Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
The adrenal cortex produces three principal categories of steroid hormones that regulate a wide variety of physiologic processes from fetal to adult life. Mineralocorticoids, principally aldosterone, regulate renal retention of sodium and thus profoundly influence electrolyte balance, intravascular volume, and blood pressure. Glucocorticoids, principally cortisol, are named for their carbohydrate-mobilizing activity, but they are ubiquitous physiologic regulators, influencing a wide variety of bodily functions. Adrenal androgens serve no known physiologic role but do mediate some secondary sexual characteristics in women (e.g., pubic and axillary hair), and their overproduction may result in virilism. Thus the adrenal cortex is of considerable interest because of the widespread effects of its secretions and because derivatives of these secreted steroids are widely used as pharmacologic agents. Disorders of the adrenal cortex, once thought to be rare, are being recognized with increasing frequency. The severe congenital adrenal hyperplasias (CAHs) affect nearly 1 in 10,000 persons, and the very mild forms may affect as many as 1 in 100 in some populations. Cushing disease, once regarded as a true rarity in pediatrics, may affect as many children as adults. Primary aldosteronism is a common cause of hypertension, especially in adults.
The history of adrenal research has been reviewed recently. The adrenal glands apparently were first described in 1563 by the Italian anatomist Bartolomeo Eustaccio, better known for his description of the eustacian tube of the ear. Medical interest in the adrenals as something other than an anatomic curiosity began in the mid-19th century with Addison’s classical description of adrenal insufficiency and Brown-Sequard’s experimental creation of similar disorders in animals subjected to adrenalectomy. The signs and symptoms of glucocorticoid excess caused by adrenal tumors were well known by 1932, when Cushing described the pituitary tumors that cause what is now known as Cushing disease . Effects of adrenalectomy on salt and water metabolism were reported in 1927, Loeb showed that saline administration extended the life of Addisonian patients in 1933, and by the late 1930s, Selye had proposed the terms glucocorticoid and mineralocorticoid to distinguish the two broad categories of actions of adrenal extracts.
Numerous adrenal steroids were painstakingly isolated and their structures determined during the 1930s in the laboratories of Reichstein and Kendall. Many of these steroids were synthesized chemically, providing pure material for experimental purposes. In 1949 Kendall and Hench reported that glucocorticoids ameliorated the symptoms of rheumatoid arthritis, greatly stimulating interest in synthesizing new pharmacologically active analogues of naturally occurring steroids. Kendall, Reichstein, and Hench shared the 1950 Nobel Prize in Medicine. The structures of the various adrenal steroids suggested precursor/product relationships, leading in 1950 to the first treatment of CAH with cortisone by both Wilkins and Bartter. This opened a vigorous era of clinical investigation of the pathways of steroidogenesis in a variety of inherited adrenal and gonadal disorders. The association of cytochrome P450 with 21-hydroxylation was made in 1965, and some of the steroidogenic enzymes were then isolated in the 1970s, but it was not until the genes for most of these enzymes were cloned in the 1980s that it became clear which proteins participated in which steroidal transformations. The identification of these genes ( Table 14.1 ) then led to an understanding of the genetic lesions causing heritable disorders of steroidogenesis. At the same time, studies of steroid hormone action led to the discovery of steroid hormone receptors in the 1960s, but it was not until they were cloned in the 1980s that their biology has begun to be understood.
| Enzyme | Gene | Gene Size (kb) | Chromosomal Location | Exons (n) | mRNA Size (kb) |
|---|---|---|---|---|---|
| StAR | STAR | 8 | 8p11.2 | 8 | 1.6 |
| P450scc | CYP11A1 | 30 | 15q23–q24 | 9 | 2 |
| P450c11β | CYP11B1 | 9.5 | 8q21–22 | 9 | 4.2 |
| P450c11AS | CYP11B2 | 9.5 | 8q21–22 | 9 | 4.2 |
| P450c17 | CYP17A1 | 6.6 | 10q24.3 | 8 | 1.9 |
| P450c21 | CYP21A2 | 3.4 | 6p 21.1 | 10 | 2 |
| P450aro | CYP19A1 | 130 | 15q21.1 | 10 | 1.5–4.5 |
| 3βHSD1 | HSD3B1 | 8 | 1p13.1 | 4 | 1.7 |
| 3βHSD2 | HSD3B2 | 8 | 1p13.1 | 4 | 1.7 |
| 11βHSD1 | HSD11B1 | 7 | 1q32–q41 | 6 | 1.6 |
| 11βHSD2 | HSD11B2 | 6.2 | 16q22 | 5 | 1.6 |
| 17βHSD1 | HSD17B1 | 3.3 | 17q11–q21 | 6 | 1.4, 2.4 |
| 17βHSD2 | HSD17B2 | 63 | 16q24.1–q24.2 | 5 | 1.5 |
| 17βHSD3 | HSD17B3 | 67 | 9q22 | 11 | 1.2 |
| 17βHSD6 (RODH) | HSD17B6 | 24.5 | 12q13 | 5 | 1.6 |
| AKR1C1 | AKR1C1 | 14.3 | 10p14–p15 | 9 | 1.2 |
| AKR1C2 | AKR1C2 | 13.8 | 10p14–p15 | 9 | 1.3 |
| AKR1C3 | AKR1C3 | 13 | 10p14–p15 | 9 | 1.2 |
| AKR1C4 | AKR1C4 | 22.1 | 10p14–p15 | 9 | 1.2 |
| 5α-Reductase 1 | SRD5A1 | 36 | 5p15 | 5 | 2.4 |
| 5α-Reductase 2 | SRD5A2 | 56 | 2p23 | 5 | 2.4 |
| SULT2A1 | SULT2A1 | 17 | 19q13.3 | 6 | 2 |
| PAPSS2 | PAPSS2 | 85 | 10q24 | 13 | 3.9 |
| P450 Oxidoreductase | POR | 69 | 7q11.2 | 16 | 2.5 |
| Ferredoxin | FDX1 | 35 | 11q22 | 5 | 1.0, 1.4, 1.7, 3.2 |
| Ferredoxin Reductase | FDXR | 11 | 17q24–q25 | 12 | 2 |
| Cytochrome b 5 | CYB5A | 32 | 18q23 | 5 | 0.9 |
| H6PDH | H6PD | 36.5 | 1p36 | 5 | 9 |
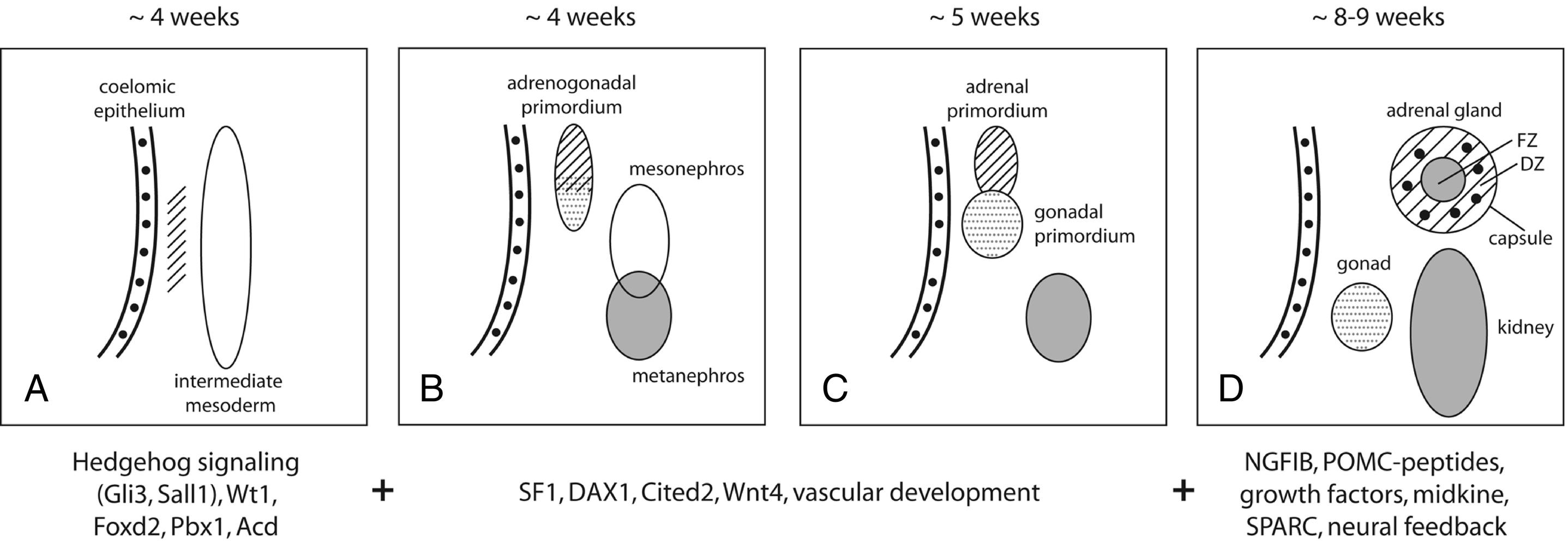
The cells of the adrenal cortex are of mesodermal origin, in contrast to cells of the adrenal medulla, which are derived from the neuroectoderm. In human embryos, adrenogonadal progenitor cells first appear at around the fourth week of gestation as a thickening of the coelomic epithelium (or intermediate mesoderm) between the urogenital ridge and dorsal mesentery ( Fig. 14.1 ). These progenitor cells give rise to the steroidogenic cells of the gonads and to the adrenal cortex. The adrenal and gonadal cells then separate, with the adrenal cells migrating retroperitoneally to the cranial pole of the mesonephros and the gonadal cells migrating caudally. Between the seventh and eighth week of development, the adrenal primordium is invaded by sympathetic cells derived from the neural crest that give rise to the adrenal medulla. By the end of the eighth week, the rudimentary adrenal has become encapsulated and is clearly associated with the upper pole of the kidney, which at this time is much smaller than the adrenal.
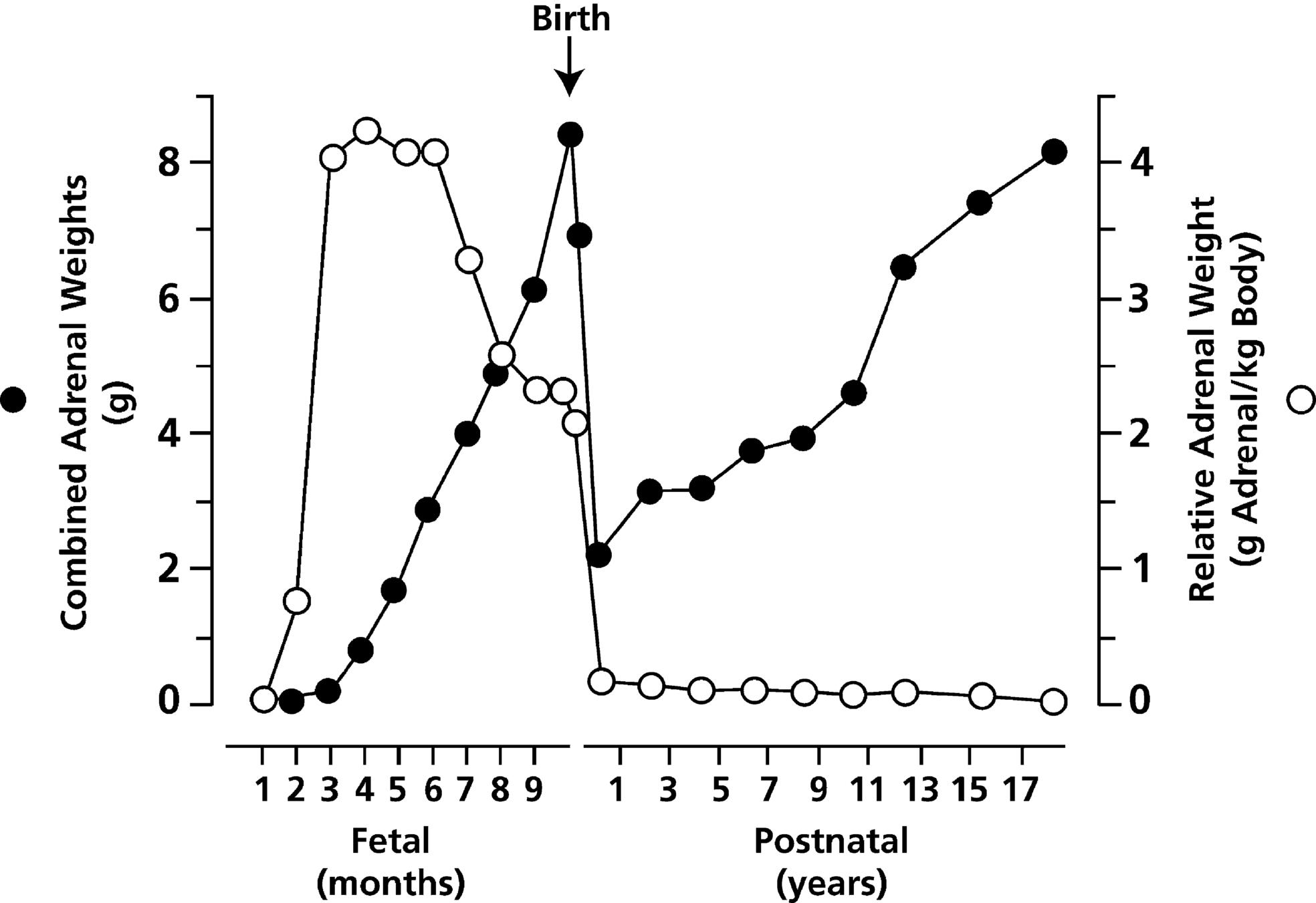
The fetal adrenal cortex consists of an outer “definitive” zone, the principal site of glucocorticoid and mineralocorticoid synthesis, and a much larger “fetal” zone that makes androgenic precursors (dehydroepiandrosterone [DHEA], dehydroepiandrosterone sulfate [DHEAS]) that the placenta converts to estriol. A putative “transitional” zone exists between these regions toward the end of fetal development, but its role is unclear. The fetal adrenal glands are huge in proportion to other structures, and continue to grow well into the third trimester ( Fig. 14.2 ). At birth, the adrenals weigh 8 to 9 g, about the same size of adult adrenals, and represent approximately 0.4% of total body weight. Following birth, cells of the fetal zone undergo apoptosis, and the fetal adrenal zone rapidly involutes and has virtually disappeared by 6 to 12 months of postnatal life. Thereafter adrenal growth is comparatively slow, so that the adrenal glands represent only 0.01% of body weight in the adult.
The complex mechanisms regulating adrenal development are still relatively poorly understood. However, important insight into key factors has been obtained from studies of transgenic mice and from patients with disorders of adrenal development. For example, the early stages of adrenal differentiation and development involve a number of signaling pathways (hedgehog/GLI3, WNT3/WNT4/WNT11, midkine), transcription factors (SALL1, FOXD2, PBX1, WT1, SF1 [NR5A1], DAX1 [NR0B1]), coregulators (CITED2), matrix proteins (SPARC), and regulators of telomerase activity (ACD). Subsequent fetal adrenal growth is highly dependent on the trophic effects of adrenocorticotropic hormone (ACTH), its receptor (MC2R), and its downstream signaling pathways, as well as growth factor signaling pathways, such as insulin-like growth factor-2 (IGF-2), basic fibroblast growth factor (bFGF, now termed FGF2 ), and epidermal growth factor (EGF).
The adrenals, once termed suprarenal glands , derive their name from their anatomic location, sitting on top of the upper pole of each kidney. Unlike most other organs, the arteries and veins serving the adrenal do not run parallel. Arterial blood is provided by several small arteries arising from the renal and phrenic arteries, the aorta, and sometimes the ovarian and left spermatic arteries. The veins are more conventional, with the left adrenal vein draining into the left renal vein and the right adrenal vein draining directly into the vena cava. Arterial blood enters the sinusoidal circulation of the cortex and drains toward the medulla, so that medullary chromaffin cells are bathed in very high concentrations of steroid hormones. High concentrations of cortisol are required for expression of medullary phenylethanolamine-N-methyltransferase, which converts norepinephrine to epinephrine, linking the adrenal cortical and medullary responses to stress.
The adrenal cortex consists of three histologically recognizable zones: the zona glomerulosa is immediately below the capsule, the zona fasciculata is in the middle, and the zona reticularis lies next to the medulla. The glomerulosa, fasciculata, and reticularis, respectively, constitute about 15, 75, and 10% of the adrenal cortex of the older child and adult. These zones appear to be distinct functionally, as well as histologically, but considerable overlap exists, and immunocytochemical data show that the zones physically interdigitate. After birth, the large fetal zone begins to involute and disappears by about 3 to 6 months of age. The definitive zone simultaneously enlarges, but two of the adult zones, the glomerulosa and fasciculata, are not fully differentiated until about 3 years of age, and the reticularis may not be fully differentiated until about 15 years of age. The origin of the distinct adrenocortical zones and the mechanisms that regulate their proliferation are still poorly understood. One model suggests that a population of undifferentiated stem cells exists between the zona glomerulosa and zona fasciculata, which represents a pool of common precursor cells that can contribute to either the inner or outer zones. In contrast, the “centripetal migration” theory proposes that a subcapsular population of progenitor/stem cells first differentiates into cells of the zona glomerulosa, which then convert into zona fasciculata cells (and presumably later into zona reticularis cells), as they migrate centripetally toward the adrenal medulla, where they complete their life span and undergo apoptosis.
Much is now known about steroid biosynthesis, and about the early steps in the intracellular cholesterol trafficking. The human adrenal can synthesize cholesterol de novo from acetate, but most of its supply of cholesterol comes from plasma low-density lipoproteins (LDLs) derived from dietary cholesterol. Rodent adrenals derive most of their cholesterol from high-density lipoproteins via a receptor termed SR-B1 , but this pathway plays a minor role in human steroidogenesis. Adequate concentrations of LDL will suppress 3-hydroxy-3-methylglutaryl co-enzyme A (HMG-CoA) reductase, the rate-limiting enzyme in cholesterol synthesis. ACTH, which stimulates adrenal steroidogenesis, also stimulates the activity of HMG-CoA reductase, LDL receptors, and uptake of LDL cholesterol. LDL cholesterol esters are taken up by receptor-mediated endocytosis, then are stored directly or converted to free cholesterol and used for steroid hormone synthesis. Cholesterol can be esterified by acyl-CoA:cholesterol transferase (ACAT), stored in lipid droplets, and accessed by activation of hormone-sensitive lipase (HSL) and by the so-called NPC proteins, which derive their name from their causative role in Niemann-Pick type C disease. ACTH stimulates HSL and inhibits ACAT, thus increasing the availability of free cholesterol for steroid hormone synthesis.
Most steroidogenic enzymes are cytochrome P450 enzymes. “Cytochrome P450” designates a group of oxidative enzymes, all of which have about 500 amino acids and contain a single heme group. “P450” means “pigment 450” because all absorb light at 450 nm in their reduced states. Human beings have 57 genes for P450 enzymes; seven human P450s are targeted to mitochondria and 50 are targeted to the endoplasmic reticulum, especially in the liver, where they metabolize countless toxins, drugs, xenobiotics, and environmental pollutants. Each P450 enzyme, including the steroidogenic P450s, can metabolize multiple substrates, catalyzing a broad array of oxidations.
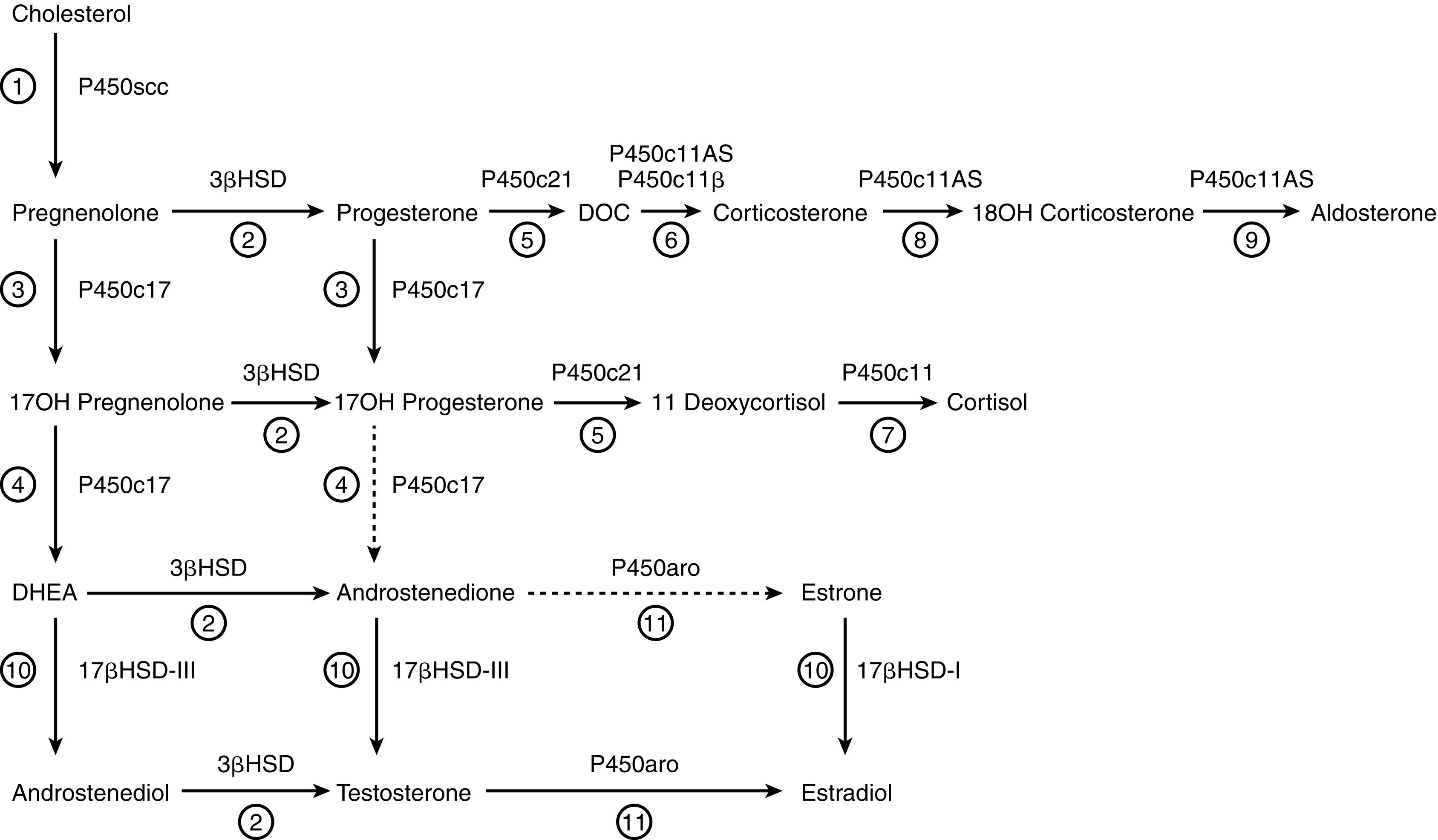
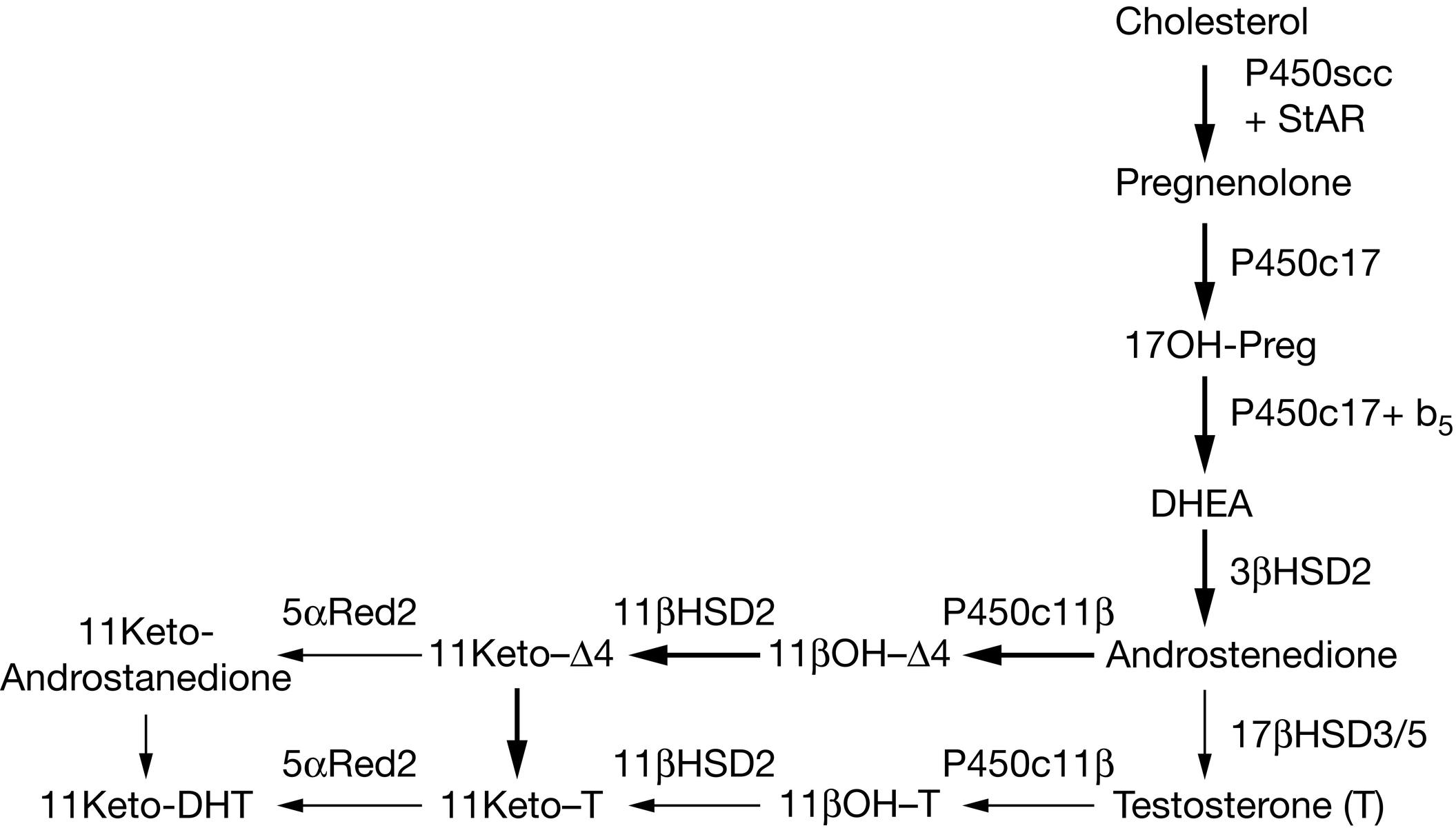
Five P450s are involved in adrenal steroidogenesis ( Fig. 14.3 ). Mitochondrial P450scc (CYP11A1) is the cholesterol side-chain cleavage enzyme catalyzing the series of reactions formerly termed 20,22 desmolase . The two mitochondrial isozymes of P450c11, P450c11β (CYP11B1) and P450c11AS (CYP11B2), catalyze 11β-hydroxylase, 18-hydroxylase, and 18-methyl oxidase activities. P450c17 (CYP17A1), found in the endoplasmic reticulum, catalyzes both 17α-hydroxylase and 17,20 lyase activities, and P450c21 (CYP21A2) catalyzes the 21-hydroxylation of both glucocorticoids and mineralocorticoids. In the gonads and elsewhere P450aro (CYP19A1) in the endoplasmic reticulum catalyzes aromatization of androgens to estrogens.
The hydroxysteroid dehydrogenases (HSDs) have molecular masses of about 35 to 45 kDa, do not have heme groups, and require nicotinamide adenine dinucleotide (NAD + ) or nicotinamide adenine dinucleotide phosphate (NADP + ) as cofactors. Whereas most steroidogenic reactions mediated by P450 enzymes are catalyzed by a single form of P450, each of the reactions mediated by HSDs can be catalyzed by at least two isozymes. The HSDs include the 3α- and 3β-hydroxysteroid dehydrogenases, two 11β-hydroxysteroid dehydrogenases, and a series of 17β-hydroxysteroid dehydrogenases; the 5α-reductases are unrelated to this family. Based on their structures, the HSDs fall into two groups: the short-chain dehydrogenase/reductase (SDR) family, structurally characterized by a “Rossman fold,” and the aldo-keto reductase (AKR) family, characterized by a triosephosphate isomerase barrel motif. The SDR enzymes include 11β-HSDs 1 and 2, and 17β-HSDs 1, 2, 3, and 4; the AKR enzymes include 17β-HSD5, which is important in extraglandular activation of androgenic precursors, and the 3α-hydroxysteroid dehydrogenases that participate in the so-called backdoor pathway of fetal androgen synthesis (see later). Based on their activities, it is physiologically more useful to classify them as dehydrogenases or reductases. The dehydrogenases use NAD + as their cofactor to oxidize hydroxysteroids to ketosteroids, and the reductases mainly use NADPH to reduce ketosteroids to hydroxysteroids. Although these enzymes are typically bidirectional in vitro, they tend to function in only one direction in intact cells, with the direction determined by the cofactor(s) available.
Conversion of cholesterol to pregnenolone in mitochondria is the first, rate-limiting and hormonally regulated step in the synthesis of all steroid hormones. This involves cholesterol 20α-hydroxylation, 22-hydroxylation, and scission of its side chain to yield pregnenolone and isocaproic acid. Because 20-hydroxycholesterol, 22-hydroxycholesterol, and 20,22-hydroxycholesterol could be isolated from adrenals in significant quantities, it was previously thought that three separate enzymes were involved. However, a single protein, termed P450scc (‘scc’ refers to the s ide- c hain c leavage of cholesterol) encoded by the CYP11A1 gene on chromosome 15 catalyzes all the steps between cholesterol and pregnenolone. Deletion of the mouse or rabbit cyp11a1 gene eliminates all steroidogenesis, indicating that all steroidogenesis is initiated by this one enzyme.
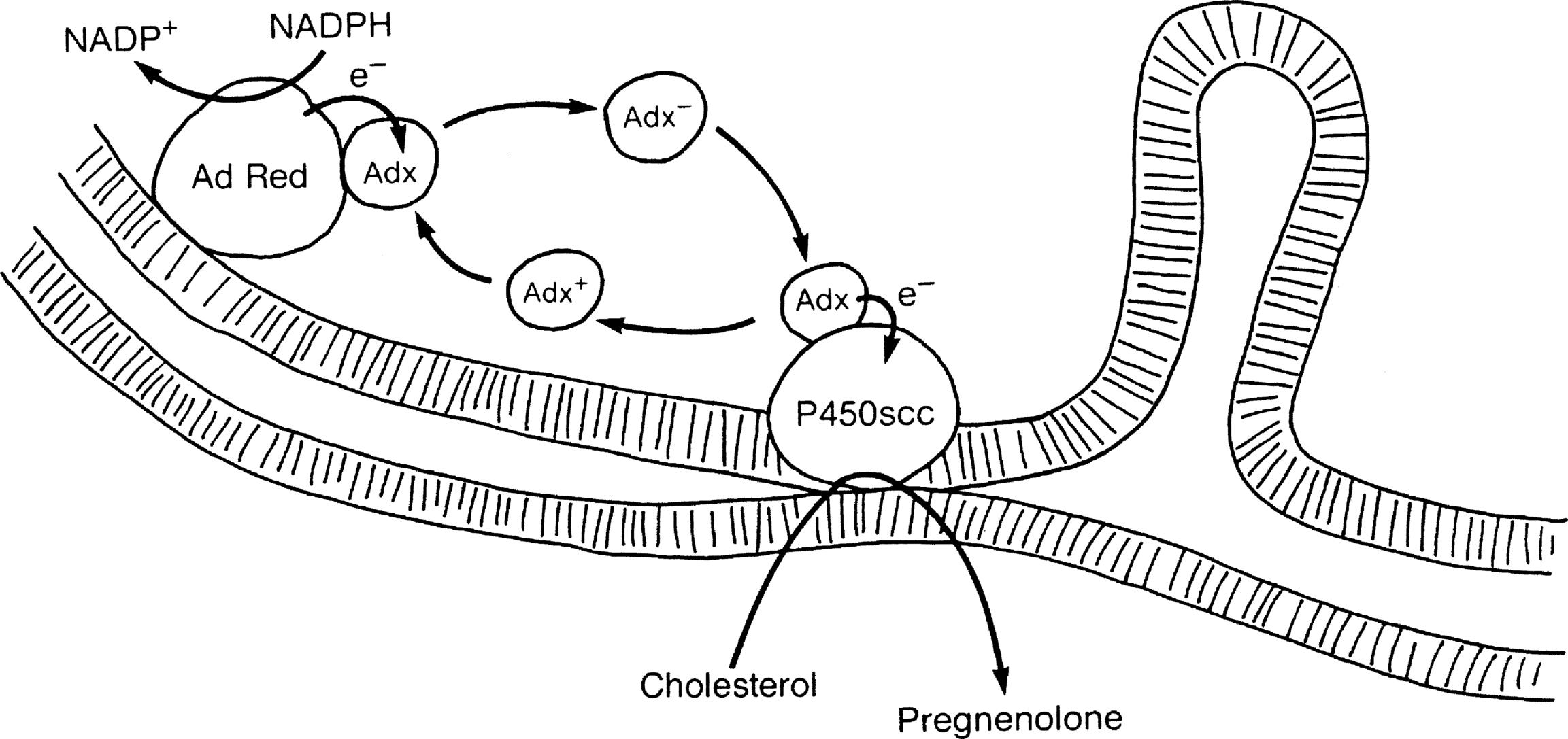
Mitochondrial P450 enzymes (P450scc, P450c11β, P450c11AS, and the vitamin D 1α- and 24-hydroxylases) are terminal oxidases in an electron transport system: NADPH donates electrons to ferredoxin reductase (FDXR, also termed adrenodoxin reductase ), a flavoprotein that is loosely associated with the inner mitochondrial membrane. FDXR transfers the electrons to ferredoxin (FDX, also termed adrenodoxin ), a 14-kDa iron/sulfur protein, which then transfers the electrons to P450scc ( Fig. 14.4 ). FDX forms a 1:1 complex with FDXR, dissociates, then reforms an analogous 1:1 complex with the P450, thus functioning as a diffusible electron shuttle mechanism. FDXR and FDX are widely expressed in human tissues, but FDXR expression is two orders of magnitude higher in steroidogenic tissues. The primary ribonucleic acid (RNA) transcript from the FDXR gene is alternatively spliced yielding two messenger RNA (mRNA) species that encode proteins differing by six amino acids, but only the shorter protein is active in steroidogenesis. FDXR is also essential in the formation of the iron/sulfur centers used by many enzymes. There are two human FDX isozymes encoded by genes on different chromosomes: FDX1 interacts with mitochondrial P450 enzymes; FDX2 is used for synthesis of iron-sulfur clusters, but not for steroidogenesis. FDX1 is ubiquitously expressed but is especially abundant in adrenal cortex. Human mutations in FDX have not been described, but several FDXR mutations that partially impair formation of iron/sulfur centers are associated with neuropathic hearing loss.
ACTH regulates steroidogenic capacity (chronic regulation) by inducing the transcription of genes for steroidogenic enzymes, but acute regulation, where steroids are released within minutes of a stimulus, is at the level of cholesterol access to P450scc. Treating either steroidogenic cells or intact rats with inhibitors of protein synthesis (e.g., cycloheximide) eliminated the acute steroidogenic response, suggesting that a short-lived protein triggers the response. A long search led to the identification and cloning of the steroidogenic acute regulatory protein, StAR. The central role of StAR in steroidogenesis was proven by finding that mutations of StAR caused congenital lipoid adrenal hyperplasia. Thus StAR is the acute trigger that is required for the rapid flux of cholesterol from the outer to the inner mitochondrial membrane that is needed for the acute response of aldosterone to angiotensin II, of cortisol to ACTH, and of sex steroids to a luteinizing hormone (LH) pulse.
Some adrenal steroidogenesis is independent of StAR; this StAR-independent steroidogenesis is about 14% of the StAR-induced rate. The placenta uses P450scc to initiate steroidogenesis but does not express StAR. The mechanism of StAR-independent steroidogenesis is unclear; it may occur without a triggering protein, or some other protein may exert StAR-like activity to promote cholesterol flux, but without StAR's rapid kinetics. The mechanism of StAR's action is unclear, but it is established that StAR acts on the outer mitochondrial membrane (OMM), does not need to enter the mitochondria to be active, and undergoes conformational changes on the OMM that are required for StAR’s activity. Some studies suggest that StAR functions as a component of a molecular machine that consists of StAR, TSPO (the translocator protein formerly known as the peripheral benzodiazepine receptor), and other proteins on the OMM, although studies with TSPO-knockout mice question its role. The precise fashion in which cholesterol is loaded into the OMM and moves from the OMM to P450scc with the assistance of StAR remains unclear, and remains under active investigation.
Once pregnenolone is produced from cholesterol, it may undergo 17α-hydroxylation by P450c17 to yield 17-hydroxypregnenolone (17-Preg), or it may be converted to progesterone. Two 42-kDa isozymes of 3β-hydroxysteroid dehydrogenase (3βHSD), encoded by the HSD3B1 and HSD3B2 genes, can catalyze both conversion of the hydroxyl group to a keto group on carbon 3 and the isomerization of the double bond from the B ring (Δ 5 steroids) to the A ring (Δ 4 steroids). These isozymes share 93.5% amino acid sequence identity and are enzymatically very similar: both can convert pregnenolone to progesterone, 17-Preg to 17α-hydroxyprogesterone (17OHP), DHEA to androstenedione, and androstenediol to testosterone. However, 3βHSD2, the isozyme expressed in the adrenals and gonads, has a high Michaelis-Menten constant (Km) of about 5.5 μM, about 10 times higher than 3βHSD1 expressed in placenta, brain, and “extraglandular” tissues. The low Km of extraglandular 3βHSD1 permits it to act on the low concentrations of some steroids found in the circulation. Ultrastructural data show that 3βHSD can be found in the mitochondria, endoplasmic reticulum, and cytoplasm. It is not clear if this subcellular distribution differs in various types of steroidogenic cells, but this could be a novel point regulating the direction of steroidogenesis.
P450c17 (CYP17A1) catalyzes both 17α-hydroxylase and 17,20-lyase activities. The 17α-hydroxylase activity of P450c17 can convert pregnenolone to 17-Preg and progesterone to 17OHP. The 17,20-lyase activity of P450c17 can convert 17-Preg to DHEA, but very little 17OHP is converted to androstenedione because human P450c17 catalyzes this reaction at only around 2% to 3% of the rate for conversion of 17-Preg to DHEA. P450c17 is the key branch point in steroid hormone synthesis: in its absence, as in the adrenal zona glomerulosa, 17α-hydroxylase and 17,20-lyase activities are absent, so that pregnenolone is converted to mineralocorticoids; in the presence of its 17α-hydroxylase activity in the zona fasciculata, only the 17α-hydroxylase activity is present so that pregnenolone is sequentially converted to cortisol; in the zona reticularis where both activities are present, pregnenolone is sequentially converted to sex steroids (see Fig. 14.3 ).
17α-Hydroxylase and 17,20 lyase were once thought to be separate enzymes. The adrenals of prepubertal children synthesize ample cortisol but virtually no DHEA (i.e., have 17α-hydroxylase activity but not 17,20 lyase activity) until adrenarche initiates production of adrenal androgens (i.e., turns on 17,20 lyase activity). Furthermore, patients had been described lacking 17,20 lyase activity but retaining normal 17α-hydroxylase activity. However, both 17α-hydroxylase and 17,20 lyase activities reside in the same active site, and cells transfected with a vector expressing P450c17 acquire both 17α-hydroxylase and 17,20 lyase activities. P450c17 is encoded by the CYP17A1 gene on chromosome 10q24.3, and is structurally related to the CYP21A2 gene for P450c21 (21-hydroxylase). Thus the distinction between 17α-hydroxylase and 17,20 lyase is functional and not genetic or structural. Human P450c17 catalyzes 17α-hydroxylation of pregnenolone and progesterone equally well, but its 17,20 lyase activity uses 17-Preg almost exclusively, and not 17OHP, consistent with the large amounts of DHEA secreted by both the fetal and adult adrenal. The principal factor regulating the 17,20 lyase reaction is electron transport from NADPH via P450 oxidoreductase (POR).
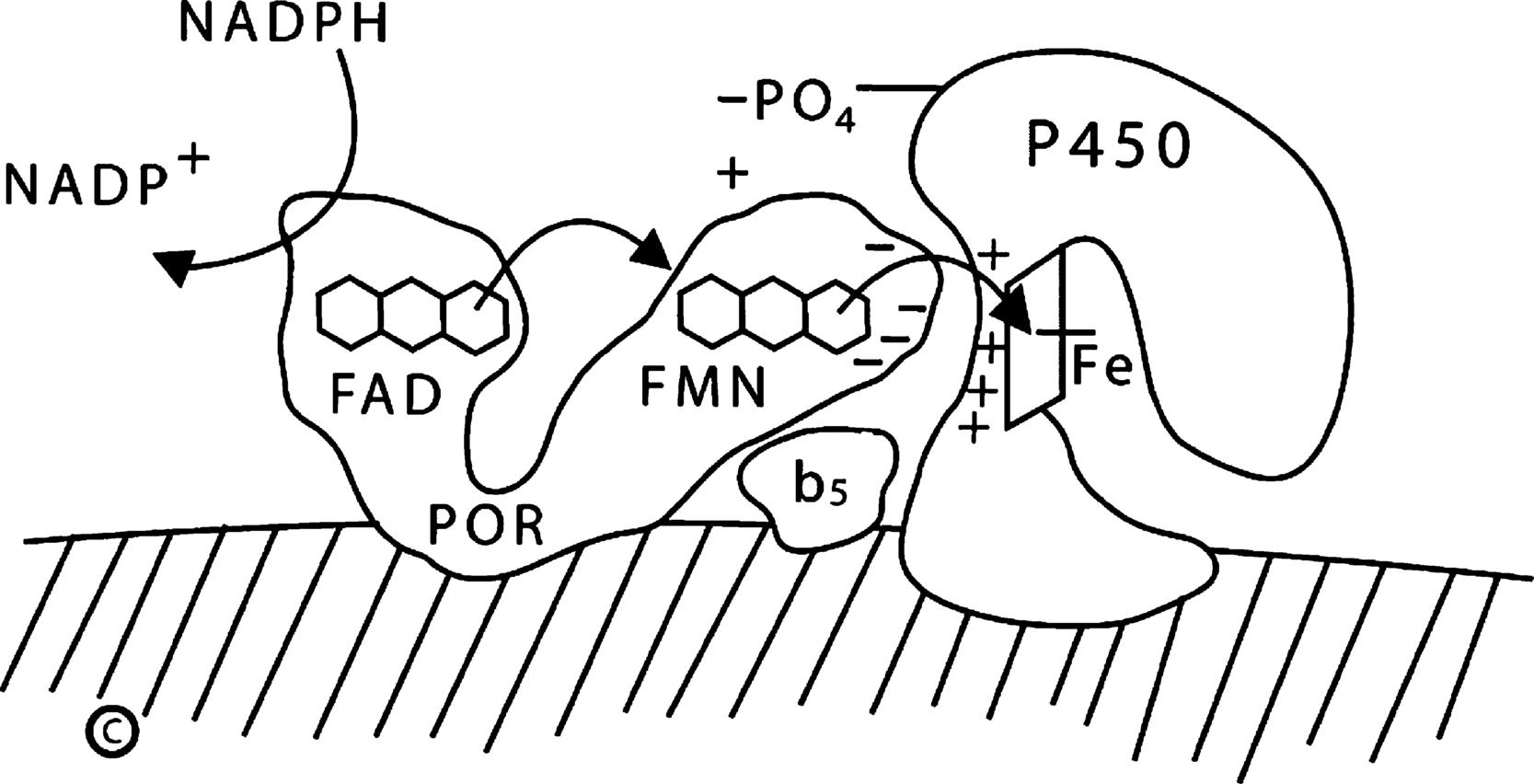
POR, a membrane-bound flavoprotein that is unrelated to mitochondrial ferredoxin reductase, receives electrons from NADPH and transfers them to the 50 microsomal forms of cytochrome P450, including P450c17, P450c21, and P450aro. For the 17,20 lyase reaction of P450c17, electron transfer is facilitated by the action of cytochrome b 5 , acting as an allosteric factor rather than as an alternate electron donor; 17,20 lyase activity is also increased by the serine/threonine phosphorylation of P450c17 by p38α, a cyclic adenosine monophosphate (cAMP)-dependent protein kinase ( Fig. 14.5 ). Thus the availability of electrons determines whether P450c17 performs only 17α-hydroxylation, or also performs 17,20 bond scission: increasing the ratio of POR or cytochrome b 5 to P450c17 increases the ratio of 17,20 lyase activity to 17α-hydroxylase activity. Thus the regulation of 17,20 lyase activity, and consequently of DHEA production, depends on factors that facilitate the flow of electrons to P450c17: high concentrations of POR, the presence of cytochrome b 5 , and serine phosphorylation of P450c17.
After the synthesis of progesterone and 17OHP, these steroids are 21-hydroxylated to yield deoxycorticosterone (DOC) and 11-deoxycortisol, respectively (see Fig. 14.3 ). The nature of the 21-hydroxylating step is of great interest because disordered 21-hydroxylation causes more than 90% of all cases of CAH. The clinical findings in CAH are complex and potentially devastating. Decreased cortisol and aldosterone synthesis often lead to sodium loss, potassium retention, acidosis, and hypotension, which will lead to cardiovascular collapse and death, usually within a month after birth if not treated appropriately. Decreased adrenal steroidogenesis in utero leads to overproduction of adrenal androgens via several pathways (see later), resulting in severe prenatal virilization of female fetuses. Adrenal 21-hydroxylation is catalyzed by P450c21 found in smooth endoplasmic reticulum, using POR to receive electrons from NADPH. Duplicated CYP21A1P and CYP21A2 genes lie on chromosome 6p21, but only the human CYP21A2 gene encodes P450c21. As this gene lies in the middle of the major histocompatibility locus, disorders of adrenal 21-hydroxylation are closely linked to specific human leukocyte antigen (HLA) types. Extraadrenal 21-hydroxylase activity is found in many adult and fetal tissues, especially in the liver, but is catalyzed by other enzymes, notably CYP2C19 and CYP3A4, which are principally involved in drug metabolism. CYP2C19 and CYP3A4 can 21-hydroxylate progesterone but not 17OHP, and hence may contribute to the synthesis of mineralocorticoids but not glucocorticoids.
The closely related P450c11β and P450c11AS enzymes catalyze the final steps in the synthesis of glucocorticoids and mineralocorticoids. These two isozymes have 93% amino acid sequence identity and are encoded by tandemly duplicated genes on chromosome 8q21-22. Like P450scc, the two forms of P450c11 are found on the inner mitochondrial membrane, and use ferredoxin and ferredoxin reductase to receive electrons from NADPH. By far the more abundant of the two isozymes is P450c11β (encoded by CYP11B1 ), which is the classic 11β-hydroxylase that converts 11-deoxycortisol to cortisol and 11-deoxycorticosterone to corticosterone. The less abundant isozyme, P450c11AS (encoded by CYP11B2 ), is found only in the zona glomerulosa, where it has 11β-hydroxylase, 18-hydroxylase, and 18-methyl oxidase (aldosterone synthase) activities; thus P450c11AS is able to catalyze all the reactions needed to convert DOC to aldosterone. CYP11B1 is induced by ACTH via cAMP and is suppressed by glucocorticoids; CYP11B2 is induced by angiotensin II and K + . Patients with mutations in CYP11B1 have classic 11β-hydroxylase deficiency but can still produce aldosterone, whereas patients with mutations in CYP11B2 have rare forms of aldosterone deficiency (so-called corticosterone methyl oxidase deficiency ), while retaining the ability to produce cortisol.
Androstenedione is converted to testosterone, DHEA is converted to androstenediol, and estrone is converted to estradiol by the 17β-hydroxysteroid dehydrogenases (17βHSD; HSD17B), sometimes also termed 17-oxidoreductases or 17-ketosteroid reductases . The terminologies for these enzymes vary, depending on the direction of the reaction being considered. The literature about the 17βHSDs can be confusing because (1) there are several different 17βHSDs; (2) some are preferential oxidases, whereas others are preferential reductases; (3) they differ in their substrate preference and sites of expression; (4) the nomenclature is inconsistent; and (5) some proteins termed 17βHSD actually have very little 17βHSD activity, and are principally involved in other reactions.
Type 1 17βHSD (17βHSD1, encoded by HSD17B1 ), is a 34-kDa reductive, estrogenic SDR enzyme expressed in ovarian granulosa cells (where it produces estradiol) and placenta (where it produces estriol). 17βHSD1 uses NADPH as its cofactor, acts as a dimer, and only accepts steroid substrates with an aromatic A ring, so that its activity is confined to activating estrogens. No genetic deficiency syndrome for 17βHSD1 has been described.
17βHSD2 is a microsomal oxidase that uses NAD + to inactivate estradiol to estrone and testosterone to Δ 4 androstenedione. 17βHSD2 is found in the placenta, liver, small intestine, prostate, secretory endometrium, and ovary. Whereas 17βHSD1 is found in placental syncytiotrophoblast cells, 17βHSD2 is expressed in endothelial cells of placental intravillous vessels, consistent with its apparent role in defending the fetal circulation from transplacental passage of maternal estradiol or testosterone. No deficiency state for 17βHSD2 has been reported.
Microsomal 17βHSD3 is the principal androgenic form of 17βHSD, apparently expressed only in the testis. This enzyme is disordered in the classic syndrome of male pseudohermaphroditism that is often termed 17-ketosteroid reductase deficiency .
An enzyme termed 17βHSD4 was initially identified as an NAD + -dependent oxidase with activities similar to 17βHSD2, but this peroxisomal protein is primarily an enoyl-CoA hydratase and 3-hydroxyacyl-CoA dehydrogenase. Deficiency of 17βHSD4 causes a form of Zellweger syndrome, in which bile acid biosynthesis is disturbed but steroidogenesis is not.
17βHSD5, originally cloned as a 3α-hydroxysteroid dehydrogenase, is an AKR enzyme (whereas 17βHSD types 1-4 are SDR enzymes) termed AKR1C3 that catalyzes the reduction of Δ 4 androstenedione to testosterone. The 17βHSD activity of 17βHSD5 is quite labile in vitro, and this enzyme catalyzes different activities under different conditions. The adrenal zona reticularis expresses this enzyme at low levels, accounting for the small amount of testosterone produced by the adrenal.
17βHSD6, encoded by the HSD17B6 gene on chromosome 12q13.3, is also known as RoDH for its homology to retinol dehydrogenases. 17βHSD6 is expressed at low but detectable levels in the fetal testes, where it appears to catalyze oxidative 3αHSD activities in the so-called “backdoor pathway” to dihydrotestosterone (DHT) synthesis.
Steroid sulfates may be synthesized directly from cholesterol sulfate or may be formed by sulfation of steroids by cytosolic sulfotransferase (SULT) enzymes. SULTs use 3’-phosphoadenine-5’-phosphosulfate (PAPS) as sulfate donor, synthesized from adenosine triphosphate (ATP) and sulfate by two isozymes of PAPS synthase: PAPSS1, which is ubiquitously expressed, and PAPSS2, principally expressed in cartilage, adrenal, and liver. At least 44 distinct isoforms of these enzymes have been identified belonging to five families of SULT genes; many of these genes yield alternately spliced products accounting for the large number of enzymes. The SULT enzymes that sulfonate steroids include SULT1E (estrogens), SULT2A1 (nonaromatic steroids), and SULT2B1 (sterols). SULT2A1 is the principal sulfotransferase expressed in the adrenal, where it sulfates the 3β hydroxyl group of Δ 5 steroids (pregnenolone, 17OH-pregnenolone, DHEA, androsterone) but not cholesterol. SULT2B1a will also sulfonate pregnenolone but not cholesterol, whereas cholesterol is the principal substrate for SULT2B1b in the skin, liver, and elsewhere. It is not clear whether most steroid sulfates are simply inactivated forms of steroid or if they serve specific hormonal roles. Knockout of the mouse sult1e1 gene is associated with elevated estrogen levels, increased placental expression of tissue factor, and increased platelet activation, leading to placental thrombi and fetal loss that could be ameliorated by anticoagulant therapy. Mutations ablating the function of human SULT enzymes have not been described, but PAPSS2 mutations deplete adrenal PAPS, increasing production of unconjugated DHEA. African Americans have a high rate of polymorphisms in SULT2A1, apparently influencing plasma ratios of DHEA:DHEAS, which may correlate with risk of prostatic and other cancers.
Steroid sulfates may also be hydrolyzed to the native steroid by steroid sulfatase. Deletions in the steroid sulfatase gene on chromosome Xp22.3 cause X-linked ichthyosis. The fact that males have a single copy of this gene probably accounts for males having higher DHEAS levels than females of the same age. In the fetal adrenal and placenta, diminished or absent sulfatase deficiency reduces the pool of free DHEA available for placental conversion to estrogen, resulting in low concentrations of estriol in the maternal blood and urine. The accumulation of steroid sulfates in the stratum corneum of the skin causes the ichthyosis.
Estrogens are produced by the aromatization of androgens, including adrenal androgens, by a complex series of reactions catalyzed by aromatase, P450aro. This microsomal cytochrome P450 is encoded by a single gene ( CYP19A1 ) on chromosome 15q21.1 that uses several different promoter sequences, transcriptional start sites, and alternatively chosen first exons to encode identical P450aro in different tissues under different hormonal regulation. Aromatase expression in the extraglandular tissues, especially adipose tissue, can convert adrenal androgens to estrogens. Aromatase in the epiphyses of growing bone converts testosterone to estradiol; the tall stature, delayed epiphyseal maturation and osteopenia of males with aromatase deficiency, and their rapid reversal with estrogen replacement indicate that estrogen, not androgen, is responsible for epiphyseal maturation in males.
Rare patients with aromatase deficiency illustrate that placental aromatase activity and consequent feto-placental estrogen synthesis are not needed for normal fetal development. However, in the absence of placental aromatase activity, fetal adrenal androgens and androgen precursors pass into the maternal circulation, causing maternal virilization. Furthermore, placental aromatase converts maternal androgens to estrogens, protecting the fetus from potential virilization (as in pregnant women with undertreated 21-hydroxylase deficiency [21OHD]). Children with aromatase deficiency grow normally and continue to grow after puberty, because only estrogens, not androgens, mediate epiphyseal fusion. Treating aromatase-deficient patients with estrogens will fuse their epiphyses and arrest growth. These observations underlie the use of aromatase inhibitors for inhibiting accelerated bone maturation.
Testosterone is converted to the more potent androgen, DHT, by 5α-reductase, an enzyme found in testosterone’s target tissues. There are two hydrophobic, 30-kDa isozymes of 5α-reductase that share 50% identity. The type I enzyme, found in the scalp and other peripheral tissues, is encoded by the SRD5A1 gene on chromosome 5; the type II enzyme, the predominant form found in male reproductive tissues, is encoded by the structurally related SRD5A2 gene on chromosome 2p23. The syndrome of 5α-reductase deficiency, a disorder of male sexual differentiation, is caused by a wide variety of mutations in the SRD5A2 gene. In the fetus, the SRD5A1 gene is expressed in the testis, then is expressed briefly in the skin of the newborn, and then remains unexpressed until its activity and protein are again found after puberty. The SRD5A2 gene is expressed in fetal genital skin, in the normal prostate, and in prostatic hyperplasia and adenocarcinoma. Thus the type I enzyme may be responsible for the pubertal virilization seen in patients with classic 5α-reductase deficiency, and the type II enzyme may be involved in male pattern baldness.
Although certain steroids are typically categorized as glucocorticoids or mineralocorticoids, the “mineralocorticoid” (glucocorticoid type II) receptor has equal affinity for both aldosterone and cortisol. Nevertheless, cortisol does not act as a mineralocorticoid in vivo, even though cortisol concentrations can exceed aldosterone concentrations by 100- to 1000-fold, because mineralocorticoid responsive tissues (such as the kidney) convert cortisol to cortisone, a metabolically inactive steroid. The interconversion of cortisol and cortisone is mediated by two membrane-bound isozymes of 11β-hydroxysteroid dehydrogenase (11βHSD; HSD11B), each of which can catalyze both oxidase and reductase activity, depending on the cofactor available (NADP + or NADPH). The ratio of NADP + to NADPH is regulated by hexose-6-phosphate dehydrogenase (H6PDH).
The type 1 enzyme (HSD11B1; 11βHSD1) is expressed mainly in glucocorticoid-responsive tissues, such as the liver, fat, testis, and lung. HSD11B1 can catalyze both the oxidation of cortisol to cortisone using NADP + as its cofactor (Km 1–2 μM), or the reduction of cortisone to cortisol using NADPH as its cofactor (Km 0.1–0.3 μM); the reaction catalyzed depends on which cofactor is available, but the enzyme can only function with high (micromolar) concentrations of steroid. HSD11B1 is located on the luminal side of the endoplasmic reticulum, and hence is not in contact with the cytoplasm, permitting HSD11B1 to receive NADPH provided by H6PDH. This links HSD11B1 to the pentose monophosphate shunt, providing a direct paracrine link between local glucocorticoid production and energy storage as fat. Prednisone and cortisone are inactive 11-ketosteroids that must be reduced to their active 11β-hydroxy derivatives by HSD11B1, mainly in the liver. By activating cortisone, HSD11B1 amplifies glucocorticoid action in the tissues in which it is expressed, especially in liver and fat, potentially contributing to obesity, insulin resistance, metabolic syndrome, and possibly nonalcoholic fatty liver disease; consequently, studies of HSD11B1 inhibitors are of substantial pharmaceutic interest.
HSD11B2 (11βHSD2) catalyzes the oxidation of cortisol to cortisone using NADH, and can function with low (nanomolar) steroid concentrations (Km 10–100 nM). HSD11B2 is expressed in mineralocorticoid-responsive tissues, such as the distal nephron and thus serves to “defend” the mineralocorticoid receptor (MR) by inactivating cortisol to cortisone, so that only “true” mineralocorticoids, such as aldosterone or deoxycorticosterone, can exert a mineralocorticoid effect; thus HSD11B2 prevents cortisol from overwhelming renal MRs. Placental HSD11B2 also inactivates maternal cortisol to cortisone (and prednisolone to prednisone), and the placenta has abundant NADP + favoring the oxidative action of HSD11B1, so that in the placenta both enzymes protect the fetus from high maternal concentrations of cortisol, but not from maternally administered beta-methasone or dexamethasone, which are not substrates for HSD11B enzymes. Thus the HSD11B isozymes determine whether a steroid “crosses the placenta.”
The 3α-hydroxysteroid dehydrogenases (3αHSDs) are not familiar to most endocrinologists, but are clinically important because of the recent discovery of the “backdoor pathway” of steroidogenesis. This remarkable pathway ( Fig. 14.6 ), first discovered as the mechanism by which the male marsupial fetal testis makes androgens, plays a central role in human male sexual differentiation. In this pathway, 17OHP is converted to DHT without going through DHEA, androstenedione, or testosterone, and hence provides a mechanism for 17OHP to contribute to the virilization of female fetuses with 21OHD. The reductive 3αHSDs are AKR enzymes and the oxidative 3αHSDs are SDR enzymes. There are four reductive 3αHSDs, termed AKR1C4-1. These enzymes are structurally very similar, are encoded by a cluster of very similar genes on chromosome 10p14-15, and catalyze a wide array of steroidal conversions (notably 17-ketosteroid reduction and 20α-reduction) and other reactions. AKR1C3, also known as 17βHSD5, converts androstenedione to testosterone in the adrenal.
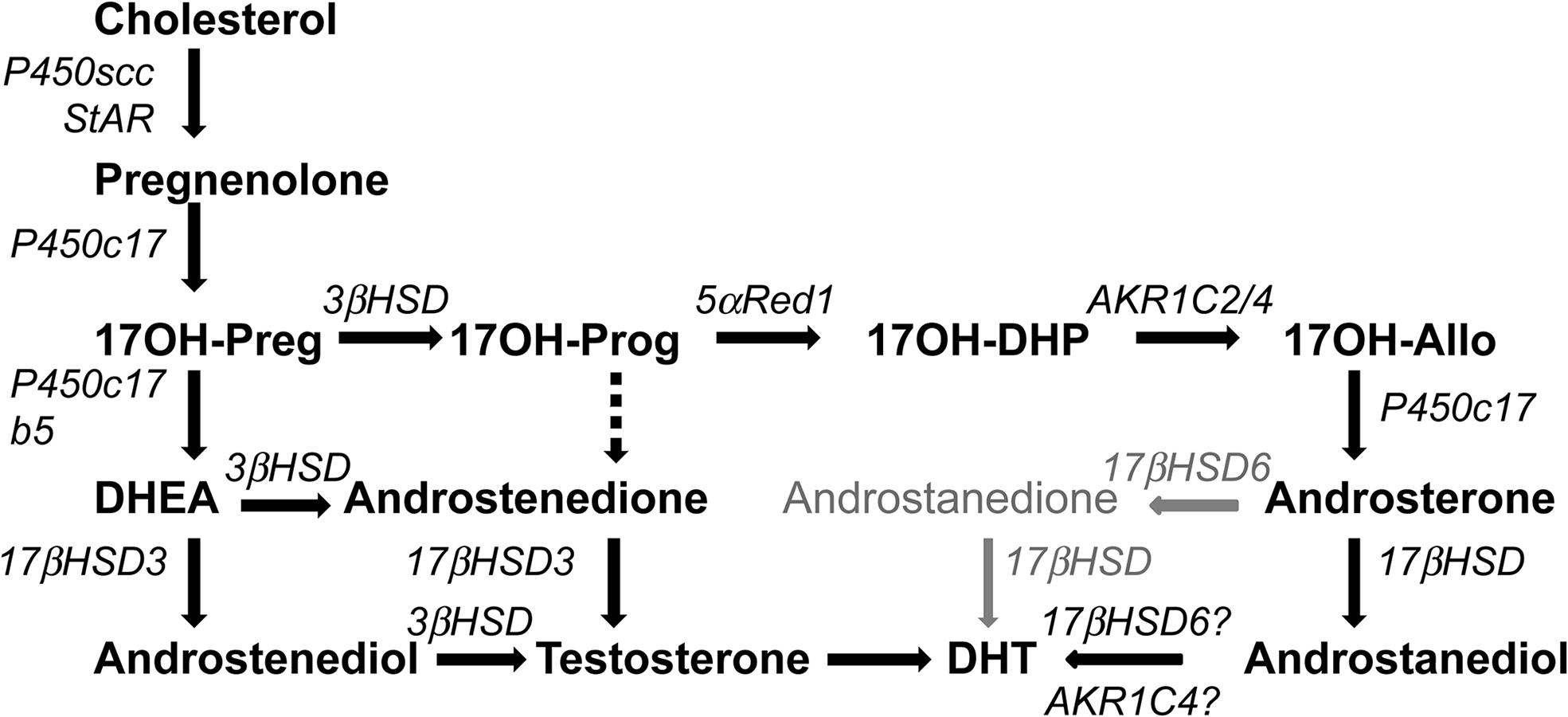
The backdoor pathway is characterized by both reductive and oxidative 3αHSD activities; the reductive activity can apparently be catalyzed by either AKR1C2 or AKR1C4. The oxidative 3αHSDs are SDRs that are similar to the retinol dehydrogenase or cis-retinol/androgen dehydrogenase (RoDH/CRAD) subfamily. The most active member of these is RoDH, also called 17βHSD6, which probably catalyzes the final step in the backdoor pathway. In the brain, 3αHSDs reduce 5α-dihydroprogesterone to allopregnanolone, which is an allosteric activator of the gamma-aminobutyric acid (GABA) A receptors. Further studies of the role of the backdoor pathway will be central to pediatric endocrinology.
Embryonic adrenocortical steroidogenesis begins around 7 weeks after fertilization. Steroidogenic enzymes are immunocytochemically identifiable, principally in the fetal zone, at 50 to 52 days postconception, and by 8 weeks postconception, the adrenal contains cortisol and responds to ACTH in primary culture systems. This cortisol synthesis is regulated by pituitary ACTH and involves transient expression of adrenal 3βHSD2: following the ninth week postconception, expression of 3βHSD2 and synthesis of cortisol wane, and 3βHSD2 is barely detectable at 10 to 11 weeks and absent at 14 weeks. At the same time, the fetal adrenal also produces 17βHSD5, which can convert androstenedione to testosterone. Thus the fetal adrenal makes cortisol at the same time during gestation that fetal testicular testosterone is virilizing the genitalia of the normal male fetus. This fetal adrenal cortisol apparently suppresses ACTH, which otherwise would drive adrenal androgen synthesis and virilization of 46,XX fetuses.
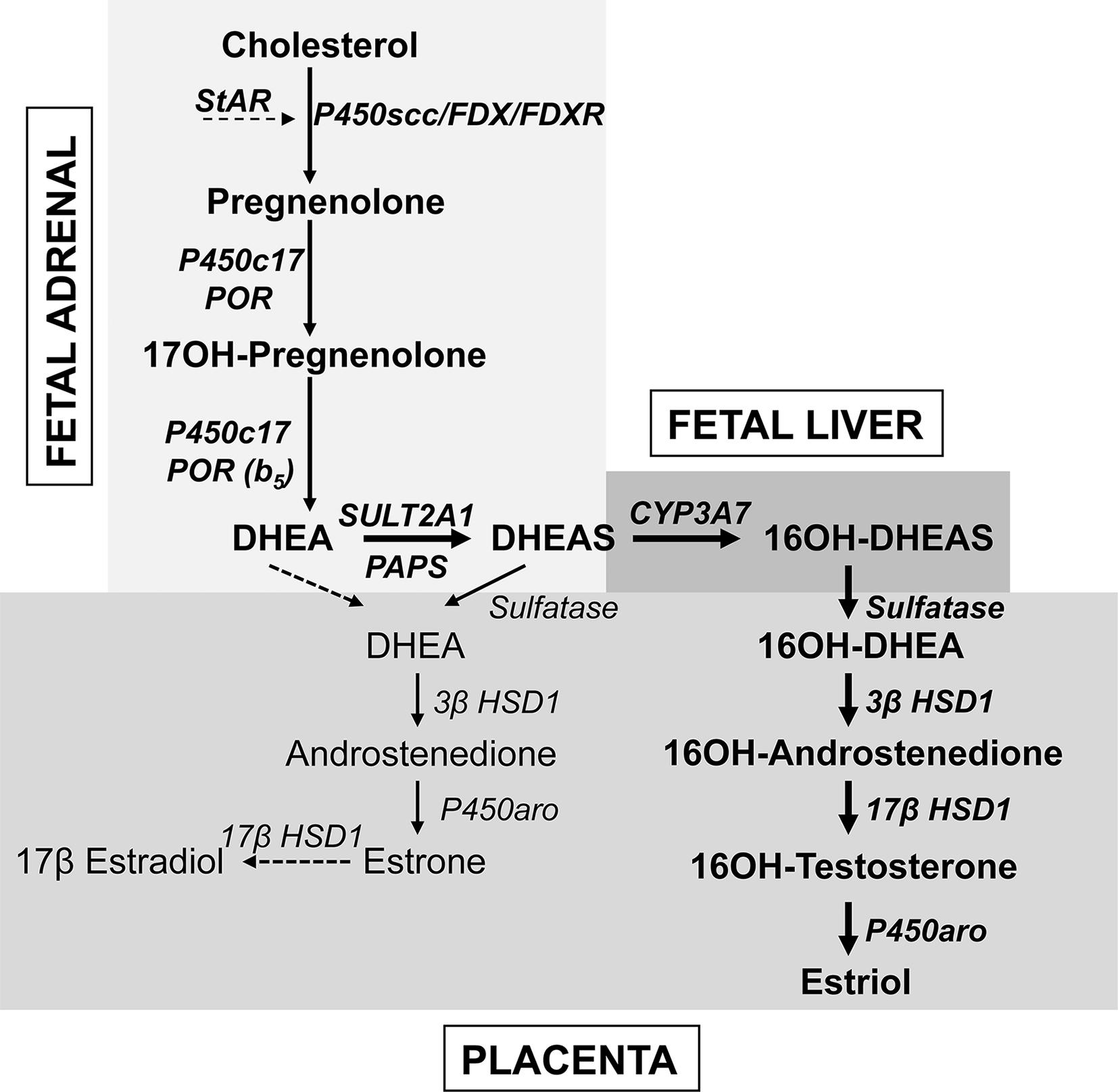
Fetuses affected with genetic lesions in adrenal steroidogenesis can produce sufficient adrenal androgen to virilize a female fetus to a nearly male appearance, and this masculinization of the genitalia is complete by about the 12th week of gestation. The definitive zone of the fetal adrenal produces steroid hormones according to the pathways in Fig. 14.3 . In contrast, the large fetal zone of the adrenal is relatively deficient in 3βHSD2 activity after 12 weeks. Robust 17,20 lyase activity and low 3βHSD activity in the fetal adrenal account for the abundant production of DHEA and its sulfate, DHEAS, which are then converted to estrogens by the placenta ( Fig. 14.7 ). The fetal adrenal also has considerable sulfotransferase activity but little steroid sulfatase activity, also favoring conversion of DHEA to DHEAS. The resulting DHEAS is not a substrate for adrenal 3βHSD2, and is secreted, 16α-hydroxylated in the fetal liver, and then acted on by placental 3βHSD1, 17βHSD1, and P450aro to produce estriol; steroids that escape 16α-hydroxylation in the fetal liver yield estrone and estradiol. Placental estrogens inhibit adrenal 3βHSD activity, providing a feedback system to promote production of DHEAS. Fetal adrenal steroids account for 50% of the estrone and estradiol and 90% of the estriol in the maternal circulation.
Although the feto-placental unit produces huge amounts of DHEA, DHEAS, and estriol (and other steroids), they do not appear to serve an essential role. Successful pregnancy requires placental synthesis of progesterone, which suppresses uterine contractility and prevents spontaneous abortion; however, fetuses with genetic disorders of adrenal and gonadal steroidogenesis develop normally, reach term gestation, and undergo normal parturition and delivery. Mineralocorticoid production is only required postnatally, estrogens are not required, and androgens are only needed for male sexual differentiation. It appears that human fetal glucocorticoids are needed at about 8 to 12 weeks, but it is not clear that they are needed thereafter; if they are, the small amount of maternal cortisol that escapes placental inactivation suffices. A single newborn has been described with profound glucocorticoid resistance who was homozygous for a frameshift mutation at codon 772 in the glucocorticoid-binding domain of the glucocorticoid receptor (GR). Although the infant had severe hypoglycemia and hypertension postnatally, pulmonary and other aspects of fetal development were normal, suggesting that glucocorticoid action is not required for normal human fetal development.
The regulation of steroidogenesis and growth of the fetal adrenal are not fully understood, but both are related to ACTH. ACTH effectively stimulates steroidogenesis by fetal adrenal cells in vitro, and excess ACTH is clearly involved in the adrenal growth and overproduction of androgens in fetuses affected with CAH. Experimental prenatal treatment of such fetuses by administering pharmacologic doses of dexamethasone to the mother at 6 to 10 weeks’ gestation can significantly reduce fetal adrenal androgen production and thus reduce the virilization of female fetuses, indicating that the hypothalamic-pituitary-adrenal (HPA) axis functions very early in fetal life. In contrast, anencephalic fetuses lacking pituitary ACTH have adrenals that contain a fairly normal complement of steroidogenic enzymes and retain their capacity for steroidogenesis. Thus fetal adrenal steroidogenesis may be regulated by both ACTH-dependent and ACTH-independent mechanisms.
The principal steroidal product of the human adrenal is cortisol, which is mainly secreted in response to ACTH (corticotropin) produced in the pituitary; secretion of ACTH is stimulated primarily by corticotropin-releasing factor (CRF) from the hypothalamus. The history of the discovery of the components of the HPA axis and their interrelationships has been reviewed recently. Hypothalamic CRF is a 41-amino acid peptide synthesized mainly by neurons in the paraventricular nucleus. These same hypothalamic neurons also produce the decapeptide arginine vasopressin (AVP, also known as antidiuretic hormone or ADH). Both CRF and AVP are proteolytically derived from larger precursors, with the AVP precursor containing the sequence for neurophysin, which is the AVP-binding protein. CRF and AVP travel through axons to the median eminence, which releases them into the pituitary portal circulation, although most AVP axons terminate in the posterior pituitary. AVP is cosecreted with CRF in response to stress, and both CRF and AVP stimulate the synthesis and release of ACTH, but they appear to do so by different mechanisms. CRF binds to a G protein–coupled receptor on the membranes of pituitary corticotropes and activates adenylyl cyclase, increasing cAMP, which activates the protein kinase A (PKA) signaling pathway. PKA triggers ACTH secretion by concerted regulation of cellular potassium and calcium fluxes, and enhances proopiomelanocortin ( POMC ) gene transcription. AVP binds to its G protein–coupled receptor and activates phospholipase C, which leads to the release of intracellular Ca ++ and to the activation of protein kinase C (PKC). AVP seems to amplify the effects of CRF on ACTH secretion without affecting synthesis. However, CRF is the more important physiologic stimulator of ACTH release, although maximal doses of AVP can elicit a maximal ACTH response. When given together, CRF and AVP act synergistically, as would be expected from their independent mechanisms of action.
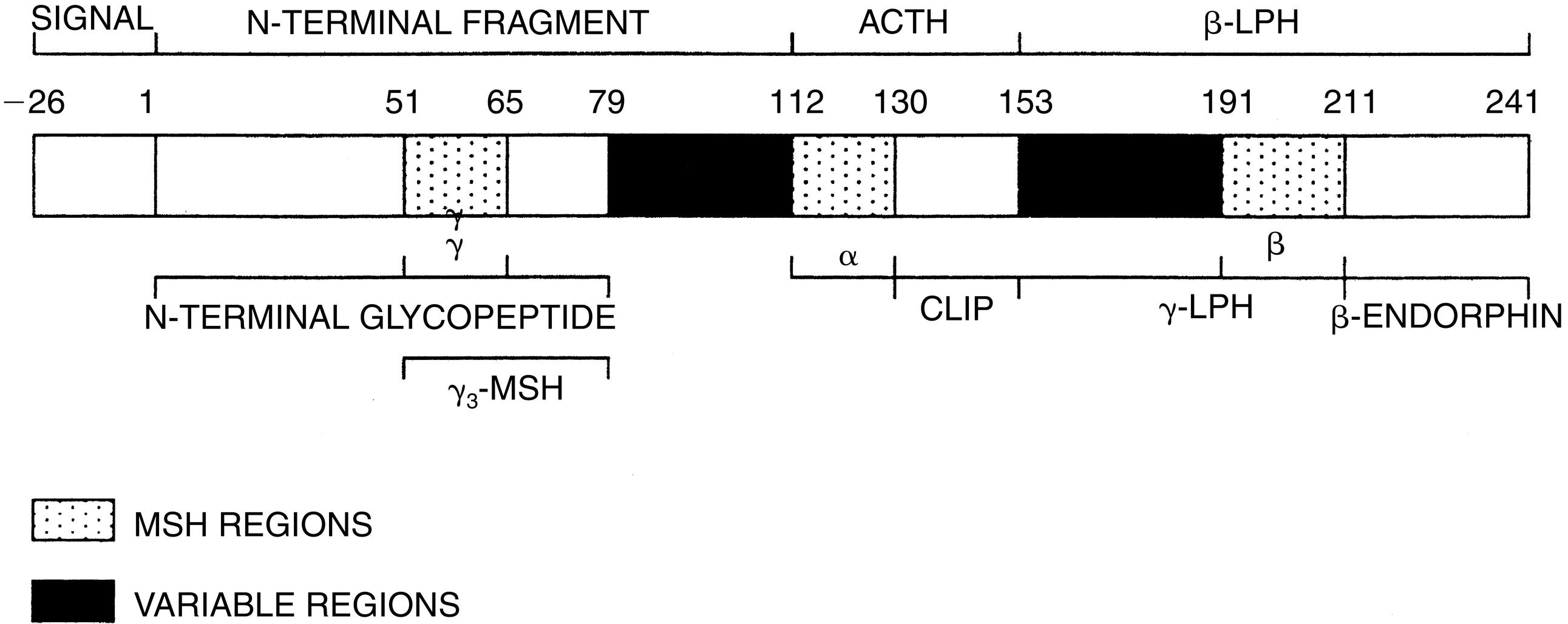
Pituitary ACTH is a 39-amino acid peptide derived from POMC, a 241-amino acid protein. POMC undergoes a series of proteolytic cleavages, yielding several biologically active peptides ( Fig. 14.8 ). The N-terminal glycopeptide (POMC 1-75) can stimulate steroidogenesis and may function as an adrenal mitogen. POMC 112-150 is ACTH 1-39, POMC 112-126 and POMC 191-207 constitute α- and β-MSH (melanocyte stimulating hormone), respectively, and POMC 210-241 is β-endorphin. POMC is also produced in small amounts by the brain, testis, liver, kidney, and placenta, but this extrapituitary POMC does not contribute significantly to circulating ACTH. Malignant tumors will commonly produce “ectopic ACTH” in adults and rarely in children; this ACTH derives from ectopic biosynthesis of the same POMC precursor. Only the first 20 to 24 amino acids of ACTH are needed for its full biologic activity, and synthetic ACTH 1-24 is widely used in diagnostic tests of adrenal function. However, these shorter forms of ACTH have a shorter half-life than does native ACTH 1-39. POMC gene transcription is stimulated by CRF and inhibited by glucocorticoids.
ACTH stimulates the G protein–coupled melanocortin 2 receptor (MCR2), which is located almost exclusively in the adrenal cortex. Activation of MCR2 triggers the production of cAMP, activating PKA that catalyzes the phosphorylation of many proteins involved in steroidogenesis, thereby modifying their activity. ACTH elicits both acute and long-term effects. ACTH stimulates the biosynthesis of LDL receptors and the uptake of LDL, which provides most of the cholesterol used for steroidogenesis, and stimulates transcription of the gene for HMG-CoA reductase, the rate-limiting step in cholesterol biosynthesis, but adrenal biosynthesis of cholesterol is quantitatively much less important than the uptake of LDL cholesterol. Cholesterol is stored in steroidogenic tissues as cholesterol esters in lipid droplets. ACTH stimulates the activity of cholesterol esterase, while inhibiting cholesterol ester synthetase, thus increasing the intracellular pool of free cholesterol, the substrate for P450scc. Finally, ACTH facilitates transport of cholesterol into mitochondria, by stimulating the synthesis and phosphorylation of StAR, thus increasing the flow of free cholesterol into the mitochondria. All of these actions are mediated by cAMP and occur within minutes, constituting the “acute” effect of ACTH on steroidogenesis. The adrenal contains relatively modest amounts of steroid hormones; thus release of preformed cortisol does not contribute significantly to the acute response to ACTH; acute responses occur by the rapid provision of large supplies of cholesterol to mitochondrial P450scc.
The long-term “chronic” effects of ACTH are mediated directly at the level of the steroidogenic enzymes. ACTH via cAMP stimulates the accumulation of the steroidogenic enzymes and their mRNAs by stimulating the transcription of their genes. ACTH also increases adrenal blood flow, increasing the influx of oxygen and metabolic fuel and the delivery of newly secreted hormones to the circulation. Thus ACTH increases both the uptake of the cholesterol substrate and its conversion to steroidal products. The stimulation of this steroidogenesis occurs at each step in the pathway, and not only at the rate-limiting step, P450scc.
The role of ACTH and other peptides derived from POMC, in stimulating growth of the adult adrenal, is supported by the observations that lack of pituitary POMC causes severe adrenal hypoplasia, and chronic ACTH excess causes adrenal hyperplasia. In the fetal adrenal, ACTH stimulates the local production of IGF-2, FGF2, and EGF. These, and possibly other factors work together to mediate ACTH-induced growth of the fetal adrenal.
Plasma concentrations of ACTH and cortisol tend to be high in the morning and low in the evening. Peak ACTH levels are usually seen at 4 to 6 AM and peak cortisol levels follow at about 8 AM. Both ACTH and cortisol are released episodically in pulses every 30 to 120 minutes throughout the day, but the frequency and amplitude of these is much greater in the morning. The basis of this diurnal rhythm is complex and poorly understood. The hypothalamic content of CRF itself shows a diurnal rhythm with peak content at about 4 AM. At least four factors appear to play a role in the rhythm of ACTH and cortisol: intrinsic rhythmicity of synthesis and secretion of CRF by the hypothalamus; light/dark cycles; feeding cycles; and inherent rhythmicity in the adrenal, possibly mediated by adrenal innervation. These factors are clearly interdependent and related. Dietary rhythms may play as large a role as light/dark cycles. Animal experiments show that altering the time of feeding can overcome the ACTH/cortisol periodicity established by a light/dark cycle. In normal human subjects, cortisol is released before lunch and supper, but not at these times in persons eating continuously during the day. Thus glucocorticoids, which increase blood sugar, appear to be released at times of fasting and are inhibited by feeding.
As all parents know, infants do not have a diurnal rhythm of sleep or feeding. Infants acquire such behavioral rhythms in response to their environment long before they acquire a rhythm of ACTH and cortisol. The diurnal rhythms of ACTH and cortisol begin to be established at 6 to 12 months and often are not well established until after 3 years of age. Once the rhythm is well established in the older child or adult, it is changed only with difficulty. When people move to different parts of the world, their ACTH/cortisol rhythms generally take 15 to 20 days to adjust appropriately. Reentrainment of the circadian clock following jet lag requires approximately 1 to 2 hours/day, more for eastward and less for westward travel.
Physical stress (such as major surgery, severe trauma, blood loss, high fever, or serious illness) can increase the secretion of both ACTH and cortisol, but minor surgery and minor illnesses (such as upper respiratory infections) have little effect on ACTH and cortisol secretion. Infection, fever, and pyrogens can stimulate the release of cytokines, such as interleukin (IL)-1 and IL-6, which stimulate secretion of corticotropin-releasing hormone (CRH), and also stimulate IL-2 and tumor necrosis factor (TNF), which stimulate release of ACTH, providing further stimulus to cortisol secretion during inflammation ; furthermore, IL-6 can directly stimulate adrenal synthesis and release of cortisol. Conversely, glucocorticoids inhibit cytokine production in the immune system, providing a negative feedback loop. Most psychoactive drugs, such as anticonvulsants, neurotransmitters, and antidepressants, do not affect the diurnal rhythm of ACTH and cortisol, although cyproheptadine (a serotonin antagonist) can suppress ACTH release.
The HPA axis is a classic example of an endocrine feedback system. ACTH increases production of cortisol, and cortisol decreases production of ACTH. Cortisol and other glucocorticoids exert feedback inhibition of both CRF and ACTH (and AVP), principally through the GR. Like the acute and chronic phases of the action of ACTH on the adrenal, there are acute and chronic phases of the feedback inhibition of ACTH (and presumably CRF). The acute phase, which occurs within minutes, inhibits release of ACTH (and CRF) from secretory granules. With prolonged exposure, glucocorticoids inhibit ACTH synthesis by directly inhibiting the transcription of the gene for POMC (and AVP), which can result in secondary adrenal insufficiency. Some evidence also suggests that glucocorticoids can directly inhibit steroidogenesis at the level of the adrenal fasciculata cell itself, but this appears to be a physiologically minor component of the regulation of cortisol secretion.
Renin is a serine protease enzyme synthesized primarily by the juxtaglomerular cells of the kidney, but it is also produced in a variety of other tissues, including the glomerulosa cells of the adrenal cortex. The role of adrenally produced renin is not well established; it appears to maintain basal levels of P450c11AS, but it is not known if angiotensin II is involved in this action. Renin is synthesized as a precursor of 406 amino acids that is cleaved to prorenin (386 amino acids) and finally to the 340-amino acid protein found in plasma. Decreased blood pressure, upright posture, sodium depletion, vasodilatory drugs, kallikrein, opiates, and β-adrenergic stimulation all promote release of renin. Renin enzymatically attacks angiotensinogen, the renin substrate, in the circulation. Angiotensinogen is a highly glycosylated protein, and therefore has a highly variable molecular weight from 50,000 to 100,000 daltons. Renin proteolytically releases the amino-terminal 10 amino acids of angiotensinogen, referred to as angiotensin I . This decapeptide is biologically inactive until converting enzyme, an enzyme found primarily in the lungs and blood vessels, cleaves off its two carboxy-terminal amino acids, to produce an octapeptide, termed angiotensin II . Angiotensin II binds to specific membrane receptors located in the zona glomerulosa of the adrenal cortex to stimulate aldosterone production. Angiotensin-converting enzyme can be inhibited by captopril and related agents; alternatively angiotensin II receptors may be blocked by pharmacologic agents, such as candesartan for the diagnosis and treatment of (hyperreninemic) hypertension.
Angiotensin II has two principal actions, both of which increase blood pressure. It directly stimulates arteriolar vasoconstriction within a few seconds and it stimulates synthesis and secretion of aldosterone within minutes. Increased plasma potassium is a highly potent, direct stimulator of aldosterone synthesis and release. Aldosterone, secreted by the glomerulosa cells of the adrenal cortex, has the greatest mineralocorticoid activity of all naturally occurring steroids. Aldosterone causes renal potassium excretion and sodium retention, with a consequent increase in intravascular volume and blood pressure. Expansion of the blood volume provides the negative feedback signal for regulation of renin and aldosterone secretion. Angiotensin II binds to AT 1 , its G protein–coupled receptor (G q ) to stimulate production of phosphatidylinositol, mobilize intracellular and extracellular Ca ++ , and activate signaling via PKC and the calcium-calmodulin system. These intracellular second messengers stimulate transcription of the CYP11A1 gene for P450scc independently of the actions of ACTH and cAMP. Increases in plasma potassium directly regulate aldosterone production by depolarizing zona glomerulosa cells, which leads to an influx of Ca ++ through voltage-dependent calcium channels. Thus angiotensin II and increased concentrations of potassium converge on the same intracellular second messenger pathway to regulate aldosterone synthesis and secretion. Although the renin-angiotensin system is clearly the major regulator of mineralocorticoid secretion, ACTH (and possibly other POMC-derived peptides) can also promote secretion of aldosterone. Ammonium ion, hyponatremia, dopamine antagonists, and some other agents can also stimulate secretion of aldosterone, and atrial natriuretic factor is a potent physiologic inhibitor of aldosterone secretion.
The trophic roles of angiotensin II and hyperkalemia are supported by animal studies showing a dynamic expansion of the zona glomerulosa in response to chronic volume depletion, MR blockade, a low-sodium diet, and/or a high-potassium diet. In contrast, chronic volume expansion, as occurs with a high-sodium diet and/or hypokalemia, inhibits growth of the zona glomerulosa.
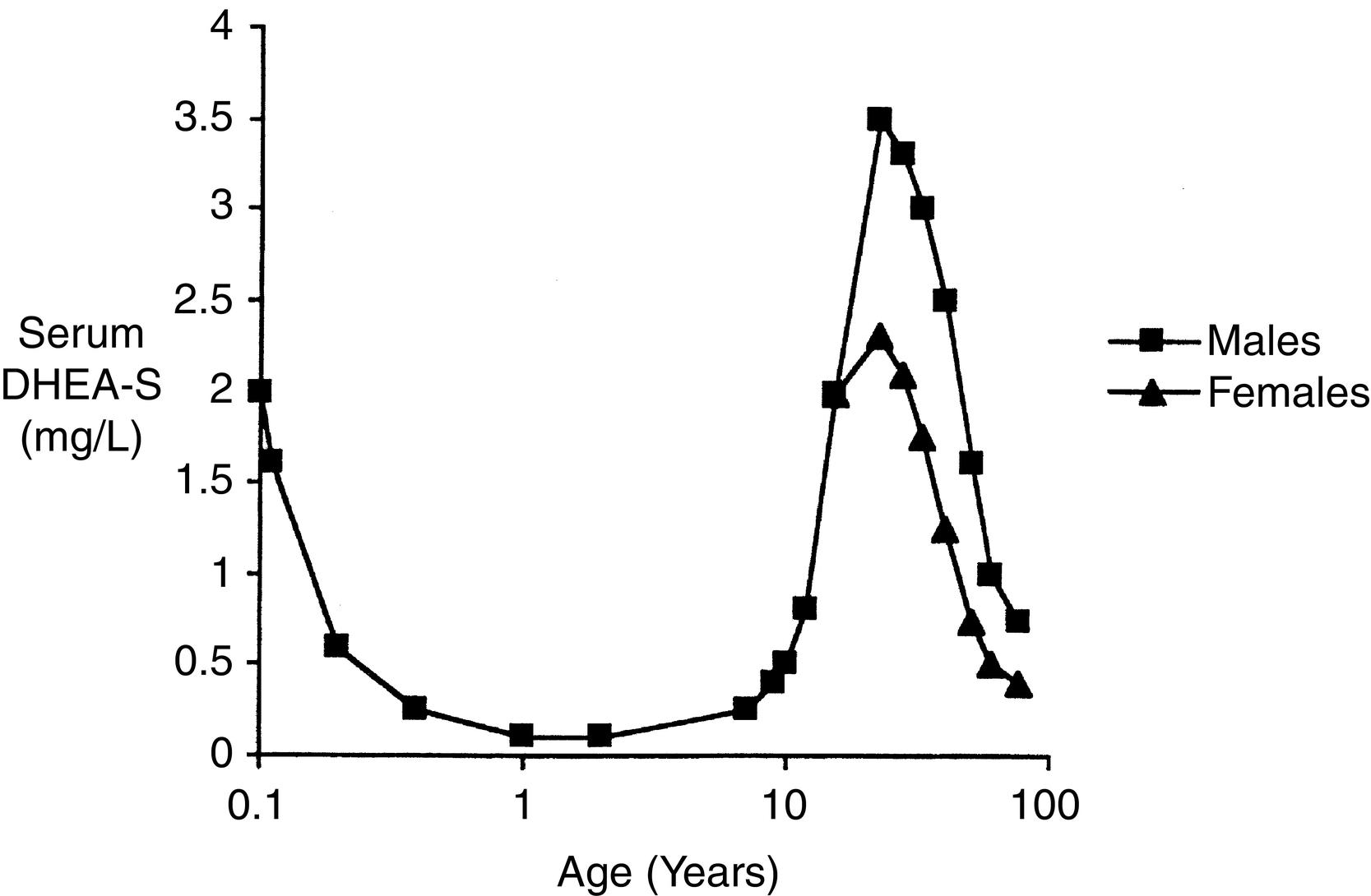
DHEA, DHEAS, and androstenedione, which are almost exclusively secreted by the adrenal zona reticularis, are generally referred to as adrenal androgens because they can be peripherally converted to testosterone. However, these steroids have little if any capacity to bind to and activate androgen receptors, hence they are only androgen precursors, and not true androgens. The fetal adrenal secretes large amounts of DHEA and DHEAS, and these steroids are abundant in the newborn, but their concentrations fall rapidly as the fetal zone of the adrenal involutes following birth. After the first year of life, the adrenals of young children secrete very small amounts of DHEA, DHEAS, and androstenedione until the onset of adrenarche, usually around age 7 to 8 years, preceding the onset of puberty by about 2 years. Adrenarche is independent of puberty, the gonads, or gonadotropins, and the mechanism by which the onset of adrenarche is triggered remains unknown. The secretion of DHEA and DHEAS continues to increase during and after puberty and reach maximal values in young adulthood, following which there is a slow, gradual decrease in the secretion of these steroids in the elderly (“adrenopause”) ( Fig. 14.9 ). Men have higher serum concentrations of DHEAS than women, probably because men have a single copy of the X-linked steroid sulfatase gene. Throughout much of adult life, adrenal secretion of DHEAS exceeds that of cortisol; in adult women, adrenal secretion of androgen precursors and androgens is equal to their secretion from the ovary. Despite the huge increases in the adrenal secretion of DHEA and DHEAS during adrenarche, circulating concentrations of ACTH and cortisol do not change with age. Thus ACTH plays a permissive role in adrenarche but does not trigger it. Searches for hypothetical polypeptide hormones that might specifically stimulate the zona reticularis have been unsuccessful. Adrenarche is a unique phenomenon confined to few higher primates, such as chimpanzees or orangutans, but the significance of adrenarche remains unknown.
Recent studies of adrenarche have focused on the roles of 3βHSD and P450c17. The abundance of 3βHSD in the zona reticularis appears to decrease with the onset of adrenarche, and the adrenal expression of cytochrome b 5 , which fosters the 17,20 lyase activity of P450c17, is almost exclusively confined to the zona reticularis; these factors strongly favor the production of DHEA. The phosphorylation of P450c17, apparently by p38α, also increases 17,20 lyase activity, but its potential role in adrenarche remains unexplored. Premature and exaggerated adrenarche may be associated with insulin resistance and/or being overweight, and girls with premature exaggerated adrenarche appear to be at much higher risk of developing the polycystic ovary syndrome as adults (characterized by hyperandrogenism, fewer ovulatory cycles, insulin resistance, and hypertriglyceridemia). Recent evidence suggests that infants born small for gestational age may be at increased risk for this syndrome. Thus studies of physiology, biochemistry, and clinical correlates of adrenarche suggest premature adrenarche may be an early sign of a metabolic disorder. The suggestion that replacing the DHEA may improve memory and a sense of well-being in the elderly and in adrenal insufficiency remains controversial.
Whereas it has long been thought that DHEA, DHEAS, and androstenedione are “adrenal androgens,” recent work has shown that the principal adrenal androgens are 11-oxygenated (Oxo) steroids, mainly 11-keto-testosterone (11-KT). In addition to being expressed in the zona fasciculata, P450c11β, the classic 11-hydroxylase that converts 11-deoxycortisol to cortisol, is expressed in the zona reticularis, where it converts androstenedione and testosterone to 11OH-androstenedione and 11OH-testosterone, respectively. These 11-Oxo steroids can be converted into the nonaromatizable 11-keto androstenedione and 11-KT by HSD11B2 ( Fig. 14.10 ). 11-KT may also be 5α-reduced to 11-keto dihydrotestosterone (11-KDHT); 11-KT and 11-KDHT are androgens that bind and activate the androgen receptor with affinities similar to those of testosterone and DHT; these androgens are found at similar levels in men and woman, are higher in the adrenal vein than in peripheral veins, and are elevated in CAH and polycystic ovary syndrome. Thus 11-KT appears to be the dominant circulating bioactive androgen during both normal and premature adrenarche, as well as in classic CAH. These 11-Oxo steroids correlate with adrenal size and may be useful biomarkers for adrenal rest tumors in CAH patients.
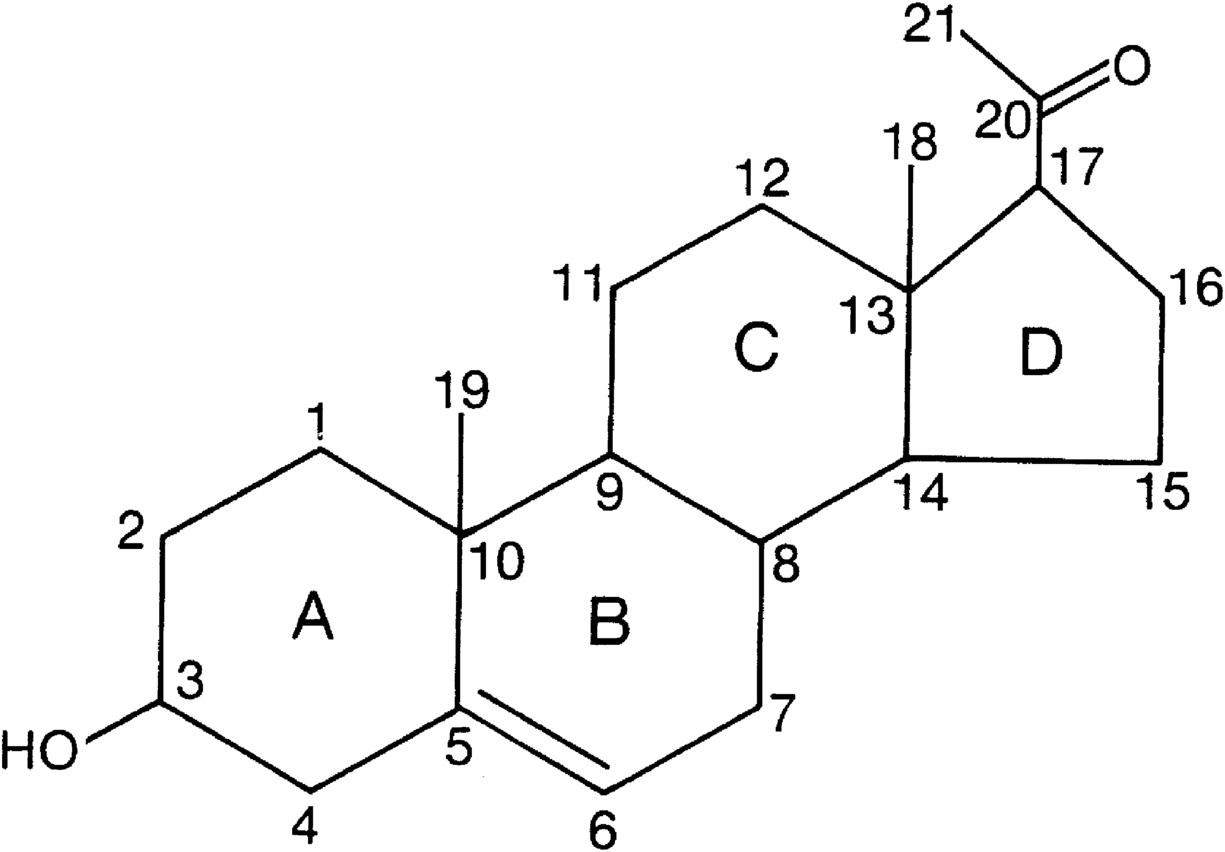
All steroid hormones are derivatives of pregnenolone ( Fig. 14.11 ). Pregnenolone and its derivatives that contain 21 carbon atoms are often termed C21 steroids. Each carbon atom is numbered, indicating the location at which the various steroidogenic reactions occur (e.g., 21-hydroxylation, 11-hydroxylation). The 17,20 lyase activity of P450c17 cleaves the bond between carbon atoms 17 and 20, yielding C19 steroids, which include all the androgens; P450aro converts C19 androgens to C18 estrogens. With the exception of estrogens, all steroid hormones have a single unsaturated carbon-carbon double bond. Steroids having this double bond between carbon atoms 4 and 5, including all the principal biologically active steroids, are termed Δ 4 steroids; their precursors having a double bond between carbon atoms 5 and 6 are termed Δ 5 steroids. The two isozymes of 3βHSD convert Δ 5 to Δ 4 steroids.
There is a logically systematic, unambiguous chemical terminology to describe accurately the structure of all the steroid hormones and all their conceivable derivatives. However, this terminology is unbelievably cumbersome (e.g., cortisol is 11β,17α,21-trihydroxy-pregn-4-ene-3,20-dione, and dexamethasone is 9α-fluoro-11β,17α,21-trihydroxypregna-1,4-diene-3,20-dione). Therefore we use only the standard “trivial names.” Before the structures of the steroid hormones were determined in the 1930s, Reichstein, Kendall, and others identified them as spots on paper chromatograms and designated them A, B, C, and so on. Unfortunately, some persist in using this outmoded terminology more than 80 years later, so that corticosterone is sometimes termed compound B, cortisol compound F, and 11-deoxycortisol compound S. This archaic terminology obfuscates the precursor-product relationships of the steroids, confuses students, and should not be used.
Although over 50 different steroids have been isolated from adrenocortical tissue, the main pathways of adrenal steroidogenesis include only a dozen or so steroids, of which only a few are secreted in sizable quantities. The adult secretory rates for DHEA and cortisol are each about 20 mg/24 hours and the secretion of corticosterone, a weak glucocorticoid, is about 2 mg/24 hours. Although glucocorticoids, such as cortisol, and mineralocorticoids, such as aldosterone, are both needed for life and hence are of physiologic importance, diagrams, such as Fig. 14.3 , fail to indicate that these steroids are not secreted in molar equivalents. The adult secretion rate of aldosterone is only about 0.1 mg/24 hours. This 100- to 1000-fold molar difference in the secretory rates of cortisol and aldosterone must be borne in mind when considering the effects of steroid-binding proteins in plasma and when conceptualizing the physiologic manifestations of incomplete defects in steroidogenesis.
Most circulating steroids are bound to plasma proteins, including corticosteroid-binding globulin (CBG), albumin, and α 1 acid glycoprotein. CBG has a very high affinity for cortisol but a relatively low binding capacity albumin has a low affinity and high capacity and α 1 acid glycoprotein is intermediate for both variables. The result is that about 90% of circulating cortisol is bound to CBG and a little more is bound to other proteins. Interestingly, absence of CBG does not cause a detectable physiologic disorder. Therefore these plasma proteins are thought to act as a nonessential reservoir for steroids that facilitates broad and even distribution of cortisol throughout the body. Most synthetic glucocorticoids used in therapy do not bind significantly to CBG and bind poorly to albumin, partially accounting for their increased potencies, which are also associated with increased receptor-binding affinities. Aldosterone is not bound well by any plasma protein; hence changes in plasma protein concentration do not affect plasma aldosterone concentrations, but greatly influence plasma cortisol concentrations. Estradiol and testosterone bind strongly to a different plasma protein termed sex steroid-binding globulin and also bind weakly to albumin.
Because steroids are hormones, it is often thought that the concentration of “free” (i.e., unbound) circulating steroids determines biologic activity. However, the target tissues for many steroid hormones contain enzymes that modify those steroids. Thus many actions of testosterone are actually caused by DHT produced by local 5α-reductase. Similarly, cortisol will have differential actions on various tissues because of the presence or absence of the two isozymes of 11βHSD, which can inactivate cortisol to cortisone or reactivate cortisone back to cortisol. Analogous peripheral metabolism occurs via “extraglandular” 21-hydroxylase, P450aro, 3βHSD, and 17βHSD. Thus circulating steroids are both classic hormones and precursors to locally acting autocrine or paracrine factors.
Only about 1% of circulating plasma cortisol and aldosterone are excreted unchanged in the urine; the remainder is metabolized by the liver. Technologies, such as labeled tracers and mass spectroscopy, have enhanced our understanding of adrenal physiology and have advanced clinical care. Understanding the processes and pathways of steroid metabolism can facilitate more rapid and precise diagnoses and avoid unwanted side effects from drugs. Liquid chromatography-mass spectrometry (LC-MS/MS) can now specifically and simultaneously identify and quantify major and minor metabolites. The major enzymes that metabolize steroids are summarized later.
The liver is the primary site of glucocorticoid metabolism. Cortisol is reduced, oxidized, or hydroxylated and then conjugated with sulfate or glucuronic acid, rendering it water soluble, and is excreted in the urine. 3α-Hydroxysteroid dehydrogenase (e.g., AKR1C2 and AKR1C4) is the major enzyme group that reduces cortisol at the 3-keto group, and 5α- or 5β-reductases (SRD5A1 and AKR1D1, respectively) reduce the 4-5 double bond in the A ring. The tetrahydrocortisols and tetrahydrocortisones that result from these reactions can be reduced by 20-hydroxysteroid dehydrogenases, producing cortols and cortolones. Depending on cofactor availability, 11β-hydroxysteroid dehydrogenase type 1 (HSD11B1) can have either dehydrogenase (inactivation) or reductase (activation) activities, but in the liver, this enzyme usually functions as a reductase to activate cortisone to cortisol. Cortisol, and the metabolites generated in the reactions described earlier, are oxidized. This process removes the C20-C21 side chain, resulting in C19 steroids with a 17-ketone group, but the enzyme that drives this reaction has not yet been identified. CYP3A4 can 6β-hydroxylate cortisol; when cortisol levels are normal, the rate of this reaction is very low. However, when cortisol levels are elevated, the rate of the reaction increases, which can make the measurement of urinary 6β-hydroxycortisol a useful adjunct test for excess glucocorticoids. Finally, uridine diphosphoglucuronosyl transferases can conjugate glucuronic acid or sulfate to C19 and C21 metabolites, increasing their water solubility and facilitating their urinary excretion.
Similarly to cortisol, aldosterone is reduced and conjugated in the liver. 4,3-Ketosteroid-reductase (which also has 5β-hydroxysteroid reductase activity) and a 3α-hydroxysteroid dehydrogenase are the major enzymes that result in the conversion of aldosterone to 3α, 5β-tetrahydroaldosterone. Tetrahydroaldosterones are conjugated to glucuronic acid at the 3-keto position (which increases water solubility) and is the major metabolite of aldosterone that is excreted in the urine.
DHEA is the adrenal steroid produced in greatest quantity. DHEA is converted to androstenedione and 5α-reduced to androsterone, which is then converted to etiocholanolone by 5β-reductase. Finally, 17β-hydroxysteroid dehydrogenases reduce etiocholanolones into -diol derivatives, which can be conjugated and excreted in the urine. However, fecal excretion of DHEA and its metabolites is higher than other steroids. The sulfate ester of DHEA (DHEAS), on the other hand, can be directly excreted in the urine. Although these pathways can seem somewhat esoteric, as illustrated later, these pathways can be perturbed by common therapies and conditions, hence they need to be considered in clinical diagnostic and treatment plans.
Thyroid Hormone accelerates cortisol metabolism by inducing hepatic 5α- and 5β-reductase activity and inhibiting CYP3A enzymes. The converse process occurs in patients with hypothyroidism. In both situations, serum cortisol levels are usually normal because the HPA axis remains intact. However, in cases of hypopituitarism, it is prudent to replace cortisol before initiating thyroid hormone replacement, to avoid an acute adrenal crisis because of accelerated cortisol clearance.
Spironolactone increases serum aldosterone levels, in part by inhibition of 18-glucuronidation of aldosterone.
Troglitazone induces CYP3A4 activity, disrupting cortisol metabolism. Although neither rosiglitazone nor pioglitazone appear to affect CYP3A4, thiazolidinedione drugs generally inhibit steroidogenic P450c17 and HSD3B2.
Drugs That Alter P450 Enzymes . The results of a randomized control trial supported reports that consuming Hypericum perforatum (St. John’s Wort, a common herbal remedy) decreased efficacy of estradiol-based oral contraception. St. John’s Wort induces CYP3A4, CYP2C19, and CYP2C9, accelerating the metabolism of the oral contraceptives, decreasing their effectiveness. In contrast, the antifungal drug ketoconazole acts principally by inhibiting CYP51 (lanosterol demethylase), but it also inhibits several steroidogenic P450 enzymes and has been used as adjunctive therapy in prostate cancer and Cushing syndrome.
Stress: Surprisingly, elevations in ACTH levels are usually a transient processes, even when stress is prolonged. The persistently elevated cortisol levels during chronic stress are caused by stimulating cytokines and diminished clearance of cortisol through enzymatic inactivation by 5α- and 5β-reductases and by HSD11B2.
Cushing Syndrome: It is thought that when glucocorticoid levels remain persistently elevated, the oxidation and reduction pathways that metabolize them become saturated and CYP3A4 is induced. This results in increased levels of 6β-hydroxylation (and concomitantly lower levels of cortols, cortolones, tetrahydrocortisone, and 5α- tetrahydrocortisol) excreted, which can be confirmed by analysis of the urine. Elevations in the levels of glucocorticoids also stimulate hepatic HSD11B2 activity.
Obesity: Obese individuals have elevated levels of cortisol metabolites in their urine, even when normalized for body surface area. It is important to distinguish this process from Cushing syndrome. In obese patients, serum cortisol levels are normal as the higher excretion rate is matched by higher production rates.
Insulin Resistance: Individuals with insulin resistance, including those with hyperinsulinemia, have increased levels of hepatic SRD5A1 activity, increasing urinary excretion of 5α-reduced metabolites of cortisol.
Renal Disease: Although metabolism of cortisol is usually normal in patients with renal disease, clearance of glucuronides can be reduced, causing accumulation of the inactive conjugated compounds in the circulation. This process could potentially be used to monitor disease but is not thought to contribute to pathology.
Heart Failure: Patients with severe congestive heart failure and impaired perfusion of the liver also have impaired aldosterone metabolism, resulting in lower levels of urinary tetrahydroaldosterone glucuronide.
Astute clinical evaluation can generally reveal the presence of primary adrenal deficiency or hypersecretion before performing laboratory tests. Thomas Addison described adrenal insufficiency in 1849, long before immunoassays became available. Virtually all patients with chronic adrenal insufficiency will have weakness, fatigue, anorexia, weight loss, hypotension, and hyperpigmentation. Patients with acute adrenal insufficiency may have hypotension, shock, weakness, apathy, confusion, anorexia, nausea, vomiting, dehydration, abdominal or flank pain, hyperthermia, and/or hypoglycemia. Deficient adrenal androgen secretion will compromise the acquisition of virilizing secondary sexual characteristics (pubic and axillary hair, acne, axillary odor) in female adolescents. Early signs of glucocorticoid excess include increased appetite, weight gain, mood changes, and growth arrest without a concomitant delay in bone age. Chronic glucocorticoid excess in children results in typical Cushingoid facies and muscle wasting, but the “buffalo hump” and centripetal distribution of body fat that are characteristic of adult Cushing disease are seen only in long-standing undiagnosed disease in children. Mineralocorticoid excess is mainly characterized by hypertension, but patients receiving very low sodium diets (e.g., the newborn) will not be hypertensive, as mineralocorticoids increase blood pressure primarily by retaining sodium and thus increasing intravascular volume. Moderate hypersecretion of adrenal androgens is characterized by mild signs of virilization, whereas substantial hypersecretion of adrenal androgens is characterized by accelerated growth, with a disproportionate increase in bone age, increased muscle mass, acne, hirsutism, and deepening of the voice. A key feature of any physical examination of a virilized male is careful examination and measurement of the testes. Bilaterally enlarged testes suggest true (central) precocious puberty; unilateral testicular enlargement suggests testicular tumor; prepubertal testes in a virilized male indicate an extratesticular source of androgen, such as the adrenal.
Imaging studies are of limited utility in adrenocortical disease. Computed tomography (CT) will only rarely detect pituitary tumors hypersecreting ACTH, and magnetic resonance imaging (MRI) will detect less than half of these, even with gadolinium enhancement. The small size, odd shape, and location near other structures also compromise the use of imaging techniques for the adrenals. CT is currently the first choice of imaging the adrenal gland; while entailing radiation exposure, it has the advantage of higher resolution compared with MRI. Patients with Cushing disease or CAH will have modestly enlarged adrenals, but such enlargement is not detectable by imaging techniques with any useful degree of certainty. Imaging studies may be of assistance in diagnosing gross enlargement of the adrenals in congenital lipoid adrenal hyperplasia, their hypoplasia in adrenal hypoplasia congenita, or in the hereditary ACTH unresponsiveness syndromes, and with many malignant tumors; however, many adrenal adenomas are too small (< 2 mm) to be detected. Thus imaging studies may establish the presence of pituitary or adrenal tumors, but they can never establish their absence. Complementary functional tests, with radiopharmaceuticals targeted to the adrenal cortex and medulla, may enhance the diagnostic utility of imaging studies and are used in combination with scintigraphy, positron emission tomography (PET), and single-photon emission computed tomography (SPECT).
Catheter-directed hormonal sampling is rarely performed in children. Petrosal sinus sampling may be of use in suspected Cushing disease, when imaging studies fail to reveal the pituitary ACTH-secreting tumor. Adrenal vein sampling may distinguish unilateral from bilateral hypersecretory adrenal adenomas (e.g., hyperaldosteronism, Conn syndrome), but these are usually seen in adults.
The diagnostic evaluation of adrenal function is essentially chemical. The nonspecificity of many of the clinical signs described earlier and the disappointing results with imaging studies remind us that any proper evaluation of HPA function must rely on a series of carefully performed physiologic maneuvers associated with hormonal assays. The development of highly specific, exquisitely sensitive assays that can be done on small volumes of blood now permit the direct examination of virtually every hormone involved in adrenal metabolism. In addition, steroid profiling and analysis of serum and urine samples, using chromatographic, mass-spectrometric methods, with which conventional and novel steroid metabolites may be detected simultaneously from a single sample, has developed into a powerful tool to identify characteristic steroidal signatures of complex disorders.
Steroids are typically measured by immunoassays (IAs) or mass spectrometry (MS) methods. IAs are the traditional technique used in most routine laboratories: they are easy, fast, cheap, and widely available. IAs are limited by their specificity, which is limited by (1) a size mismatch between small steroid molecules and the binding fragment of the immunoglobulin, (2) cross-reactivity of antisera to related steroids, and (3) the quality of the antisera themselves. Furthermore, matrix effects caused by cross-reacting nonsteroidal molecules, other lipophilic compounds, or binding proteins in unprocessed samples may also affect specificity of IAs. This effect may be ameliorated by sample purification by liquid or solid phase extraction, chromatography, or precipitation. However, direct IAs on automated high-throughput instruments have pushed IAs to their limits. Although the reliability of IAs has been questioned recently, especially for measuring sex steroids, validated IAs performed properly remain a valuable tool for clinical steroid measurements.
MS may be the most versatile and precise method for the qualitative and quantitative measurement of steroids. Chromatographic methods (gas or liquid) serve as separation techniques, and the mass spectrometer serves as the detector; together, these methods achieve the highest analytical specificity and selectivity. In contrast to IAs, where one test measures a single steroid, a single run in an MS-based assay provides a steroid profile of multiple steroids. Depending on the specific methods applied, instruments may be run in a nondiscriminatory, untargeted scanning mode, which is typically used for research studies. In contrast, in clinical applications, the instruments record preselected ions corresponding to specific steroid analytes. Quantitative analysis of steroids requires internal standards labeled with stable isotopes; these are now commercially available for most steroids of interest, including the newly identified steroid metabolites derived from the “backdoor” and 11-Oxo pathways. In general, gas chromatography followed by mass spectrometry (GC-MS) is the ideal method for separating steroids and is widely used in research laboratories for characterizing steroid metabolites in new or complex disorders of steroidogenesis. However, GC-MS/MS requires sample derivatization, it is complex and time-consuming, and is not suitable for high-throughput analysis of clinical samples. In contrast, LC-MS/MS is easier, faster, and can analyze sulfated and glucuronidated steroids. Thus LC-MS/MS is used as a high-throughput method for steroid analysis and has now become the method of choice. However, all MS-based methods require knowledge of complex analytics and biochemistry and hence are only established in specialized laboratories. Interpreting a steroid profile of a serum or urine sample is not trivial. Concentrations or excretion rates of multiple metabolites are compared with reference values and/or precursor:product ratios calculated as surrogates of enzyme activities. Diagnosis of complex steroid disorders requires pattern recognition from quantitative datasets of multiple steroids. This may be facilitated by unbiased mathematical approaches (“machine learning”) and has been used for some steroid disorders.
Plasma cortisol may be measured by IAs, such as radioimmunoassay (RIA), immunoradiometric assay (IRMA), and electrochemiluminescence assay (ECLIA), the latter being the preferred method in automated high-throughput laboratories. Alternatively, cortisol can also be determined by LC-MS/MS in a standardized setting. It is essential to know what method one's laboratory is using and precisely what this method is measuring. All immunoassays have some degree of cross-reactivity with other steroids. Most cortisol IAs will detect both cortisol and cortisone; in contrast, these are readily distinguished by mass spectrometric techniques. The newborn's plasma contains mainly cortisone rather than cortisol, hence comparison of newborn data obtained by high-performance liquid chromatography (HPLC) or LC-MS/MS to published standards obtained by IAs may incorrectly suggest adrenal insufficiency. Tables 14.2 and 14.3 summarize the normal plasma concentrations for a variety of steroids measured by LC-MS/MS ( https://www.endocrinesciences.com/ ). With the notable exception of DHEAS, most adrenal steroids exhibit a diurnal variation, based on the diurnal rhythm of ACTH. Because the stress of illness or hospitalization can increase adrenal steroid secretion and because diurnal rhythms may not be well established in children under 3 years of age, it is best to obtain two or more samples for the measurement of any steroid.
| Age | Prog | 17OHP | DHEA | DHEA-S | Δ4A | E1 | E2 | T | DHT | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | |||||||||
| Unit | ng/dL | ng/dL | ng/dL | μg/dL | ng/dL | pg/mL | pg/mL | ng/dL | ng/dL | ng/dL | ng/dL | |
| Childhood | ||||||||||||
| Preterms | ||||||||||||
| 26–28 weeks | Postnatal D4 | 124–841 | 82–1484 | 123–882 | 63–935 | 5–16 | 59–125 | 2–13 | 10–53 | |||
| 31–35 weeks | Postnatal D4 | 26–568 | 56–1853 | 122–710 | 50–449 | 5–22 | 37–198 | 2–13 | 10–53 | |||
| Terms | Postnatal D3 | < 78 | 41–1292 | 88–356 | < 10–279 | 20–64 | 75–400 | < 2–15 | 5–60 | |||
| Infants | ||||||||||||
| 1 wk to 6 mo | 13–106 | < 948 | < 112 | < 10–37 | < 15 | < 15 | < 10 | 20–50 | < 3 | |||
| 6–12 mo | 13–106 | < 136 | < 49 | < 10–17 | < 15 | < 15 | < 10 | < 2.5–10 | < 3 | < 3 | ||
| Minipuberty | 2–3 mo | 40–200 (M) | 5–50 | 60–400 | 12–85 | |||||||
| Children | < 91 | < 10–17 | < 15 | < 15 | < 2.5–10 | < 2.5–10 | < 3 | < 3 | ||||
| 1–5 y | < 68 | < 57 | ||||||||||
| 6–7 y | < 111 | < 72 | ||||||||||
| 8–10 y | < 186 | < 193 | ||||||||||
| Males | ||||||||||||
| Pubertal | 1–16 y | < 10–15 | < 491 | |||||||||
| Tanner I | < 91 | < 186 | 13–83 | < 10–17 | < 5–17 | 5–11 | < 2.5–10 | < 3 | ||||
| Tanner II | < 116 | < 202 | 42–109 | < 10–33 | 10–25 | 5–16 | 18–150 | 3–17 | ||||
| Tanner III | 10–138 | < 319 | 48–200 | 17–72 | 15–25 | 5–25 | 100–320 | 8–33 | ||||
| Tanner IV | 29–180 | 39–481 | 102–385 | 15–115 | 15–45 | 10–36 | 200–620 | 22–52 | ||||
| Tanner V | 24–175 | 40–491 | 120–370 | 33–192 | 20–45 | 10–36 | 350–970 | 24–65 | ||||
| Adult | < 10–11 | 27–199 | 10–50 | 8–35 | 264–916 | 30–85 | ||||||
| 20–49 y | 31–701 | 16–523 | 44–186 | |||||||||
| > 50 y | 21–402 | < 298 | ||||||||||
| Females | ||||||||||||
| Pubertal | Tanner I | < 10–26 | < 83 | < 186 | 19–144 | < 10–17 | 4–29 | 5–20 | < 2.5–10 | < 3 | ||
| Tanner II | < 10–255 | 11–98 | < 202 | 34–129 | < 10–72 | 10–33 | 10–24 | 7–28 | 5–12 | |||
| Tanner III | < 10–852 | 11–115 | < 319 | 32–226 | 50–170 | 15–43 | 7–60 | 15–35 | 7–19 | |||
| Tanner IV | < 10–1076 | 18–230 | 39–481 | 58–260 | 47–208 | 16–77 | 21–85 | 13–32 | 4–13 | |||
| Tanner V | < 10–1294 | 20–265 | 40–491 | 44–248 | 50–224 | 29–105 | 34–170 | 20–38 | 3–18 | |||
| Adult | 31–701 | 17–372 | 28–230 | 10–55 | 4–22 | |||||||
| Follicular | < 10–1563 | 15–70 | 30–100 | 30–100 | ||||||||
| Luteal | < 10–2555 | 35–290 | 9–160 | 70–300 | ||||||||
| Peak (D17–23) | 350–3750 | |||||||||||
| Postmenopausal | < 10 | 21–402 | < 215 | < 10–93 | < 40 | < 15 | 7–40 | |||||
| Age | Cortisol | Corticosterone | DOC | 11-Deoxycortisol | 21-Deoxycortisol | 18OH Corticosterone | Aldosterone | Plasma Renin Activity | |
|---|---|---|---|---|---|---|---|---|---|
| Unit | μg/dL | ng/dL | ng/dL | ng/dL | ng/dL | ng/dL | ng/dL | ng/mL/h | |
| Childhood | |||||||||
| Preterms | 11000–167000 | ||||||||
| 26–28 weeks | 1–11 | 235–1108 | 20–105 | 110–1376 | 10–670 | 5–635 | |||
| 31–35 weeks | 2.5–9.1 | 150–1700 | 28–78 | 48–579 | 57–410 | 19–141 | |||
| Term Newborns | < 78 | 2000–35000 | |||||||
| Postnatal D3 | 1.7–14 | 70–850 | 13–147 | 31–546 | 7–184 | ||||
| Postnatal D7 | 2–11 | 70–850 | 5–175 | ||||||
| Infants | 1–12 mo | 2.8–23 | 80–1500 | 7–49 | < 10–156 | 5–220 | 5–90 | 2000–37000 | |
| Children | |||||||||
| 8:00 AM | 1–15 y | 3–21 | 135–1860 | 2–34 | 12–158 | < 10 | |||
| 4:00 PM | 1–15 y | ND | 70–620 | ||||||
| 1–2 y | 18–155 | 7–54 a | 1700–11200 | ||||||
| 3–9 y | 6–85 | 5–80 b | 500–6500 | ||||||
| 10–14 y | 10–72 | 4–48 b | 500–3300 | ||||||
| Adults | |||||||||
| 8:00 am | 8–19 | 130–820 | 2–19 | 12–158 | < 10 | 9–58 | 167–5380 | ||
| 4:00 pm | 4–11 | 60–220 | |||||||
| Supine/upright | 4–21/5–46 | ND/<31 | |||||||
Data exist for the concentrations of a large number of steroid hormones throughout normal infancy, childhood, and adolescence (see Tables 14.2 and 14.3 ). Not all endocrine laboratories perform all of these assays, and, depending on the assay procedures used, various laboratories may have different “normal” values. Most central hospital and commercial laboratories are designed primarily to serve adult, rather than pediatric, patients. Thus it is important to know whether the available assays will be sufficiently sensitive with small volumes of blood to be useful in measuring pediatric values. This is especially true for the measurement of sex steroids (and gonadotropins), which can exhibit pathological elevations in children and still remain below the limit of detection of most “adult” assays. Efforts to achieve standardization of analytical methods and normative values are active topics in the field.
Measurement of the 24-hour urinary excretion of steroid metabolites, one of the oldest procedures for assessing adrenal function, has recently been revived by novel analytical mass spectrometric methods. Examination of total 24-hour urinary steroid excretion eliminates the diurnal fluctuations in serum steroid concentrations, and the variations attributable to episodic bursts of ACTH and transient stress (such as a visit to the clinic or difficult venipuncture). Collection of a complete 24-hour urine sample can be difficult in the infant or small child, hence urine should also be assayed for creatinine to monitor the completeness of the collection. Because of the diurnal and episodic nature of steroid secretion, one should never infer the 24-hour excretory rate from partial collections. This is important when assessing the absolute excretion rate of a single steroid, such as free cortisol. In contrast, a spot urine (preferably the first morning void, which is most concentrated and has been produced under peak ACTH stimulation), in which multiple excreted steroids are quantified in relation to creatinine, may suffice for qualitative pattern diagnostic of a specific steroid disorder.
Contemporary procedures for urinary steroid analysis use chromatography for separating steroids, followed by an MS detection method, usually GC-MS/MS, permitting very sensitive and specific assays of urinary steroids. However, each steroid is metabolized to multiple forms before being excreted in urine, and this metabolism can vary with age and sex in pediatric populations, so that the analyses are complex and require specialized expertise that is not yet widely available. Urinary free cortisol (UFC) measurements are highly reliable for diagnosing Cushing syndrome in adults. Excretion of UFC and of total cortisol metabolites is closely correlated with age, body surface area, and adiposity, but are typically 11 ± 5 μg/m 2 /day. Values vary substantially among different reference laboratories, reflecting variations in assay technologies, thus it is essential to use a laboratory with good data for normal children. It remains important to measure urinary creatinine to monitor the completeness of the collection.
Renin may be assayed by its enzymatic activity or by direct measurements of its concentration. Plasma renin activity (PRA) is simply an assay of the amount of angiotensin I generated per milliliter of serum, per hour at 37° C. In normal serum, the concentration of both renin and angiotensinogen (the renin substrate) are limiting. Another test, which is technically more challenging, directly measures plasma renin content (PRC) by immunoassay.
PRA is sensitive to dietary sodium intake, posture, diuretic therapy, activity, and sex steroids. Because PRA values can vary widely, it is best to measure PRA twice, once in the morning, after overnight supine posture, and then again after maintenance of upright posture for 4 hours. A simultaneous 24-hour urine for total sodium excretion is generally needed to interpret PRA results. Decreased dietary and urinary sodium, decreased intravascular volume, diuretics, and estrogens will increase PRA. Sodium loading, hyperaldosteronemia, and increased intravascular volume decrease PRA.
Renin measurements are used in the evaluation of hypertension and in the management of CAH. Assessment of the renin-angiotensin system is essential in children with simple virilizing (SV) CAH who lack clinical evidence of urinary salt loss (hyponatremia, hyperkalemia, acidosis, hypotension, shock), but who may nevertheless have increased PRA, especially when dietary sodium is restricted. This is a clinical sign that this form of 21OHD is simply a milder form of the more common salt-wasting form. Treatment of SV CAH with sufficient mineralocorticoid, to suppress PRA into the normal range, will reduce the child's requirement for glucocorticoids, thus maximizing final adult height and reducing exposure to excess glucocorticoids. Children with CAH need to have their mineralocorticoid replacement therapy monitored routinely by measuring PRA. Measurement of angiotensin II is also possible in some research laboratories, but most antibodies to angiotensin II strongly cross-react with angiotensin I. Thus PRA remains the usual way of evaluating the renin-angiotensin-aldosterone system.
Accurate immunoassay of plasma ACTH is available in most centers, but its measurement remains more difficult and variable than the assays for most other pituitary hormones. Handling of the samples must be done with care; samples must be drawn into a plastic syringe containing heparin or ethylenediamine tetraacetic acid (EDTA) and quickly transported in plastic tubes on ice, as ACTH adheres to glass and is quickly inactivated. Thus elevated plasma ACTH concentrations can be highly informative, but most assays cannot detect low or low-normal values, and such values can be spurious if the samples are handled badly. In adults and older children who have well-established diurnal rhythms of ACTH, normal 8 AM values rarely exceed 50 pg/mL, whereas 8 PM values are usually undetectable. Patients with Cushing disease often have normal morning values, but the diagnosis can be suggested by consistently elevated afternoon and evening values; patients with the ectopic ACTH syndrome can have values up to 1000 pg/mL.
The secretory rates of cortisol and aldosterone (or other steroids) can be measured by administering a small dose of tritiated cortisol or aldosterone and measuring the specific activity of one or more known metabolites in a 24-hour urine collection. This procedure permitted measurement of certain steroids, such as aldosterone, before specific immunoassays were available. These procedures have also provided much information about the normal rate of production of various steroids. Based on this procedure, most authorities have agreed that children and adults secrete about 6 to 9 mg of cortisol per square meter of body surface area per day.
Administration of dexamethasone, a potent synthetic glucocorticoid, will suppress secretion of pituitary ACTH and adrenal cortisol; the dexamethasone suppression test is useful for distinguishing whether glucocorticoid excess is caused primarily by pituitary disease or adrenal disease. As dexamethasone also suppresses adrenal androgen secretion, this test is useful for distinguishing between adrenal and gonadal sources of sex steroids. A complete formal dexamethasone suppression test requires the measurement of basal values and those obtained in response to both low- and high-dose dexamethasone. This is described in the section on the evaluation of Cushing syndrome. Variations of this test are commonly used, notably the single dose 1.0-mg in adults or 0.3 mg/m 2 in children. This is a useful outpatient screening procedure for distinguishing Cushing syndrome from exogenous obesity. It can be useful for the same purpose in adolescents and older children, but is otherwise of limited utility in pediatrics. An overnight high-dose dexamethasone suppression test is probably more reliable than the standard 2-day, high-dose test in differentiating adults with Cushing disease from those with the ectopic ACTH syndrome. However, the utility of this test in pediatric patients has not been established.
Direct stimulation of the adrenal with ACTH is a rapid, safe, easy way to evaluate adrenocortical function. The original ACTH test consisted of a 4- to 6-hour infusion of 0.5 units/kg of ACTH(1-39). This will maximally stimulate adrenal cortisol secretion, and thus effectively distinguishes primary adrenal insufficiency (Addison disease), in which the adrenal is incapable of responding, from secondary adrenal insufficiency caused by hypopituitarism. In secondary adrenal insufficiency, some steroidogenic capacity is present, therefore some cortisol is produced in response to the ACTH; thus cortisol secretion is less than normal but greater than the negligible values seen in primary adrenal insufficiency. The 4- to 6-hour intravenous ACTH test has been replaced by the 60-minute test, wherein a single bolus of ACTH(1-24) is administered intravenously and cortisol and possibly other steroids are measured at 0 and 60 minutes. Normal responses to a 60-minute test are shown in Table 14.4 . Synthetic ACTH(1-24) (cosyntropin) is preferred, as it has a more rapid action and shorter half-life than ACTH(1-39). The usual dose is 15 μg/kg in children up to 2 years of age, and 0.25 mg for children older than 2 years and adults. All of these doses are pharmacologic. A very-low-dose (1 μg) test may be useful in assessing adrenal recovery from glucocorticoid suppression. Newer data show that maximal steroidal responses can be achieved after only 30 minutes, but the best available standards are for a 60-minute test. One of the widest uses of intravenous ACTH tests in pediatrics is in diagnosing CAH. Stimulating the adrenal with ACTH increases steroidogenesis, resulting in accumulation of steroids proximal to the disordered enzyme. For example, inspection of Fig. 14.3 shows that impaired activity of P450c21 (21-hydroxylase) should lead to the accumulation of progesterone and 17OHP. However, progesterone does not accumulate in appreciable quantities, because it is converted to 17OHP. In routine practice, measuring the response of 17OHP to a 60-minute challenge, with intravenous ACTH, is the single most powerful and reliable means of diagnosing 21OHD; genetic testing can provide a useful confirmation. Comparing the patient's basal and ACTH-stimulated values of 17OHP against those from large numbers of well-studied patients usually permits the discrimination of normal persons, heterozygotes, patients with nonclassic CAH, and patients with classic CAH, although there inevitably is some overlap between groups ( Fig. 14.12 ). Measurement of testosterone or Δ 4 androstenedione in response to ACTH can distinguish normal persons from patients with classic CAH, but heterozygotes and patients with cryptic CAH have values overlapping both normal and classic CAH.
| 1–6 Months | 2–6 Years | Prepubertal | Adult Males | Adult Females | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unit | Basal | Stimulated | Basal | Stimulated | Basal | Stimulated | Basal | Stimulated | Basal | Stimulated | |
| Cortisol | μg/dL | 3–22 | 27–50 | 6–19 | 20–33 | 5–16 | 20–31 | 7–15 | 19–31 | 7–21 | 17–39 |
| 17OHP | ng/dL | 13–173 | 85–250 | 7–114 | 50–269 | 7–100 | 85–280 | 35–150 | 45–258 | 22–140 | 65–250 |
| 17OH Pregnenolone | ng/dL | 52–828 | 633–3286 | 10–103 | 45–347 | 10–186 | 70–656 | 20–187 | 240–1000 | 48–320 | 290–1382 |
| 11–Desoxycortisol | ng/dL | 10–200 | 101–392 | 7–210 | 95–323 | 14–136 | 95–254 | 20–65 | 73–214 | 15–158 | 65–237 |
| DOC | ng/dL | 7–48 | 40–158 | 4–49 | 26–139 | 4–17 | 22–120 | 3–13 | 14–38 | 3–19 | 12–90 |
| Pregnenolone | ng/dL | 10–150 | 100–359 | 17–50 | 34–99 | 15–63 | 39–130 | 10–85 | 20–200 | 46–150 | 70–220 |
| Δ4A | ng/dL | < 10–48 | < 10–87 | < 10 | < 10–35 | < 10 | < 10–69 | 50–210 | 78–285 | 61–222 | 98–295 |
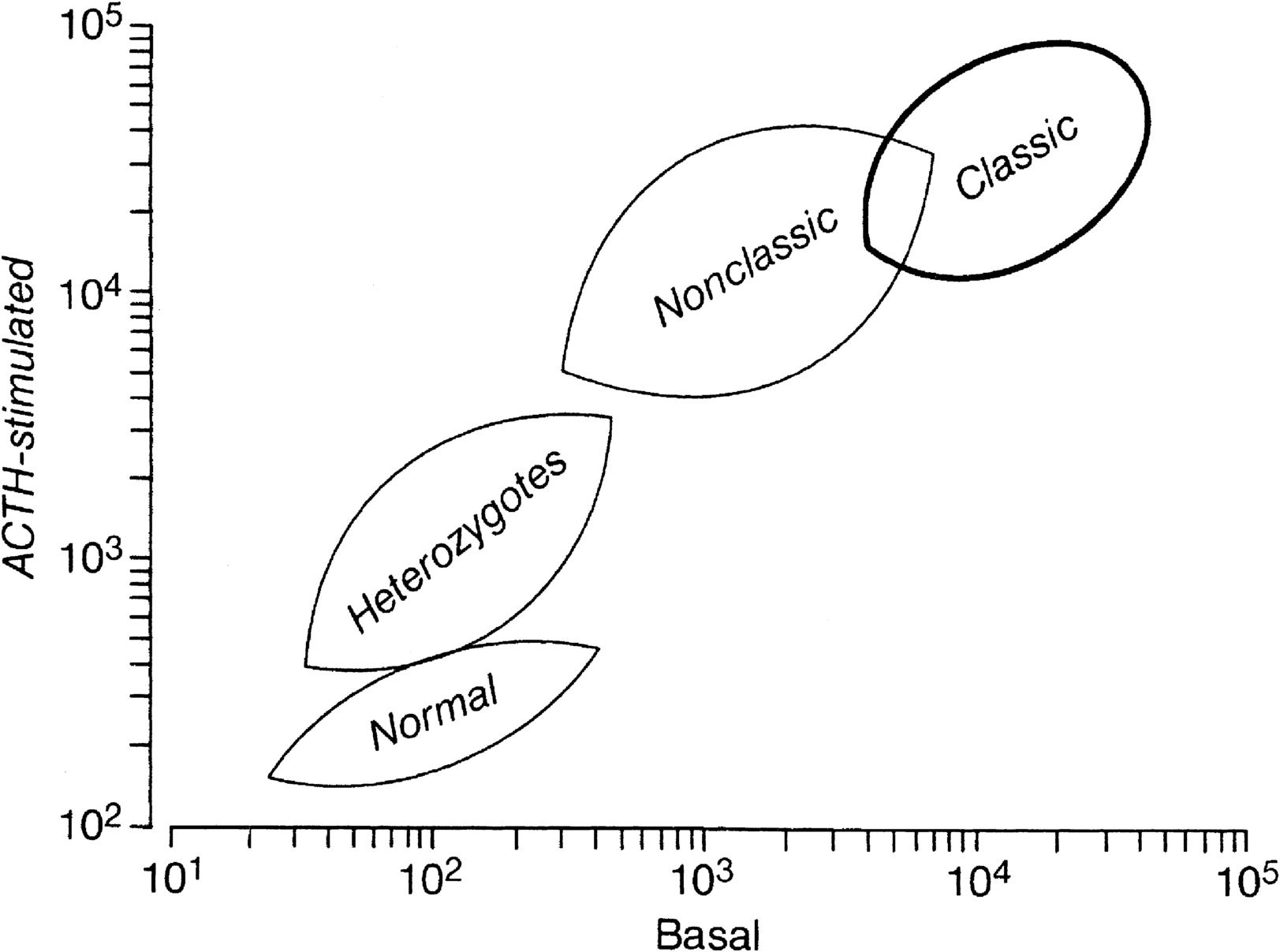
Longer ACTH tests of up to 3 days have also been used to evaluate adrenal function. It is important to remember that ACTH has both acute and chronic effects. Thus short tests measure only the acute effects of ACTH, that is, the maximal stimulation of preexisting steroidogenic machinery. In contrast, a 3-day test will examine the more chronic effects of ACTH to stimulate increased capacity for steroidogenesis by increasing the synthesis of steroidogenic machinery. Few situations exist where a 3-day intramuscular ACTH test is indicated, although it is occasionally useful in diagnosing the rare syndromes of hereditary unresponsiveness to ACTH.
Insulin-induced hypoglycemia is an effective but potentially risky test, and hence is rarely used. Insulin (0.1 U/kg/IV) is administered and blood is obtained at 0, 30, 45, and 60 minutes. The insulin-induced hypoglycemia will stimulate the release of “counterregulatory” hormones that have actions to increase plasma glucose concentrations: ACTH and cortisol, growth hormone, epinephrine, and glucagon. Because of the inherent risk of convulsions as a result of hypoglycemia, an experienced physician must be in attendance (not merely “available”) throughout the entire course of the test. Blood glucose must fall to half of the initial value or to 45 mg/dL to achieve an adequate test, and it is wise to terminate the test after this level is reached. Most patients will experience hunger, irritability, diaphoresis, and tachycardia; when these are followed by drowsiness or sleep, blood sugar levels are likely below acceptable limits. If this occurs, a blood sample should be obtained and 2 mL/kg of 20% to 25% glucose given intravenously, to a maximum of 100 mL.
Metyrapone blocks the action of P450c11β and, to a much lesser extent, P450scc. It is thus a chemical means of inducing a transient deficiency of 11-hydroxylase activity, which results in decreased cortisol secretion and subsequently increased ACTH secretion. Metyrapone testing is done to assess the capacity of the pituitary to produce ACTH in response to a physiologic stimulus. This test is useful in evaluating the hypothalamic-pituitary axis in the presence of central nervous system lesions, after neurosurgery, or long-term suppression by glucocorticoid therapy. Patients with a previous history of hypothalamic, pituitary, or adrenal disease, or those who have been withdrawn from glucocorticoid therapy should be reevaluated with a metyrapone test. A normal response indicates recovery of the HPA axis and predicts that the patient will respond normally to the stress of surgery.
Metyrapone is generally given orally as 300 mg/m 2 every 4 hours for a total of six doses (24 hours). Unlike many other drugs, it is appropriate to continue to increase the dose in older or overweight patients, but the total dose should not exceed 3.0 g. Blood should be obtained for cortisol, 11-deoxycortisol, and ACTH, before and after the test. In a normal response to metyrapone, cortisol decreases, ACTH increases, and 11-deoxycortisol (the substrate for P450c11β) increases greatly, to about 5 μg/dL. Adults and older children can be tested with the administration of a single oral dose of 30 mg/kg at midnight, given with food to reduce the gastrointestinal irritation. Blood samples are drawn at 8 AM the mornings before and after administering the drug.
Become a Clinical Tree membership for Full access and enjoy Unlimited articles
If you are a member. Log in here