalis and acts as a middle and lateral brow depressor.
Medial brow depressors: paired procerus muscles, flanked laterally by the depressor supercilii and corrugator supercilii
The corrugator is the strongest brow depressor, has a transverse and oblique head, and causes the formation of deep vertical glabellar creases. It originates over the medial supraorbital ridge and inserts on the underside of the frontalis muscle.
Transverse glabellar creases (“bunny lines”) are formed by the procerus
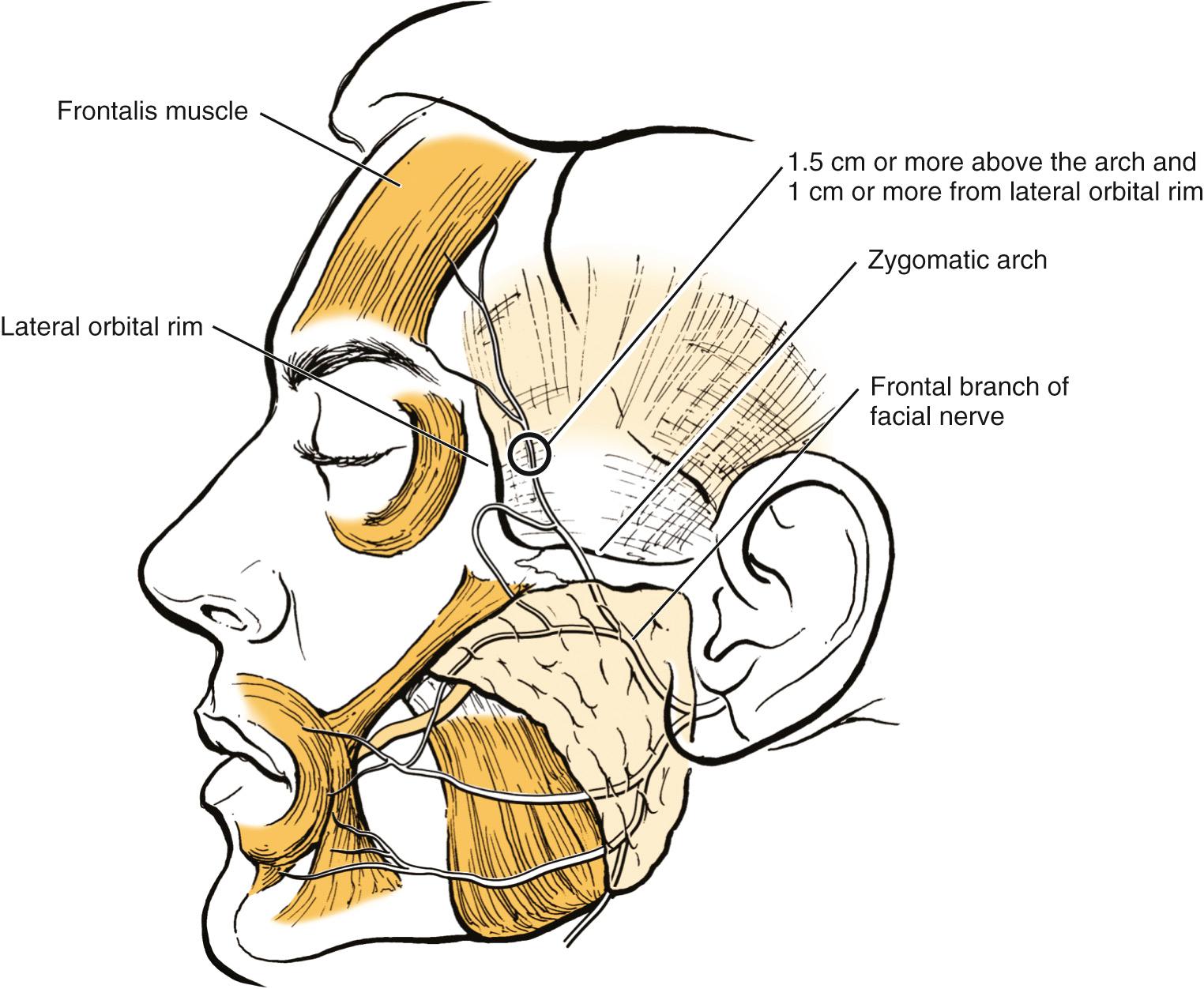
The frontalis is the primary brow elevator. The lateral margin of the frontalis muscle almost always ends along or just lateral to the temporal fusion line. The more medial the intersection, the less frontalis muscle there is to support the lateral brow; these individuals may be more prone to lateral brow ptosis.
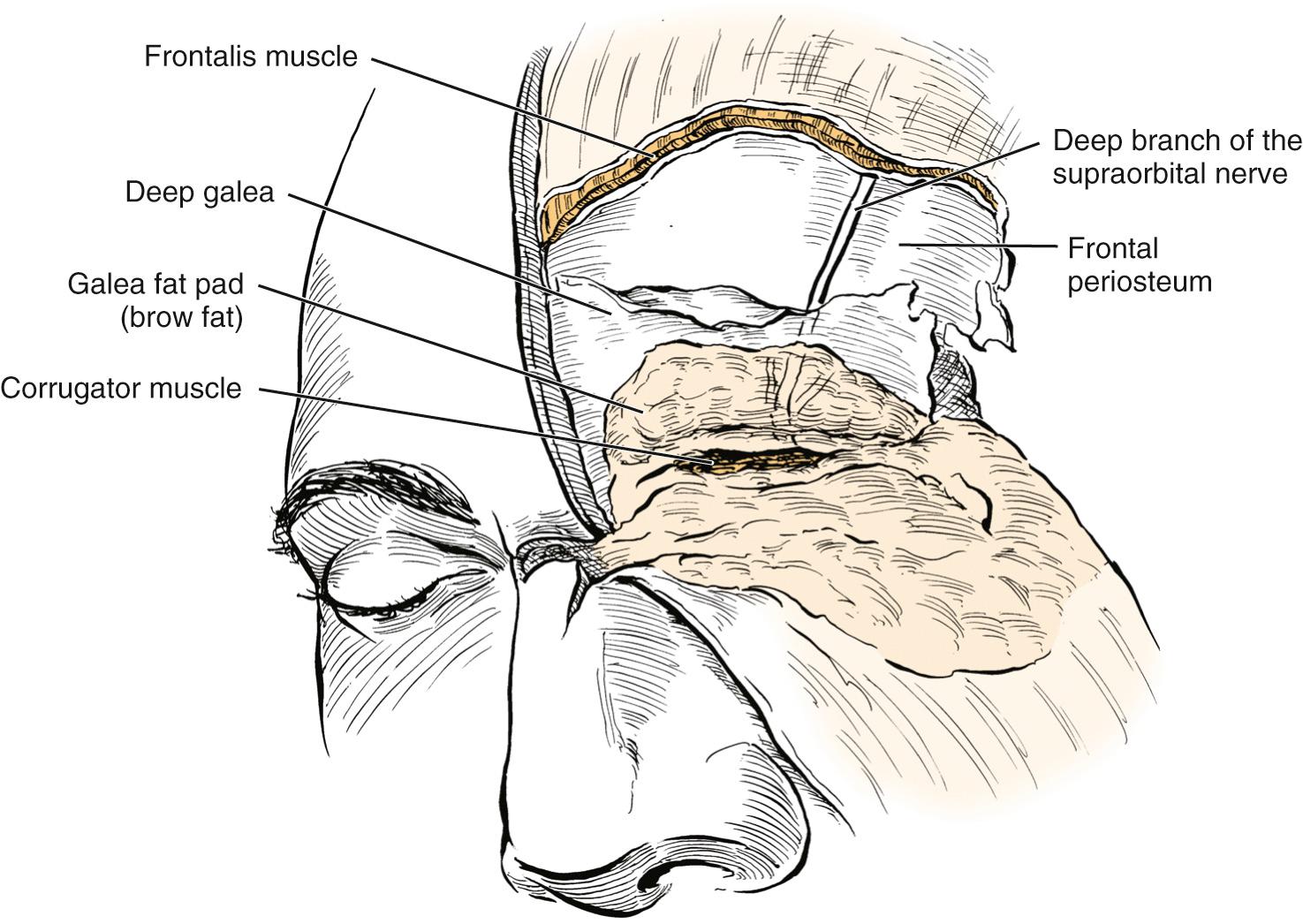
Thick forehead and brow skin abuts the very thin upper eyelid skin at the inferior edge of the eyebrow. Understanding the fascial layers of the brow region is critical, prior to performing surgery or volume augmentation in this area ( Fig. 25.5 ).
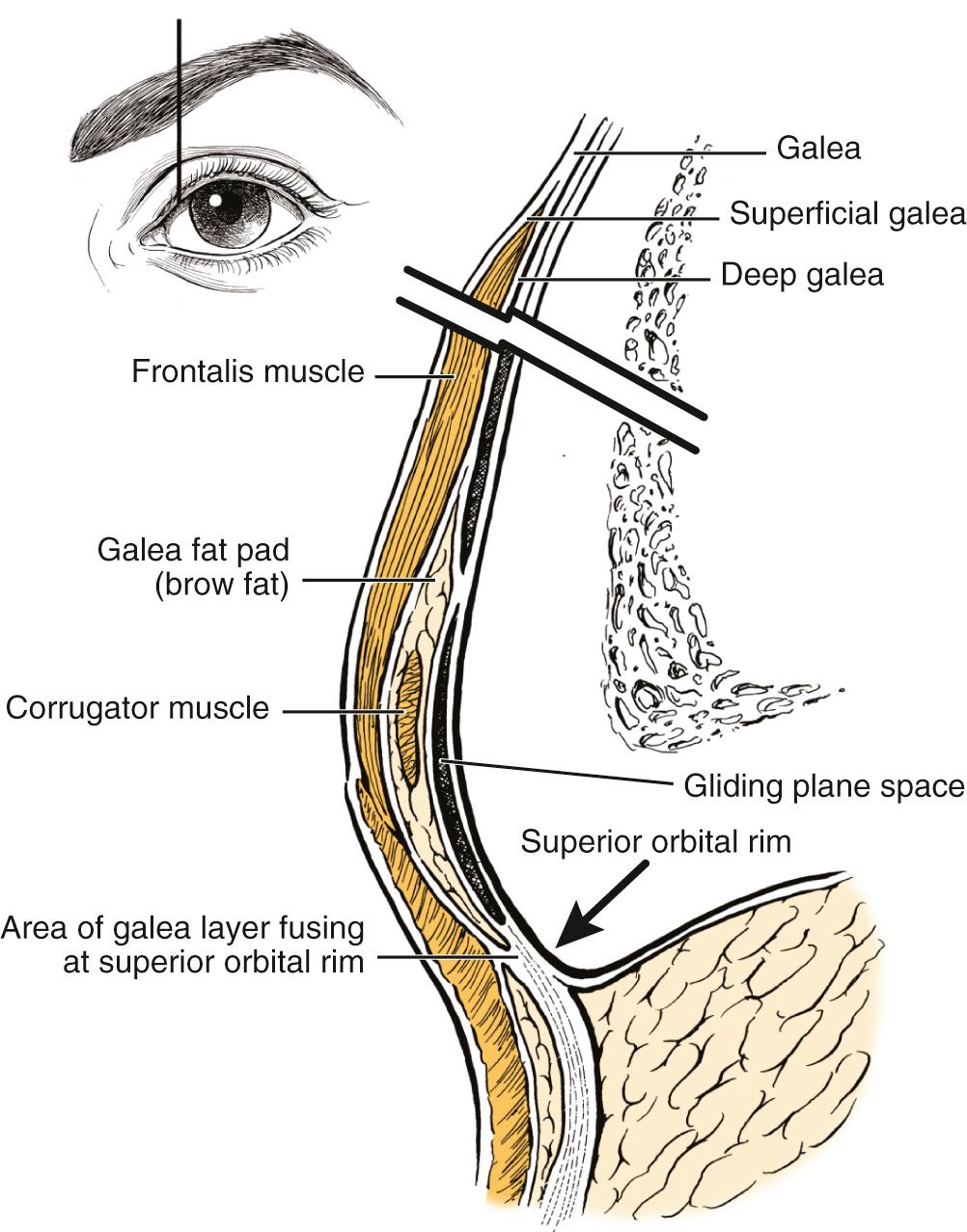
The galea aponeurotica splits to envelop the frontalis muscle and thus forms superficial and deep galea planes.
The deep galea plane splits to envelop the galea fat pad or brow fat pad.
The corrugator muscle travels within the galea fat pad.
The deep galea plane splits a third time to form the glide plane space deep to the corrugator, which contains only loose areolar tissue.
The deepest layer of the deep galeal fascia is adherent to the underlying periosteum.
The various layers of the deep galeal fascia typically rejoin and fuse at the orbital rim to form the suborbicularis fascia and orbital septum, which divide the preseptal and preaponeurotic fat in the upper lid. Knize identified individuals in whom the deep glabellar fascial layers did not rejoin at the orbital rim. In these individuals, the galea fat pad is not as well encapsulated or fixed and preaponeurotic fat could contribute to early brow ptosis.
The periorbital region is rich in true and false fascial retaining ligaments that pass perpendicularly and affix the skin to the underlying bone and deep fascia, respectively.
The orbicularis retaining ligament (ORL) is a membrane that extends from the suborbicular fascia to the periosteum, thereby stabilizing the orbicularis oculi muscle.
The ORL inserts 2 to 3 mm above the inferior edge of the supraorbital rim and divides the forehead from the upper eyelid. This is a critical anatomic point; materials injected above this point will augment the brow, whereas injections inferior to this point will enter the upper eyelid proper, which can damage the levator and create a contour irregularity.
The ORL extends over the zygoma as the lateral orbital thickening.
It should also be emphasized that the ORL “seal” at the boundary between the forehead and upper lid is incomplete around neurovascular structures. This is a possible mechanism whereby botulinum toxin can reach the levator and cause ptosis.
The supraorbital and supratrochlear branches of the ophthalmic division of the trigeminal nerve provide the primary sensory innervation to the forehead, upper lid, and brow.
The deep branch of the supraorbital nerve exits its foramen and turns posterolaterally to innervate the parietal scalp ( Fig. 25.6 ).
Travels just superficial to the periosteum and is at risk during brow-lifting if the subgaleal or subperiosteal layers of dissection are not respected.
Injury can cause intense pruritus leading to patients scratching their hair out.
The zygomaticotemporal nerve (maxillary division of the trigeminal nerve) contributes to temporal and lateral forehead sensation.
The facial nerve provides motor innervation to the forehead and periorbital musculature.
The frontal branch of the facial nerve innervates the frontalis muscle. Above the zygomatic arch and lateral to the frontalis, this nerve travels just deep to the temporoparietal fascia and is at risk during endoscopic and open brow-lifting procedures ( Fig. 25.7 ).
The orbicularis oculi, corrugator, procerus, and depressor supercilii are innervated by temporal and buccal branches that travel inferior to the eye.
The brow and forehead receive their blood supply primarily from the supraorbital and supratrochlear branches of the ophthalmic artery, from the internal carotid artery
The frontal branch of the superficial temporal artery contributes to lateral forehead blood supply.
Unilateral and even bilateral blindness caused by injection of fat and filler into the face and nose is a known complication, presumably caused by retrograde flow of particles leading to central retinal artery occlusion. The location of these blood vessels must be kept in mind at all times when performing injections in this region. Use of blunt cannulas and small syringes may reduce the risk of intravascular injection.
Traditional conceptions of brow aging focused on ptosis, so brow rejuvenation has historically revolved around brow-lifting techniques. We now know that the eyebrows remain in place or may even elevate with age.
Van den Bosch analyzed brow position, noting a higher lid crease (more TPS) and higher eyebrow position with increased age.
Goldberg and Lew have shown that the TPS increases medially and laterally.
Matros compared brow position in young women (ages 20 to 30 years) and older women (ages 50 to 60 years) and found that the lateral brow remains stable, whereas the middle and medial brow rise.
Lambros compared photographs of the same patients throughout their lives and found that the brow descended in 29%, remained stable in 30%, and was elevated in 41%.
A confounding variable in some of these studies is that upper lid dermatochalasis and involutional blepharoptosis are more common in older individuals, and both are known to cause eyebrow pseudoelevation.
Contemporary theories about upper facial aging emphasize that volume loss is as important as descent. The brow and deep temporal fat pads atrophy, and the normally thick brow skin becomes thinner and less elastic.
Brow skin lies flat against the underlying bone and creates shadows between the eyebrow and the upper eyelid crease.
The temple becomes concave, exposes the zygomatic arch, and causes shadows around the tail of the brow, which produces skeletonization and the impression of age.
Forehead aging is dominated by the formation of deep creases from the cumulative effect of periorbital muscle firing in combination with the loss of collagen and elastin from the skin.
Forehead aging manifests as a unique combination of ptosis, skin changes, and volume loss.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here